Boxed Warning
Appropriate use:
Because midodrine can cause marked elevation of supine blood pressure, it should be used in patients whose lives are considerably impaired despite standard clinical care. The indication for use of midodrine in the treatment of symptomatic orthostatic hypotension is based primarily on a change in a surrogate marker of effectiveness, an increase in systolic blood pressure measured 1 minute after standing, a surrogate marker considered likely to correspond to a clinical benefit. At present, however, clinical benefits of midodrine, principally improved ability to carry out activities of daily living, have not been verified.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
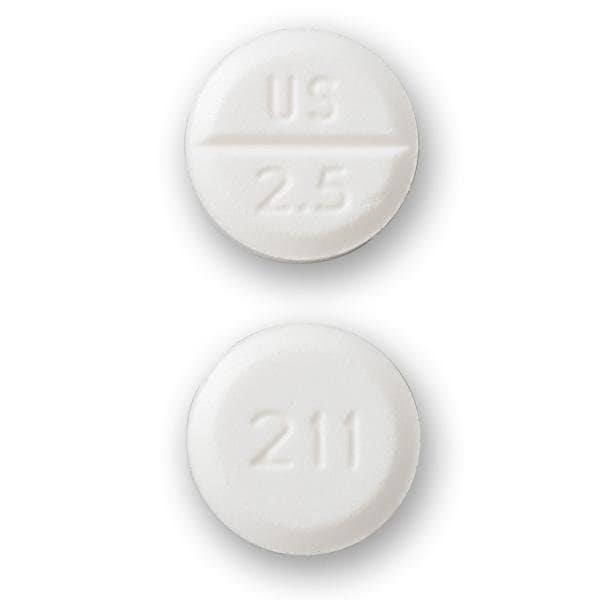
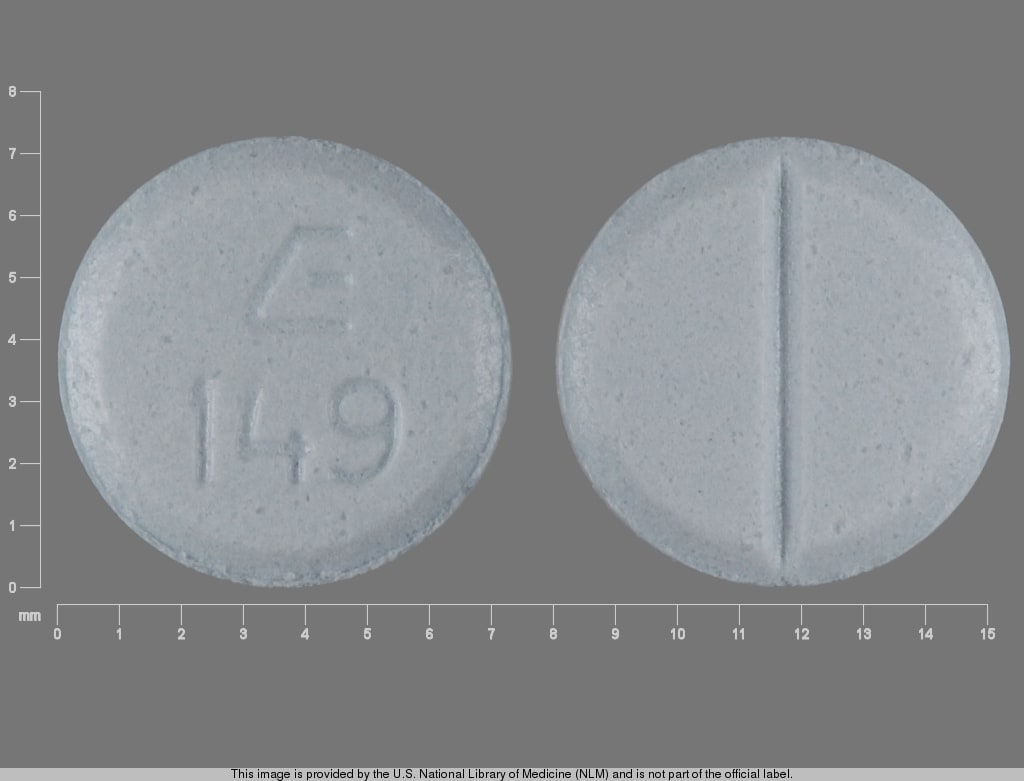
Tablet, Oral, as hydrochloride:
Generic: 2.5 mg, 5 mg, 10 mg
Pharmacology
Mechanism of Action
Midodrine forms an active metabolite, desglymidodrine, which is an alpha1-agonist. This agent increases arteriolar and venous tone resulting in a rise in standing, sitting, and supine systolic and diastolic blood pressure in patients with orthostatic hypotension.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Poorly crosses blood-brain barrier
Metabolism
Hepatic and many other tissues; midodrine is a prodrug which undergoes rapid deglycination to desglymidodrine (active metabolite)
Excretion
Urine (Midodrine: Insignificant; Desglymidodrine: 80% by active renal secretion)
Onset of Action
~1 hour
Time to Peak
Desglymidodrine: 1 to 2 hours; Midodrine: 30 minutes
Duration of Action
2 to 3 hours
Half-Life Elimination
Desglymidodrine: ~3 to 4 hours; Midodrine: 25 minutes
Protein Binding
Minimal
Use: Labeled Indications
Hypotension, symptomatic orthostatic: Treatment of symptomatic orthostatic hypotension.
Use: Off Label
Ascites, refractoryyes
Based on American Association for the Study of Liver Diseases (AASLD) clinical practice guidelines for the management of adult patients with ascites due to cirrhosis, midodrine, in addition to diuretics, should be considered for the management of refractory ascites, especially in hypotensive patients.
Hepatorenal Syndromebyes
Data from a small controlled trial in patients with type 1 hepatorenal syndrome treated with midodrine, octreotide, and albumin showed significant improvement in renal plasma flow, glomerular filtration rate, and urinary sodium excretion, although the trial included only 13 patients Angeli 1999. Retrospective data also suggest improvement in 30-day mortality with the combination of midodrine, octreotide, and albumin Esrailian 2007, Garcia-Tsao 2009.
Based on
Hypotension in the ICU, vasopressor sparingc
Data from one small prospective observational study and several retrospective, single center, observational studies suggest use of midodrine as adjunctive therapy to IV vasopressors in stable patients in the ICU may be beneficial to decrease the duration of IV vasopressor use and shorten ICU length of stay Levine 2013, Poveromo 2016, Rizvi 2018, Whitson 2016.
Hypotension, prevention of hemodialysis-inducedcyes
Data from several small studies (observational, retrospective, prospective, cross-over, or pre- and postintervention) have demonstrated intradialytic and postdialytic hemodynamic improvements (eg, systolic and diastolic blood pressures, MAP) compared to dialysis sessions without the use of midodrine Cruz 1998, Prakash 2004.
Based on the Kidney Disease Outcomes Quality Initiative (KDOQI) clinical practice guidelines for cardiovascular disease in dialysis patients, midodrine is effective and recommended in the prevention of or the amelioration of the symptoms and severity of dialysis-induced hypotension (also known as intradialytic hypotension).
Vasovagal syncopebyes
Data from two randomized, double-blind, placebo-controlled studies in a limited number of patients with frequent syncopal episodes who were not initially treated with nonpharmacologic therapy (eg, adequate fluid and salt intake, regular exercise, or physical counterpressure maneuvers) suggests that the use of midodrine may be beneficial in the treatment of vasovagal syncope Perez-Lugones 2001, Ward 1998. One randomized, double-blind, cross-over, placebo-controlled trial in patients who were refractory to nonpharmacologic therapy found no statistically significant difference between midodrine and placebo for vasovagal syncope recurrence although the follow-up period was only 3 months Romme 2011. Clinical experience also suggests the utility of midodrine as first-line pharmacologic therapy in the treatment of patients with vasovagal syncope who are refractory to nonpharmacologic therapy Schleifer 2015.
Based on the 2018 European Society of Cardiology (ESC) guidelines for the diagnosis and management of syncope, use of midodrine may be considered for treatment of patients with orthostatic form of vasovagal syncope.
Based on the 2017 American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS) guidelines for the evaluation and management of patients with syncope, midodrine may be used for treatment in patients with recurrent vasovagal syncope with no history of hypertension, heart failure, or urinary retention.
Contraindications
Severe organic heart disease; acute renal disease; urinary retention; pheochromocytoma; thyrotoxicosis; supine hypertension; poorly controlled hypertension.
Dosage and Administration
Dosing: Adult
Note: Standing systolic blood pressure may be elevated 15 to 30 mm Hg at 1 hour after a 10 mg dose. Some effect may persist for 2 to 3 hours.
Ascites, refractory (off-label use): Oral: 5 to 7.5 mg 3 times daily (AASLD [Runyon 2012]; Such 2019).
Hepatorenal syndrome (off-label use): Oral: Initial: 5 to 10 mg 3 times daily; may increase to maximum dose of 12.5 mg or 15 mg 3 times daily (with a goal to increase mean arterial pressure [MAP] by at least 15 mm Hg from baseline) (AASLD [Runyon 2012]; Angeli 1999; Esrailian 2007; Garcia-Tsao 2009).
Hypotension in the ICU, vasopressor sparing (off-label use): Oral: Initial: 5 to 20 mg 3 times daily; increase dose incrementally until IV vasopressors are discontinued (Levine 2013; Poveromo 2016; Rizvi 2018; Whitson 2016).
Hypotension, prevention of hemodialysis-induced (off-label use): Oral: 2.5 to 10 mg given 15 to 30 minutes prior to dialysis session (Cruz 1998; Flynn 1996; KDOQI 2005; Prakash 2004).
Hypotension, symptomatic orthostatic: Oral: 2.5 to 10 mg 3 times daily during daytime hours (every 3 to 4 hours) when patient is upright; maximum dose: 40 mg/day (ESC [Brignole 2018]; Kaufmann 2019). Note: Avoid administering <4 hours before bedtime to prevent supine hypertension; discontinue therapy if supine blood pressure increases excessively (Kaufmann 2019).
Vasovagal syncope (off-label use): Oral: Initial: 2.5 to 10 mg 3 times daily during daytime hours (every 6 hours) increased up to 15 mg per dose if necessary (ESC [Brignole 2018]; Perez-Lugones 2001; Ward 1998).
Dosing: Geriatric
Refer to adult dosing.
Administration
Oral: Doses may be given in approximately 3- to 4-hour intervals (eg, shortly before or upon rising in the morning, at midday, in the late afternoon not later than 6 PM). Avoid dosing after the evening meal or within 4 hours of bedtime to prevent supine hypertension.
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from light and moisture.
Midodrine Images
Drug Interactions
Alpha1-Blockers: May diminish the vasoconstricting effect of Alpha1-Agonists. Similarly, Alpha1-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Benzylpenicilloyl Polylysine: Alpha1-Agonists may diminish the diagnostic effect of Benzylpenicilloyl Polylysine. Management: Consider use of a histamine skin test as a positive control to assess a patient's ability to mount a wheal and flare response. Consider therapy modification
Bradycardia-Causing Agents: Midodrine may enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
Doxofylline: Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. Monitor therapy
Droxidopa: Midodrine may enhance the hypertensive effect of Droxidopa. Monitor therapy
Ergot Derivatives: May enhance the hypertensive effect of Alpha1-Agonists. Ergot Derivatives may enhance the vasoconstricting effect of Alpha1-Agonists. Exceptions: Ergoloid Mesylates; Nicergoline. Avoid combination
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Iobenguane Radiopharmaceutical Products: Alpha1-Agonists may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the hypertensive effect of Alpha1-Agonists. While linezolid is expected to interact via this mechanism, management recommendations differ from other monoamine oxidase inhibitors. Refer to linezolid specific monographs for details. Exceptions: Linezolid. Avoid combination
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Tricyclic Antidepressants: May enhance the therapeutic effect of Alpha1-Agonists. Tricyclic Antidepressants may diminish the therapeutic effect of Alpha1-Agonists. Monitor therapy
Adverse Reactions
>10%:
Cardiovascular: Supine hypertension (7% to 13%)
Central nervous system: Paresthesia (18%)
Dermatologic: Piloerection (13%), pruritus (12%)
Genitourinary: Dysuria (≤13%), urinary retention, urinary urgency
Renal: Polyuria
1% to 10%:
Central nervous system: Chills (5%), pain (5%)
Dermatologic: Skin rash (2%)
Gastrointestinal: Abdominal pain
<1%, postmarketing, and/or case reports: Anxiety, aphthous stomatitis, back pain, confusion, dizziness, drowsiness, erythema multiforme, facial flushing, flatulence, flushing, gastrointestinal distress, headache, heartburn, hyperesthesia, increased intracranial pressure, insomnia, leg cramps, nausea, visual field defect, weakness, xeroderma, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Bradycardia: May slow heart rate primarily due to vagal reflex. Use caution when administered concurrently with negative chronotropes (eg, digoxin, beta blockers). Discontinue use if signs or symptoms of bradycardia occur.
- Hypertension: May cause supine hypertension; discontinue use immediately if supine hypertension persists. Use with caution when administered concurrently with vasoconstrictors (eg, phenylephrine, ephedrine, dihydroergotamine, phenylpropanolamine, pseudoephedrine). Use is not recommended in patients with initial supine systolic pressure >180 mm Hg. Due to marked elevation of supine blood pressure (BP greater than 200 mm Hg systolic), use in patients whose lives are considerably impaired despite standard clinical care, including nonpharmacologic treatment (such as support stockings), fluid expansion, and lifestyle alterations. Supine and sitting blood pressure should be monitored.
Disease-related concerns:
- Diabetes: Use with caution in patients with diabetes mellitus.
- Hepatic impairment: Use with caution in patients with hepatic impairment; has not been studied.
- Renal impairment: Desglymidodrine, the active metabolite, is primarily renally excreted; assess renal function prior to initial dose; use with caution in patients with renal impairment (has not been studied) and initiate with a reduced dose; contraindicated in patients with acute renal failure.
- Visual problems: Use with caution in patients with visual problems, especially if receiving fludrocortisone.
Other warnings/precautions:
- Appropriate use: [US Boxed Warning]: Indicated for patients for whom orthostatic hypotension significantly impairs their daily life despite standard clinical care. Use is not recommended with supine hypertension. Continue therapy only in patients who appear to attain symptomatic improvement during initial treatment.
Monitoring Parameters
Blood pressure while supine, sitting, and standing upon awakening; renal and hepatic function.
Pregnancy
Pregnancy Considerations
Adverse events were observed in animal reproduction studies. Information related to the use of midodrine in pregnancy is limited (Glatter, 2005).
Patient Education
What is this drug used for?
- It is used to treat low blood pressure.
Frequently reported side effects of this drug
- Scalp tingling
- Itching
- Goose bumps
- Chills
- Passing a lot of urine
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes
- Severe dizziness
- Passing out
- Severe headache
- Vision changes
- Slow heartbeat
- Pounding in the ears
- Trouble urinating
- Burning or numbness feeling
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.