Boxed Warning
Cardiovascular thrombotic events:
NSAIDs cause an increased risk of serious cardiovascular thrombotic events, including MI and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use.
Naproxen/esomeprazole is contraindicated in the setting of CABG surgery.
GI bleeding, ulceration, and perforation:
NSAIDs cause an increased risk of serious GI adverse events, including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet Delayed Release, Oral:
Vimovo: Naproxen [delayed release] 375 mg and esomeprazole [immediate release] 20 mg, Naproxen [delayed release] 500 mg and esomeprazole [immediate release] 20 mg [contains methylparaben, propylparaben]
Pharmacology
Mechanism of Action
Naproxen: Reversibly inhibits cyclooxygenase-1 and 2 (COX-1 and 2) enzymes, which result in decreased formation of prostaglandin precursors; has antipyretic, analgesic, and anti-inflammatory properties
Esomeprazole: Proton pump inhibitor which decreases acid secretion in gastric parietal cells
Use: Labeled Indications
Osteoarthritis, rheumatoid arthritis, ankylosing spondylitis: Reduction of the risk of NSAID-associated gastric ulcers in patients at risk of developing gastric ulcers who require an NSAID for the relief of signs and symptoms of osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis in adults.
Juvenile idiopathic arthritis: Reduction of the risk of NSAID-associated gastric ulcers in patients at risk of developing gastric ulcers who require an NSAID for the relief of signs and symptoms of juvenile idiopathic arthritis (JIA) in pediatric patients ≥12 years weighing ≥38 kg.
Limitations of use: Not recommended for the initial treatment of pain; controlled studies do not extend beyond 6 months.
Contraindications
Hypersensitivity (eg, anaphylactic reactions, serious skin reactions) to naproxen, esomeprazole, other substituted benzimidazoles, omeprazole, or any component of the formulation; use in the setting of CABG surgery; history of asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs; coadministration with rilpivirine-containing products.
Canadian labeling: Additional contraindications (not in US labeling): Severe uncontrolled heart failure; active gastric/duodenal/peptic ulcer or active GI bleeding; cerebrovascular bleeding or other bleeding disorders; inflammatory bowel disease; severe liver impairment or active liver disease; severe renal impairment (creatinine clearance <30 mL/minute) or deteriorating renal disease; known hyperkalemia; use during the third trimester of pregnancy; breastfeeding; use in patients <18 years; concomitant use of rilpivirine
Dosage and Administration
Dosing: Adult
Osteoarthritis, rheumatoid arthritis, ankylosing spondylitis: Oral: One tablet (naproxen 375 mg/esomeprazole 20 mg or naproxen 500 mg/esomeprazole 20 mg) twice daily
Note: If a total daily dose of esomeprazole <40 mg is necessary, alternate treatment should be considered.
Dosing: Geriatric
Use lowest effective dose. Refer to adult dosing.
Dosing: Pediatric
Juvenile idiopathic arthritis: Children and Adolescents ≥12 years and weight ≥38 kg: Oral:
38 to <50 kg: One tablet (naproxen 375 mg/esomeprazole 20 mg) twice daily
>50 kg: One tablet (naproxen 375 mg/esomeprazole 20 mg or naproxen 500 mg/esomeprazole 20 mg) twice daily
Note: If a total daily dose of esomeprazole <40 mg is necessary, alternate treatment should be considered.
Administration
Administer dose at least 30 minutes prior to meals. Swallow tablets whole; do not chew, crush, dissolve, or split.
Do not substitute naproxen/esomeprazole with single-ingredient products of naproxen and esomeprazole magnesium.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Store in original container. Protect from moisture.
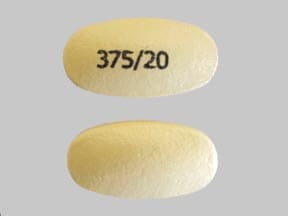
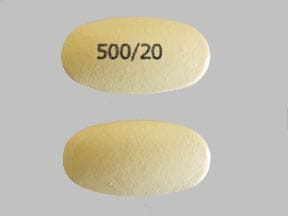
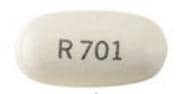
Naproxen and Esomeprazole Images
-
esomeprazole/naproxen esomeprazole magnesium 20 mg / naproxen 375 mg -
esomeprazole/naproxen esomeprazole magnesium 20 mg / naproxen 500 mg -

esomeprazole/naproxen 20 mg esomeprazole magnesium / 375 mg naproxen -
esomeprazole/naproxen 20 mg esomeprazole magnesium / 500 mg naproxen -

esomeprazole/naproxen 20 mg / 375 mg -
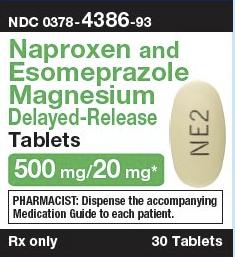
esomeprazole/naproxen 20 mg / 500 mg
Drug Interactions
5-Aminosalicylic Acid Derivatives: Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of 5-Aminosalicylic Acid Derivatives. Monitor therapy
Acalabrutinib: Proton Pump Inhibitors may decrease the serum concentration of Acalabrutinib. Avoid combination
Acemetacin: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the risk of GI bleeding may be increased with this combination. Monitor therapy
Aliskiren: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Aliskiren. Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Aliskiren. Management: Monitor renal function periodically in patients receiving aliskiren and any nonsteroidal anti-inflammatory agent. Patients at elevated risk of renal dysfunction include those who are elderly, are volume depleted, or have pre-existing renal dysfunction. Monitor therapy
Aminoglycosides: Nonsteroidal Anti-Inflammatory Agents may decrease the excretion of Aminoglycosides. Data only in premature infants. Monitor therapy
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Amphetamine: Proton Pump Inhibitors may increase the absorption of Amphetamine. Monitor therapy
Angiotensin II Receptor Blockers: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Angiotensin II Receptor Blockers. The combination of these two agents may also significantly decrease glomerular filtration and renal function. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Apixaban: Naproxen may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Naproxen may increase the serum concentration of Apixaban. Consider therapy modification
Atazanavir: Proton Pump Inhibitors may decrease the serum concentration of Atazanavir. Management: See full drug interaction monograph for details. Consider therapy modification
Bemiparin: Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin and nonsteroidal anti-inflammatory agents (NSAIDs) due to the increased risk of bleeding. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Beta-Blockers: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Beta-Blockers. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Nonsteroidal Anti-Inflammatory Agents. Consider therapy modification
Bisphosphonate Derivatives: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Bisphosphonate Derivatives. Both an increased risk of gastrointestinal ulceration and an increased risk of nephrotoxicity are of concern. Monitor therapy
Bisphosphonate Derivatives: Proton Pump Inhibitors may diminish the therapeutic effect of Bisphosphonate Derivatives. Monitor therapy
Bosutinib: Proton Pump Inhibitors may decrease the serum concentration of Bosutinib. Management: Consider alternatives to proton pump inhibitors, such as short-acting antacids or histamine-2 receptor antagonists. Administer alternative agents more than 2 hours before or after bosutinib. Consider therapy modification
Capecitabine: Proton Pump Inhibitors may diminish the therapeutic effect of Capecitabine. Monitor therapy
Cefditoren: Proton Pump Inhibitors may decrease the serum concentration of Cefditoren. Management: If possible, avoid use of cefditoren with proton pump inhibitors (PPIs). Consider alternative methods to minimize/control acid reflux (eg, diet modification) or alternative antimicrobial therapy if use of PPIs can not be avoided. Consider therapy modification
Cefpodoxime: Proton Pump Inhibitors may decrease the serum concentration of Cefpodoxime. Monitor therapy
Cefuroxime: Proton Pump Inhibitors may decrease the absorption of Cefuroxime. Avoid combination
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Cilostazol: Esomeprazole may increase serum concentrations of the active metabolite(s) of Cilostazol. Esomeprazole may increase the serum concentration of Cilostazol. Monitor therapy
Clopidogrel: Esomeprazole may diminish the antiplatelet effect of Clopidogrel. Esomeprazole may decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Clopidogrel prescribing information recommends avoiding concurrent use with esomeprazole. Rabeprazole or pantoprazole may be lower-risk alternatives to esomeprazole. Consider therapy modification
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Corticosteroids (Systemic): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Monitor therapy
CycloSPORINE (Systemic): Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of CycloSPORINE (Systemic). Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of CycloSPORINE (Systemic). CycloSPORINE (Systemic) may increase the serum concentration of Nonsteroidal Anti-Inflammatory Agents. Management: Consider alternatives to nonsteroidal anti-inflammatory agents (NSAIDs). Monitor for evidence of nephrotoxicity, as well as increased serum cyclosporine concentrations and systemic effects (eg, hypertension) during concomitant therapy with NSAIDs. Consider therapy modification
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Inducers (Strong): May increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Cysteamine (Systemic): Proton Pump Inhibitors may diminish the therapeutic effect of Cysteamine (Systemic). Monitor therapy
Dabigatran Etexilate: Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Dabigatran Etexilate. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of dabigatran and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dacomitinib: Proton Pump Inhibitors may decrease the serum concentration of Dacomitinib. Management: Avoid concurrent use of dacomitinib with proton pump inhibitors. Antacids may be used. Histamine H2-receptor antagonists (HR2A) may be used if dacomitinib is given at least 6 hours before or 10 hours after the H2RA. Avoid combination
Dasatinib: Proton Pump Inhibitors may decrease the serum concentration of Dasatinib. Management: Antacids (taken 2 hours before or after dasatinib administration) can be used in place of the proton pump inhibitor if some acid-reducing therapy is needed. Avoid combination
Deferasirox: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Delavirdine: Proton Pump Inhibitors may decrease the serum concentration of Delavirdine. Management: Chronic therapy with proton pump inhibitors (PPIs) should be avoided in patients treated with delavirdine. The clinical significance of short-term PPI therapy with delavirdine is uncertain, but such therapy should be undertaken with caution. Avoid combination
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Desmopressin: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dexibuprofen: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Dexibuprofen. Avoid combination
Dexketoprofen: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Dexmethylphenidate: Proton Pump Inhibitors may increase the absorption of Dexmethylphenidate. Specifically, proton pump inhibitors may interfere with the normal release of drug from the extended-release capsules (Focalin XR brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Dextroamphetamine: Proton Pump Inhibitors may increase the absorption of Dextroamphetamine. Specifically, the dextroamphetamine absorption rate from mixed amphetamine salt extended release (XR) capsules may be increased in the first hours after dosing. Monitor therapy
Dichlorphenamide: OAT1/3 Inhibitors may increase the serum concentration of Dichlorphenamide. Monitor therapy
Diclofenac (Systemic): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Management: Seek alternatives to the combined use of diclofenac with other nonsteroidal anti-inflammatory agents (NSAIDs). Avoid the use of diclofenac/misoprostol with other NSAIDs. Consider therapy modification
Digoxin: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Digoxin. Monitor therapy
Doxycycline: Proton Pump Inhibitors may decrease the bioavailability of Doxycycline. Monitor therapy
Drospirenone: Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Drospirenone. Monitor therapy
Edoxaban: Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of edoxaban and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. Consider therapy modification
Enoxaparin: Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue nonsteroidal anti-inflammatory agents (NSAIDs) prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Conversely, concentrations of active metabolites may be increased for those drugs activated by CYP2C19. Management: Concurrent use of enzalutamide with CYP2C19 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C19 substrate should be performed with caution and close monitoring. Consider therapy modification
Eplerenone: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Eplerenone. Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Eplerenone. Monitor therapy
Erlotinib: Proton Pump Inhibitors may decrease the serum concentration of Erlotinib. Avoid combination
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Felbinac: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Floctafenine: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Fluconazole: May increase the serum concentration of Proton Pump Inhibitors. Monitor therapy
Gefitinib: Proton Pump Inhibitors may decrease the serum concentration of Gefitinib. Management: Avoid use of proton pump inhibitors (PPIs) with gefitinib when possible. If required, administer gefitinib 12 hours after administration of the PPI or 12 hours before the next dose of the PPI. Consider therapy modification
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Haloperidol: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Haloperidol. Specifically including drowsiness and confusion. Monitor therapy
Heparin: Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or nonsteroidal anti-inflammatory agents (NSAIDs) if coadministration is required. Consider therapy modification
Heparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or agents with antiplatelet properties if coadministration is required. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Bleeding may occur. Management: Concomitant treatment with these agents should generally be avoided. If used concomitantly, increased diligence in monitoring for adverse effects (eg, bleeding, bruising, altered mental status due to CNS bleeds) must be employed. Consider therapy modification
HydrALAZINE: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of HydrALAZINE. Monitor therapy
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Indinavir: Proton Pump Inhibitors may decrease the serum concentration of Indinavir. Monitor therapy
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Iron Preparations: Proton Pump Inhibitors may decrease the absorption of Iron Preparations. Exceptions: Ferric Carboxymaltose; Ferric Citrate; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Monitor therapy
Itraconazole: Proton Pump Inhibitors may increase the serum concentration of Itraconazole. Proton Pump Inhibitors may decrease the serum concentration of Itraconazole. Management: Exposure to Tolsura brand itraconazole may be increased by PPIs; consider itraconazole dose reduction. Exposure to Sporanox brand itraconazole capsules may be decreased by PPIs. Give Sporanox brand itraconazole at least 2 hrs before or 2 hrs after PPIs Consider therapy modification
Ketoconazole (Systemic): Proton Pump Inhibitors may decrease the absorption of Ketoconazole (Systemic). Ketoconazole (Systemic) may increase the serum concentration of Proton Pump Inhibitors. Management: Administer ketoconazole with an acidic beverage, such as non-diet cola, to increase gastric acidity and improve absorption if concomitant use with proton pump inhibitors is necessary. Consider therapy modification
Ketorolac (Nasal): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Ketorolac (Systemic): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Ledipasvir: Proton Pump Inhibitors may decrease the serum concentration of Ledipasvir. Management: PPI doses equivalent to omeprazole 20 mg or lower may be given with ledipasvir under fasted conditions. Administration with higher doses of PPIs, 2 hours after a PPI, or in combination with food and PPIs may reduce ledipasvir bioavailability. Consider therapy modification
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Lithium: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Lithium. Consider therapy modification
Loop Diuretics: Nonsteroidal Anti-Inflammatory Agents may diminish the diuretic effect of Loop Diuretics. Loop Diuretics may enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Management: Monitor for evidence of kidney injury or decreased therapeutic effects of loop diuretics with concurrent use of an NSAID. Consider avoiding concurrent use in CHF or cirrhosis. Concomitant use of bumetanide with indomethacin is not recommended. Consider therapy modification
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of Proton Pump Inhibitors. Monitor therapy
Macimorelin: Nonsteroidal Anti-Inflammatory Agents may diminish the diagnostic effect of Macimorelin. Avoid combination
Mesalamine: Proton Pump Inhibitors may diminish the therapeutic effect of Mesalamine. Proton pump inhibitor-mediated increases in gastrointestinal pH may cause the premature release of mesalamine from specific sustained-release mesalamine products. Management: Consider avoiding concurrent administration of high-dose proton pump inhibitors (PPIs) with sustained-release mesalamine products. Consider therapy modification
MetFORMIN: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of MetFORMIN. Monitor therapy
Methotrexate: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Methotrexate. Management: Alternative anti-inflammatory therapy should be considered whenever possible, especially if the patient is receiving higher, antineoplastic doses of methotrexate. Consider therapy modification
Methylphenidate: Proton Pump Inhibitors may increase the absorption of Methylphenidate. Specifically, proton pump inhibitors may interfere with the normal release of drug from the extended-release capsules (Ritalin LA brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Mifamurtide: Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Mifamurtide. Avoid combination
Morniflumate: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): Proton Pump Inhibitors may decrease the serum concentration of Multivitamins/Minerals (with ADEK, Folate, Iron). Specifically, the absorption of iron may be decreased. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Mycophenolate: Proton Pump Inhibitors may decrease the serum concentration of Mycophenolate. Specifically, concentrations of the active mycophenolic acid may be reduced. Monitor therapy
Naftazone: May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Nelfinavir: Proton Pump Inhibitors may decrease serum concentrations of the active metabolite(s) of Nelfinavir. Proton Pump Inhibitors may decrease the serum concentration of Nelfinavir. Avoid combination
Neratinib: Proton Pump Inhibitors may decrease the serum concentration of Neratinib. Specifically, proton pump inhibitors may reduce neratinib absorption. Avoid combination
Nilotinib: Proton Pump Inhibitors may decrease the serum concentration of Nilotinib. Management: Avoid this combination when possible since separation of doses is not likely to be an adequate method of minimizing the interaction. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Avoid combination
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omacetaxine: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Omacetaxine. Specifically, the risk for bleeding-related events may be increased. Management: Avoid concurrent use of nonsteroidal antiinflammatory drugs (NSAIDs) with omacetaxine in patients with a platelet count of less than 50,000/uL. Avoid combination
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
PAZOPanib: Proton Pump Inhibitors may decrease the serum concentration of PAZOPanib. Avoid combination
Pelubiprofen: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Pexidartinib: Proton Pump Inhibitors may decrease the serum concentration of Pexidartinib. Management: If acid-reduction is needed, consider administering an antacid 2 hours before or after pexidartinib, or administer pexidartinib 2 hours before or 10 hours after an H2 receptor antagonist. Avoid combination
Phenylbutazone: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Posaconazole: Proton Pump Inhibitors may decrease the serum concentration of Posaconazole. Consider therapy modification
Potassium-Sparing Diuretics: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Potassium-Sparing Diuretics. Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
PRALAtrexate: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of PRALAtrexate. More specifically, NSAIDS may decrease the renal excretion of pralatrexate. Management: Closely monitor for increased pralatrexate serum levels and/or toxicity if used concomitantly with an NSAID. Monitor for decreased pralatrexate serum levels with NSAID discontinuation. Monitor therapy
Probenecid: May increase the serum concentration of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Prostaglandins (Ophthalmic): Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Prostaglandins (Ophthalmic). Nonsteroidal Anti-Inflammatory Agents may also enhance the therapeutic effects of Prostaglandins (Ophthalmic). Monitor therapy
Quinolones: Nonsteroidal Anti-Inflammatory Agents may enhance the neuroexcitatory and/or seizure-potentiating effect of Quinolones. Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Quinolones. Monitor therapy
Raltegravir: Proton Pump Inhibitors may increase the serum concentration of Raltegravir. Monitor therapy
RifAMPin: May decrease the serum concentration of Esomeprazole. Avoid combination
Rilpivirine: Proton Pump Inhibitors may decrease the serum concentration of Rilpivirine. Avoid combination
Riociguat: Proton Pump Inhibitors may decrease the serum concentration of Riociguat. Monitor therapy
Risedronate: Proton Pump Inhibitors may diminish the therapeutic effect of Risedronate. Proton Pump Inhibitors may increase the serum concentration of Risedronate. This applies specifically to use of delayed-release risedronate. Consider therapy modification
Rivaroxaban: Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: A comprehensive risk to benefit assessment should be done for all patients before any concurrent use of rivaroxaban and nonsteroidal anti-inflammatory drugs (NSAIDs). If combined, monitor patients extra closely for signs and symptoms of bleeding. Consider therapy modification
Salicylates: Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the adverse/toxic effect of Salicylates. An increased risk of bleeding may be associated with use of this combination. Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the cardioprotective effect of Salicylates. Salicylates may decrease the serum concentration of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Exceptions: Choline Magnesium Trisalicylate. Consider therapy modification
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Saquinavir: Proton Pump Inhibitors may increase the serum concentration of Saquinavir. Monitor therapy
Secretin: Proton Pump Inhibitors may diminish the diagnostic effect of Secretin. Specifically, use of PPIs may cause a hyperresponse in gastrin secretion in response to secretin stimulation testing, falsely suggesting gastrinoma. Management: Avoid concomitant use of proton pump inhibitors (PPIs) and secretin, and discontinue PPIs several weeks prior to secretin administration, with the duration of separation determined by the specific PPI. See full monograph for details. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Management: Consider alternatives to NSAIDs. Monitor for evidence of bleeding and diminished antidepressant effects. It is unclear whether COX-2-selective NSAIDs reduce risk. Consider therapy modification
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sodium Phosphates: May enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with NSAIDs, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, maintain adequate hydration and monitor renal function closely. Consider therapy modification
SORAfenib: Proton Pump Inhibitors may decrease the absorption of SORAfenib. Monitor therapy
St John's Wort: May decrease the serum concentration of Esomeprazole. Avoid combination
Tacrolimus (Systemic): Proton Pump Inhibitors may increase the serum concentration of Tacrolimus (Systemic). Management: Tacrolimus dose adjustment may be required. Rabeprazole, pantoprazole, or selected H2-receptor antagonists (i.e., ranitidine or famotidine) may be less likely to interact. Genetic testing may predict patients at highest risk. Consider therapy modification
Talniflumate: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Tenofovir Products: Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Tenofovir Products. Management: Seek alternatives to these combinations whenever possible. Avoid use of tenofovir with multiple NSAIDs or any NSAID given at a high dose. Consider therapy modification
Tenoxicam: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Thiazide and Thiazide-Like Diuretics: May enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Tipranavir: May decrease the serum concentration of Proton Pump Inhibitors. These data are derived from studies with Ritonavir-boosted Tipranavir. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Tolperisone: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Tolperisone. Specifically, the risk of hypersensitivity reactions may be increased. Tolperisone may enhance the therapeutic effect of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Tricyclic Antidepressants (Tertiary Amine): May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Vancomycin: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Vancomycin. Monitor therapy
Velpatasvir: Proton Pump Inhibitors may decrease the serum concentration of Velpatasvir. Avoid combination
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Nonsteroidal Anti-Inflammatory Agents (Nonselective) may enhance the anticoagulant effect of Vitamin K Antagonists. Management: Consider alternatives to this combination when possible. If the combination must be used, monitor coagulation status closely and advise patients to promptly report any evidence of bleeding or bruising. Consider therapy modification
Voriconazole: May increase the serum concentration of Proton Pump Inhibitors. Proton Pump Inhibitors may increase the serum concentration of Voriconazole. Monitor therapy
Zaltoprofen: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Test Interactions
See individual agents.
Adverse Reactions
Also see individual agents.
>10%: Gastrointestinal: Gastritis (17%)
1% to 10%:
Cardiovascular: Peripheral edema (3%)
Central nervous system: Dizziness (3%), headache (3%)
Gastrointestinal: Diarrhea (6%), constipation (4%), flatulence (4%), upper abdominal pain (4%), dysgeusia (2%)
Genitourinary: Urinary tract infection (2%)
Respiratory: Upper respiratory tract infection (5%)
<1%, postmarketing and/or case reports: Abdominal distention, abdominal pain, abnormal gait, acute interstitial nephritis, bruise, falling, gastroesophageal reflux disease, hematochezia, joint swelling, muscle spasm, renal tubular necrosis
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylactoid reactions: Even in patients without prior exposure anaphylactoid reactions may occur; patients with "aspirin triad" (bronchial asthma, aspirin intolerance, rhinitis) may be at increased risk. Contraindicated in patients who experience bronchospasm, asthma, rhinitis, or urticaria with nonsteroidal anti-inflammatory drug (NSAID) or aspirin therapy.
- Carcinoma: No occurrences of enterochromaffin-like (ECL) cell carcinoids, dysplasia, or neoplasia, such as those seen in rodent studies, have been reported in humans.
- Cardiovascular events: [US Boxed Warning]: NSAIDs cause an increased risk of serious (and potentially fatal) adverse cardiovascular thrombotic events, including MI and stroke. Risk may occur early during treatment and may increase with duration of use. Relative risk appears to be similar in those with and without known cardiovascular disease or risk factors for cardiovascular disease; however, absolute incidence of serious cardiovascular thrombotic events (which may occur early during treatment) was higher in patients with known cardiovascular disease or risk factors and in those receiving higher doses. New-onset hypertension or exacerbation of hypertension may occur (NSAIDs may also impair response to ACE inhibitors, thiazide diuretics, or loop diuretics); may contribute to cardiovascular events; monitor blood pressure; use with caution in patients with hypertension. May cause sodium and fluid retention, use with caution in patients with edema. Avoid use in heart failure (ACCF/AHA [Yancy, 2013]). Avoid use in patients with a recent MI unless benefits outweigh risk of cardiovascular thrombotic events. Use the lowest effective dose for the shortest duration of time, consistent with individual patient goals, to reduce risk of cardiovascular events; alternate therapies should be considered for patients at high risk.
- Clostridioides (formerly Clostridium) difficile-associated diarrhea (CDAD): Use of proton pump inhibitors (PPIs) may increase risk of CDAD, especially in hospitalized patients; consider CDAD diagnosis in patients with persistent diarrhea that does not improve. Use the lowest dose and shortest duration of PPI therapy appropriate for the condition being treated.
- CNS effects: May cause drowsiness, dizziness, blurred vision, and other neurologic effects which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving). Discontinue use with blurred or diminished vision and perform ophthalmologic exam. Periodically evaluate vision in all patients receiving long term therapy.
- Cutaneous and systemic lupus erythematosus: Has been reported as new onset or exacerbation of existing autoimmune disease; most cases were cutaneous lupus erythematosus (CLE), most commonly, subacute CLE (occurring within weeks to years after continuous therapy). Systemic lupus erythematosus (SLE) is less common (typically occurs within days to years after initiating treatment) and occurred primarily in young adults up to the elderly. Discontinue therapy if signs or symptoms of CLE or SLE occur and refer to specialist for evaluation; most patients improve 4 to 12 weeks after discontinuation of esomeprazole.
- Fractures: Increased incidence of osteoporosis-related bone fractures of the hip, spine, or wrist may occur with proton pump inhibitor (PPI) therapy. Patients on high-dose or long-term therapy (≥1 year) should be monitored. Use the lowest effective dose for the shortest duration of time, use vitamin D and calcium supplementation, and follow appropriate guidelines to reduce risk of fractures.
- Fundic gland polyps: Use of PPIs increases risk of fundic gland polyps, especially with long-term use >1 year. May occur without symptoms but nausea, vomiting, or abdominal pain may occur; GI bleeding and/or anemia may occur with ulcerated polyps. Diagnosis of polyps may also increase risk for small intestinal blockage. Use the lowest dose and shortest duration of PPI therapy appropriate for the condition being treated.
- GI events: [US Boxed Warning]: NSAIDs cause increased risk of serious GI inflammation, ulceration, bleeding, and perforation (may be fatal); elderly patients and patients with history of peptic ulcer disease and/or GI bleeding are at greater risk of serious GI events. These events may occur at any time during therapy and without warning. Avoid use in patients with active GI bleeding. In patients with a history of acute lower GI bleeding, avoid use of non-aspirin NSAIDs, especially if due to angioectasia or diverticulosis (Strate 2016). Use caution with a history of GI ulcers, concurrent therapy known to increase the risk of GI bleeding (eg, aspirin, anticoagulants, corticosteroids, selective serotonin reuptake inhibitors), advanced hepatic disease, coagulopathy, smoking, use of alcohol, or in elderly or debilitated patients. Use the lowest effective dose for the shortest duration of time, consistent with individual patient goals, to reduce risk of GI adverse events; alternate therapies should be considered for patients at high risk.
- Hematologic effects: Platelet adhesion and aggregation may be decreased; may prolong bleeding time; patients with coagulation disorders or who are receiving anticoagulants should be monitored closely. Anemia may occur; patients on long-term NSAID therapy should be monitored for anemia. Rarely, NSAID use has been associated with potentially severe blood dyscrasias (eg, agranulocytosis, thrombocytopenia, aplastic anemia).
- Hepatic effects: Transaminase elevations have been reported with NSAID use; closely monitor patients with any abnormal LFT. Rare (sometimes fatal) severe hepatic reactions (eg, fulminant hepatitis, hepatic necrosis, hepatic failure) have occurred with NSAID use; discontinue immediately if signs or symptoms of hepatic disease develop or if systemic manifestations occur.
- Hyperkalemia: NSAID use may increase the risk of hyperkalemia, particularly in elderly patients, patients with diabetes, renal disease, and with concomitant use of other agents capable of inducing hyperkalemia (eg, ACE-inhibitors). Monitor potassium closely.
- Hypomagnesemia: Reported rarely, usually with prolonged PPI use of ≥3 months (most cases >1 year of therapy). May be symptomatic or asymptomatic; severe cases may cause tetany, seizures, and cardiac arrhythmias. Consider obtaining serum magnesium concentrations prior to beginning long-term therapy, especially if taking concomitant digoxin, diuretics, or other drugs known to cause hypomagnesemia; and periodically thereafter. Hypomagnesemia may be corrected by magnesium supplementation, although discontinuation of esomeprazole may be necessary; magnesium levels typically return to normal within 1 week of stopping.
- Interstitial nephritis: Acute interstitial nephritis has been observed in patients taking PPIs; may occur at any time during therapy and is generally due to an idiopathic hypersensitivity reaction. Discontinue if acute interstitial nephritis develops.
- Renal effects: NSAID use may compromise existing renal function; dose-dependent decreases in prostaglandin synthesis may result from NSAID use, reducing renal blood flow which may cause renal decompensation (usually reversible). Patients with impaired renal function, dehydration, hypovolemia, heart failure, hepatic impairment, those taking diuretics, and ACE inhibitors, and the elderly are at greater risk of renal toxicity. Rehydrate patient before starting therapy; monitor renal function closely. Long-term NSAID use may result in renal papillary necrosis and other renal injury.
- Skin reactions: NSAIDs may cause potentially fatal serious skin adverse events including exfoliative dermatitis, Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN); may occur without warning; discontinue use at first sign of skin rash (or any other hypersensitivity).
- Vitamin B12 deficiency: Prolonged treatment (≥2 years) may lead to vitamin B12 malabsorption and subsequent vitamin B12 deficiency. The magnitude of the deficiency is dose-related and the association is stronger in females and those younger in age (<30 years); prevalence is decreased after discontinuation of therapy (Lam, 2013).
Disease-related concerns:
- Aseptic meningitis: May increase the risk of aseptic meningitis, especially in patients with systemic lupus erythematosus (SLE) and mixed connective tissue disorders.
- Asthma: Contraindicated in patients with aspirin-sensitive asthma; severe and potentially fatal bronchospasm may occur. Use caution in patients with other forms of asthma.
- Bariatric surgery: Gastric ulceration: Avoid chronic use of oral nonselective NSAIDs after bariatric surgery; development of anastomotic ulcerations/perforations may occur (Bhangu 2014; Mechanick 2013). Short-term use of celecoxib or IV ketorolac are recommended as part of a multimodal pain management strategy for postoperative pain (Chou 2016; Horsley 2019; Thorell 2016).
- Coronary artery bypass graft surgery: [US Boxed Warning]: Use is contraindicated in the setting of coronary artery bypass graft (CABG) surgery. Risk of MI and stroke may be increased with use following CABG surgery.
- Gastric malignancy: Relief of symptoms does not preclude the presence of a gastric malignancy.
- Gastrointestinal infection (eg, Salmonella, Campylobacter): Use of PPIs may increase risk of these infections.
- Hepatic impairment: Use with caution in patients with mild to moderate hepatic impairment; avoid use in severe hepatic impairment.
- Renal impairment: Avoid use in patients with advanced renal disease.
Concurrent drug therapy issues:
- Clopidogrel: Proton pump inhibitors (PPIs) may diminish the therapeutic effect of clopidogrel thought to be due to reduced formation of the active metabolite of clopidogrel. The manufacturer of clopidogrel recommends either avoidance of both omeprazole (even when scheduled 12 hours apart) and esomeprazole or use of a PPI with comparatively less effect on the active metabolite of clopidogrel (eg, pantoprazole). In contrast to these warnings, others have recommended the continued use of PPIs, regardless of the degree of inhibition, in patients with a history of GI bleeding or multiple risk factors for GI bleeding who are also receiving clopidogrel since no evidence has established clinically meaningful differences in outcome; however, a clinically significant interaction cannot be excluded in those who are poor metabolizers of clopidogrel (Abraham, 2010; Levine, 2011).
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Elderly patients are at increased risk for serious GI, cardiovascular, and/or renal adverse events; use with caution. Patients ≥50 years of age may be at increased risk for development of fractures with use of proton pump inhibitors; bioavailability of esomeprazole may be increased in elderly patients.
Other warnings/precautions:
- Laboratory test interference: Serum chromogranin A (CgA) levels increase secondary to drug-induced decreases in gastric acid; may cause false-positive results in diagnostic investigations for neuroendocrine tumors. Temporarily stop esomeprazole treatment ≥14 days before CgA test; if CgA level high, repeat test to confirm. Use same commercial laboratory for testing to prevent variable results.
- Surgical/dental procedures: Withhold products containing naproxen for at least 4 to 6 half-lives prior to surgical or dental procedures; consider alternative product if PPI is required.
Monitoring Parameters
CBC, chemistry profile, occult blood loss, and periodic liver function test; renal function (urine output, serum BUN and creatinine); blood pressure; periodic ophthalmic exam with long-term therapy.
Pregnancy
Pregnancy Considerations
Animal reproduction studies have not been conducted with this combination. Because they may cause premature closure of the ductus arteriosus, use of NSAIDs late in pregnancy should be avoided. Refer to individual agents.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience constipation, diarrhea, abdominal pain, passing gas, nausea, vomiting, or heartburn. Have patient report immediately to prescriber signs of lupus (rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs), signs of low magnesium (mood changes; muscle pain or weakness; muscle cramps or spasms; seizures; tremors; lack of appetite; severe nausea or vomiting; or an abnormal heartbeat), signs of Clostridium difficile (C. diff)-associated diarrhea (abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools), signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), signs of kidney problems (unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain), signs of bleeding (vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding), signs of high potassium (abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, or numbness or tingling feeling), signs of severe cerebrovascular disease (change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes), severe headache, severe dizziness, passing out, chest pain, fast heartbeat, shortness of breath, excessive weight gain, swelling of arms or legs, severe loss of strength and energy, bone pain, noise or ringing in the ears, vision changes, depression, confusion, flu-like symptoms, signs of abdominal ulcers (severe abdominal or back pain; black, tarry, or bloody stools; vomiting blood or vomit that looks like coffee grounds; or weight gain or abnormal swelling), or signs of Stevens-Johnson syndrome/toxic epidermal necrolysis (red, swollen, blistered, or peeling skin [with or without fever]; red or irritated eyes; or sores in mouth, throat, nose, or eyes) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.