Boxed Warning
Cardiac effects:
Minoxidil may produce serious adverse effects. It can cause pericardial effusion, occasionally progressing to tamponade, and it can exacerbate angina pectoris. Reserve for hypertensive patients who do not respond adequately to maximum therapeutic doses of a diuretic and 2 other antihypertensive agents.
In experimental animals, minoxidil caused several kinds of myocardial lesions and other adverse cardiac effects.
Appropriate use:
Administer under close supervision, usually concomitantly with therapeutic doses of a beta-adrenergic blocking agent, to prevent tachycardia and increased myocardial workload. Usually, it must be given with a diuretic, frequently one acting in the ascending limb of the loop of Henle to prevent serious fluid accumulation. When first administering minoxidil, hospitalize and monitor patients with malignant hypertension and those already receiving guanethidine to avoid too rapid or large orthostatic decreases in blood pressure.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
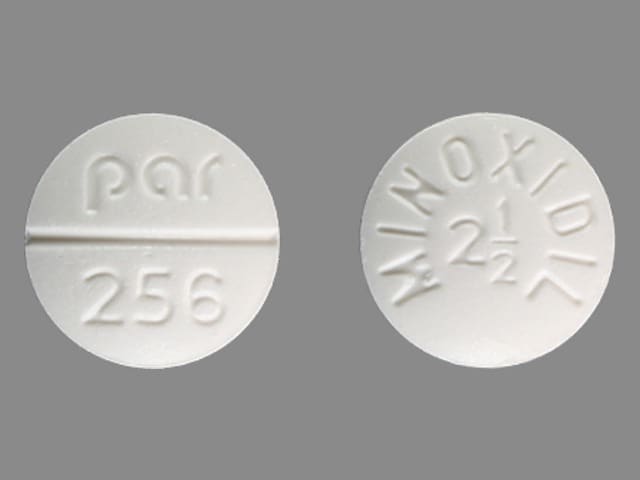
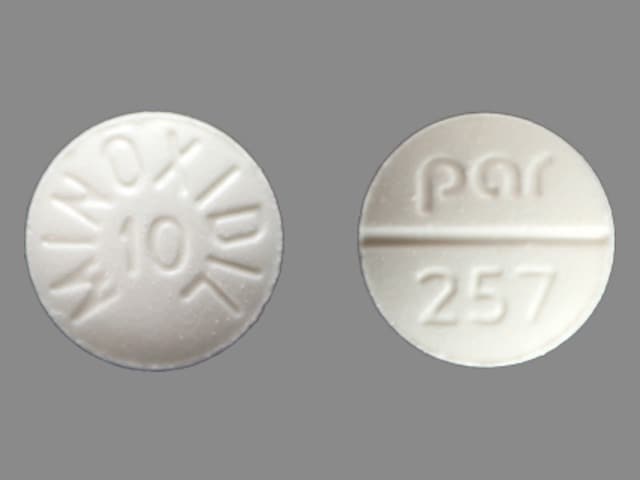
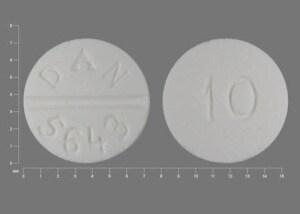
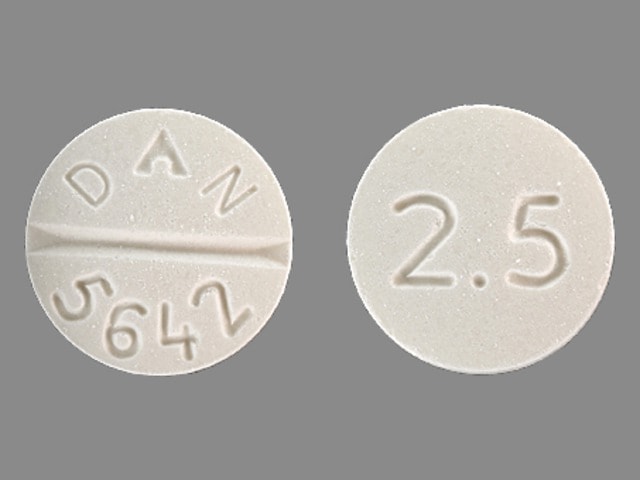
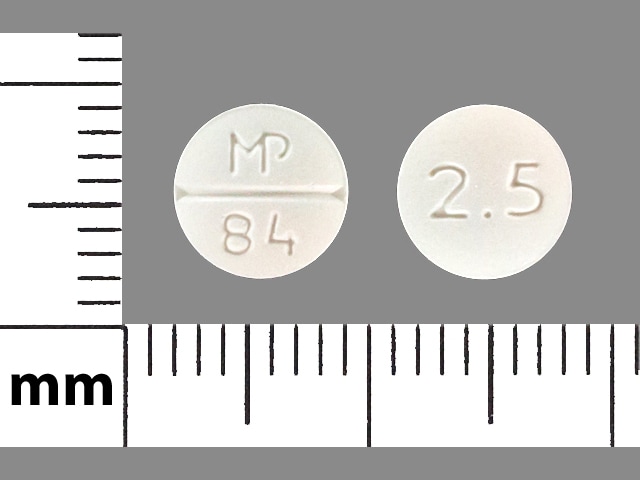
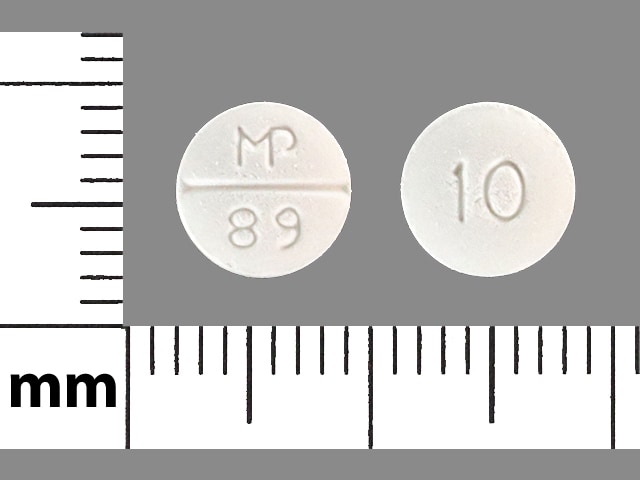
Tablet, Oral:
Generic: 2.5 mg, 10 mg
Pharmacology
Mechanism of Action
Produces vasodilation by directly relaxing arteriolar smooth muscle, with little effect on veins; effects may be mediated by cyclic AMP; stimulation of hair growth is secondary to vasodilation, increased cutaneous blood flow and stimulation of resting hair follicles
Pharmacokinetics/Pharmacodynamics
Metabolism
~90%, primarily via glucuronidation
Excretion
Urine (12% as unchanged drug)
Onset of Action
Hypotensive: ~30 minutes; Peak effect: 2 to 3 hours
Duration of Action
Up to 2 to 5 days
Half-Life Elimination
3.5 to 4.2 hours
Protein Binding
None
Use: Labeled Indications
Hypertension: Management of hypertension that is symptomatic or associated with target organ damage, and is not manageable with maximum therapeutic doses of a diuretic plus 2 other antihypertensives. Use in milder degrees of hypertension is not recommended because the benefit-risk ratio in such patients has not been defined. Note: Not recommended for the initial treatment of hypertension (ACC/AHA [Whelton 2017]).
Contraindications
Hypersensitivity to minoxidil or any component of the formulation; pheochromocytoma
Canadian labeling: Additional contraindications (not in US labeling): Pulmonary hypertension associated with mitral stenosis; severe hepatic impairment
Dosage and Administration
Dosing: Adult
Hypertension (alternative agent): Oral: Initial: 5 mg once daily, increase dose gradually in 1 to 3 divided doses every 3 days or more (or every 6 hours with careful monitoring if rapid management required) up to a maximum dose of 100 mg/day (ACC/AHA [Whelton 2017]).
Note: Dosage adjustment is needed when added to concomitant therapy. If supine diastolic pressure reduced <30 mm Hg, administer dose once daily; if supine diastolic pressure reduced >30 mm Hg, administer dose in 2 divided equal parts.
Dosing: Geriatric
Hypertension: Initial: 2.5 mg once daily; increase gradually (ASH/ISH [Weber 2014])
Dosing: Pediatric
Hypertension, severe; resistant to multiple drugs:
Children <12 years: Initial: 0.2 mg/kg/dose once daily; maximum initial dose: 5 mg/dose; titrate to effect, may increase daily dose by 50% to 100% every 3 days; may need to divide doses 1 to 3 times daily; usual effective dosage range: 0.25 to 1 mg/kg/day in 1 to 3 divided doses; maximum daily dose: 50 mg/day (NHLBI 2011; Park 2014); Note: In situations where rapid blood pressure management required, may increase dose every 6 hours with careful monitoring.
Children ≥12 years and Adolescents: Initial: 5 mg once daily, titrate to effect, may increase every 3 days by doubling daily dose (10 mg/day, 20 mg/day, and then 40 mg/day); may need to divide doses 1 to 3 times daily; usual effective daily dose range: 10 to 40 mg/day in 1 to 3 divided doses; maximum daily dose: 100 mg/day (NHLBI 2011; Park 2014); Note: In situations where rapid blood pressure management required, may increase dose every 6 hours with careful monitoring.
Storage
Store between 20°C and 25°C (68°F and 77°F).
Minoxidil (Systemic) Images
Drug Interactions
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Atazanavir: May increase the serum concentration of Minoxidil (Systemic). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
CycloSPORINE (Systemic): May enhance the adverse/toxic effect of Minoxidil (Systemic). Severe hypertrichosis has been reported. Monitor therapy
Dapoxetine: May enhance the orthostatic hypotensive effect of Minoxidil (Systemic). Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Probenecid: May increase the serum concentration of Minoxidil (Systemic). Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Valproate Products: May increase the serum concentration of Minoxidil (Systemic). Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Adverse Reactions
Frequency not always defined.
Cardiovascular: ECG changes (T-wave changes 60%), edema (reversible, 7% to 10%), pericardial effusion (occasionally with tamponade, 3%), angina pectoris, cardiac failure, pericarditis, tachycardia
Dermatologic: Hypertrichosis (80%), bullous rash (rare), skin rash, Stevens-Johnson syndrome (rare), toxic epidermal necrolysis
Endocrine & metabolic: Sodium retention, water retention, weight gain
Gastrointestinal: Nausea, vomiting
Hematologic & oncologic: Decreased hematocrit (transient, hemodilution), decreased red blood cells (transient, hemodilution), hemoglobin (transient, hemodilution), leukopenia (rare), thrombocytopenia (rare)
Hepatic: Ascites, increased serum alkaline phosphatase
Renal: Increased blood urea nitrogen (transient), increased serum creatinine (transient)
Respiratory: Pulmonary edema (Lee 2011)
<1%, postmarketing, and/or case reports: Breast tenderness (rare)
Warnings/Precautions
Concerns related to adverse effects:
- Fluid retention: May cause salt and water retention; administer with a diuretic, preferably a loop diuretic (eg, furosemide) to prevent fluid retention and subsequent local and generalized edema. Use with extreme caution in patients with heart failure.
- Pericardial effusion/tamponade: [US Boxed Warning]: May cause pericarditis and pericardial effusion that may progress to tamponade; patients with renal impairment not on dialysis may be at higher risk. Use with caution in patients with heart failure; observe patients closely. If effusion persists, consider discontinuation of minoxidil.
- Rapid blood pressure control: Rapid control of blood pressure in patients with severe hypertension can lead to syncope, cerebrovascular accidents, MI, and/or ischemia of other special sense organs resulting in decrease or loss of vision or hearing. Patients with compromised circulation or cryoglobulinemia may also suffer ischemic episodes of the affected organs.
- Sinus tachycardia: [US Boxed Warning]: May increase oxygen demand and exacerbate angina pectoris; concomitant use with a beta-blocker (if no contraindication exists) may help reduce the effect. Use with caution in patients with ischemic heart disease.
Disease-related concerns:
- Acute myocardial infarct (MI): Avoid use for a month after acute MI as use may increase oxygen demand due to reflex tachycardia. Use with extreme caution; ensure patient is receiving a beta blocker prior to initiation.
- Heart failure: Compared to placebo minoxidil increased the frequency of clinical events, including increased need for diuretics, angina, ventricular arrhythmias, worsening heart failure and death (Franciosa 1984). In a scientific statement from the American Heart Association, minoxidil has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: moderate) (AHA [Page 2016]).
- Renal impairment: Use with caution in patients with significant renal impairment; renal failure and dialysis patients may require a smaller dose. Monitor closely to prevent exacerbation of renal failure.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in the elderly; initiate at the low end of the dosage range and monitor closely.
Other warnings/precautions:
- Appropriate use: [US Boxed Warning]: Maximum therapeutic doses of a diuretic and two other antihypertensives should be used before this drug is ever added. Should be given with a diuretic to minimize fluid gain and a beta-blocker (if no contraindications) to prevent tachycardia and increased myocardial workload. Patients with malignant hypertension and those already receiving guanethidine should be hospitalized with close medical supervision to ensure blood pressure is reducing and to prevent too rapid of a reduction in blood pressure.
Monitoring Parameters
Blood pressure, standing and sitting/supine; signs/symptoms of pericardial effusion; fluid and electrolyte balance and body weight should be monitored. Any tests that are abnormal at the time of initiation (including, renal function tests, ECG, echocardiogram, chest x-ray) should be repeated initially every 1 to 3 months then every 6 to 12 months once stable.
The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year ASCVD risk ≥10%: Target blood pressure <130/80 mm Hg is recommended
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events were observed in some animal studies. Neonatal hypertrichosis has been reported following exposure to minoxidil during pregnancy.
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Hair growth
- Vomiting
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Shortness of breath
- Chest pain
- Arm pain
- Shoulder pain
- Fast heartbeat
- Dizziness
- Passing out
- Abnormal heartbeat
- Severe or persistent heartburn
- Difficulty breathing
- Trouble hearing
- Vision changes
- Weight gain
- Edema
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.