Boxed Warning
Toxicity:
Systemic absorption of neomycin occurs following oral administration, and toxic reactions may occur. Patients treated with neomycin should be under close clinical observation because of the potential toxicity associated with the use of neomycin. Neurotoxicity (including ototoxicity) and nephrotoxicity following the oral use of neomycin sulfate have been reported, even when used in recommended doses. The potential for nephrotoxicity, permanent bilateral auditory ototoxicity, and sometimes vestibular toxicity, is present in patients with healthy renal function when treated with higher doses of neomycin or for longer periods than recommended. Serial, vestibular and audiometric tests, as well as tests of renal function, should be performed (especially in high-risk patients). The risk of nephrotoxicity and ototoxicity is greater in patients with impaired renal function. Ototoxicity is often delayed in onset, and patients developing cochlear damage will not have symptoms during therapy to warn them of developing eighth nerve destruction, and total or partial deafness may occur long after neomycin has been discontinued.
Other factors which increase the risk of toxicity are advanced age and dehydration.
Neuromuscular blockade:
Neuromuscular blockage and respiratory paralysis have been reported following the oral use of neomycin. The possibility of the occurrence of neuromuscular blockage and respiratory paralysis should be considered if neomycin is administered, especially to patients receiving anesthetics; neuromuscular-blocking agents such as tubocurarine, succinylcholine, decamethonium; or massive transfusions of citrate anticoagulated blood. If blockage occurs, calcium salts may reverse these phenomena, but mechanical respiratory assistance may be necessary.
Concurrent therapy:
Concurrent or sequential systemic, oral or topical use of other aminoglycosides, including paromomycin and other potentially nephrotoxic or neurotoxic drugs such as bacitracin, cisplatin, vancomycin, amphotericin B, polymyxin B, colistin and viomycin, should be avoided because the toxicity may be additive.
The concurrent use of neomycin with potent diuretics such as ethacrynic acid or furosemide should be avoided, since certain diuretics by themselves may cause ototoxicity. In addition, when administered intravenously (IV), diuretics may enhance neomycin toxicity by altering the antibiotic concentration in serum and tissue.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral, as sulfate:
Generic: 500 mg
Pharmacology
Mechanism of Action
Interferes with bacterial protein synthesis by binding to 30S ribosomal subunits
Pharmacokinetics/Pharmacodynamics
Absorption
Oral, percutaneous: Poor (3%)
Distribution
97% of an orally administered dose remains in the GI tract. Absorbed neomycin distributes to tissues and concentrates in the renal cortex. With repeated doses, accumulation also occurs in the inner ear.
Excretion
Feces (97% of oral dose as unchanged drug); urine (30% to 50% of absorbed drug as unchanged drug)
Time to Peak
1 to 4 hours
Protein Binding
0% to 30%
Use: Labeled Indications
Hepatic coma (portal-systemic encephalopathy): Adjunctive therapy in hepatic coma.
Surgical (perioperative) prophylaxis: Adjunctive therapy as part of a regimen for the suppression of the normal bacterial bowel flora (eg, preoperative bowel preparation), given concomitantly with enteric-coated erythromycin base.
Contraindications
Hypersensitivity to the neomycin or any component of the formulation; intestinal obstruction; patients with inflammatory or ulcerative GI disease. Patients with a history of hypersensitivity or serious toxic reaction to other aminoglycosides may have a cross-sensitivity to neomycin.
Dosage and Administration
Dosing: Adult
Surgical (perioperative) prophylaxis: Oral: 1 g at 1 PM, 2 PM, and 11 PM on the day preceding 8 AM surgery as an adjunct to mechanical cleansing of the intestine in combination with oral erythromycin (manufacturer’s labeling) or in combination with erythromycin or metronidazole, and IV antibiotics on the day of surgery (Bratzler 2013)
Hepatic encephalopathy: Oral: 4 to 12 g daily divided every 4 to 6 hours for 5 to 6 days
Chronic hepatic insufficiency: Oral: 4 g daily for an indefinite period
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosage expressed in terms of neomycin sulfate.
Cholangitis, prophylaxis recurrent episodes after Kasai portoenterostomy: Limited data available: Infants and Children ≤3 years: Oral: 25 to 50 mg/kg/day in 4 divided doses 4 days per week; continue until 2 to 3 years of age. Dosing based on a prospective, randomized, comparative trial and a small case series of patients ≤2 years of age at time of therapy initiation who had an episode of cholangitis after a Kasai portoenterostomy (n=10). In the trial, two prophylactic regimens were compared (neomycin vs trimethoprim/sulfamethoxazole) against historic controls; the mean age at time of therapy initiation was 6.1 ± 3.6 months; both neomycin and trimethoprim/sulfamethoxazole decreased cholangitis incidence by ~60% and neomycin increased survival. In the case series, dosing was started at 25 mg/kg/day or 50 mg/kg/day for 5 days just prior to discharge then given 4 days per week (4 days on, 3 days off) (Bu 2003; Lien 2015; Mones 1994).
Enteric bacteria eradication (including gut flora)/infection: Limited data available: Note: Use of neomycin for the treatment of enteric infection has been replaced by other agents; most contemporary use is for eradication of intestinal flora (Red Book [AAP 2015]). Infants, Children, and Adolescents: Oral: 50 to 100 mg/kg/day divided every 6 to 8 hours; maximum daily dose: 12 g/day (Bradley 2017; Marks 1973; Red Book [AAP 2015]); duration of treatment should not exceed 2 weeks due to GI absorption which may result in systemic toxicities
Hepatic encephalopathy: Limited data available: Infants, Children, and Adolescents: Oral: 50 to 100 mg/kg/day divided every 6 hours for a maximum of 7 days with or without lactulose (Debray 2006; Lovejoy 1975); maximum daily dose: 12 g/day
Preoperative intestinal antisepsis: Limited data available: Infants, Children, and Adolescents: Oral: 15 mg/kg/dose for 3 doses administered over 10 hours (eg, at 1 PM, 2 PM, and 11 PM) the day before surgery; maximum dose: 1,000 mg/dose (Bratzler 2013; Breckler 2010; Debo Adeyemi 1986; Feng 2015, Feng 2015a, Kliegman 2007; Pennington 2014; Rangel 2015); used in combination with other oral antimicrobial (eg, erythromycin or metronidazole) and with/or without adjunct to mechanical cleansing of the intestine (Feng 2015; Feng 2015a)
Storage
Store at 20ºC to 25ºC (68ºF to 77ºF).
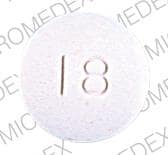
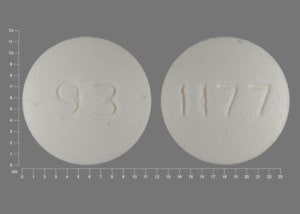
Neomycin Images
Drug Interactions
Acarbose: Neomycin may enhance the adverse/toxic effect of Acarbose. Neomycin may decrease the metabolism of Acarbose. Monitor therapy
Amphotericin B: May enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
Arbekacin: May enhance the nephrotoxic effect of Aminoglycosides. Arbekacin may enhance the ototoxic effect of Aminoglycosides. Monitor therapy
Ataluren: May enhance the adverse/toxic effect of Aminoglycosides. Specifically, an increased risk of nephrotoxicity may occur with the concomitant use of ataluren and aminoglycosides. Avoid combination
Bacitracin (Systemic): Neomycin may enhance the nephrotoxic effect of Bacitracin (Systemic). Avoid combination
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Bisphosphonate Derivatives: Aminoglycosides may enhance the hypocalcemic effect of Bisphosphonate Derivatives. Monitor therapy
Botulinum Toxin-Containing Products: Aminoglycosides may enhance the neuromuscular-blocking effect of Botulinum Toxin-Containing Products. Monitor therapy
Capreomycin: May enhance the neuromuscular-blocking effect of Aminoglycosides. Monitor therapy
CARBOplatin: Aminoglycosides may enhance the ototoxic effect of CARBOplatin. Especially with higher doses of carboplatin. Monitor therapy
Cardiac Glycosides: Aminoglycosides may decrease the serum concentration of Cardiac Glycosides. This effect has only been demonstrated with oral aminoglycoside administration. Monitor therapy
Cefazedone: May enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
Cephalosporins (2nd Generation): May enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
Cephalosporins (3rd Generation): May enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
Cephalosporins (4th Generation): May enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
Cephalothin: May enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
Cephradine: May enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
CISplatin: May enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
Colistimethate: Aminoglycosides may enhance the nephrotoxic effect of Colistimethate. Aminoglycosides may enhance the neuromuscular-blocking effect of Colistimethate. Consider therapy modification
CycloSPORINE (Systemic): Aminoglycosides may enhance the nephrotoxic effect of CycloSPORINE (Systemic). Monitor therapy
Distigmine: Aminoglycosides may diminish the therapeutic effect of Distigmine. Monitor therapy
Foscarnet: May enhance the nephrotoxic effect of Aminoglycosides. Avoid combination
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Loop Diuretics: May enhance the adverse/toxic effect of Aminoglycosides. Specifically, nephrotoxicity and ototoxicity. Monitor therapy
Mannitol (Systemic): May enhance the nephrotoxic effect of Aminoglycosides. Avoid combination
Mecamylamine: Aminoglycosides may enhance the neuromuscular-blocking effect of Mecamylamine. Avoid combination
Methoxyflurane: Aminoglycosides may enhance the nephrotoxic effect of Methoxyflurane. Avoid combination
Neuromuscular-Blocking Agents: Aminoglycosides may enhance the respiratory depressant effect of Neuromuscular-Blocking Agents. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May decrease the excretion of Aminoglycosides. Data only in premature infants. Monitor therapy
Oxatomide: May enhance the ototoxic effect of Aminoglycosides. Monitor therapy
Penicillins: May decrease the serum concentration of Aminoglycosides. Primarily associated with extended spectrum penicillins, and patients with renal dysfunction. Exceptions: Amoxicillin; Ampicillin; Bacampicillin; Cloxacillin; Dicloxacillin; Nafcillin; Oxacillin; Penicillin G (Parenteral/Aqueous); Penicillin G Benzathine; Penicillin G Procaine; Penicillin V Benzathine; Penicillin V Potassium. Consider therapy modification
Regorafenib: Neomycin may decrease serum concentrations of the active metabolite(s) of Regorafenib. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
SORAfenib: Neomycin may decrease the serum concentration of SORAfenib. Monitor therapy
Tenofovir Products: Aminoglycosides may increase the serum concentration of Tenofovir Products. Tenofovir Products may increase the serum concentration of Aminoglycosides. Monitor therapy
Vancomycin: May enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Neomycin may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Sore mouth
Gastrointestinal: Anorectal pain, diarrhea, mouth irritation, nausea, rectal irritation, vomiting
<1%, postmarketing, and/or case reports: Auditory ototoxicity, dyspnea, eosinophilia, nephrotoxicity, neurotoxicity, vestibular ototoxicity
Warnings/Precautions
Concerns related to adverse effects:
- Malabsorption: Small amounts of neomycin are absorbed through intact intestinal mucosa; increases in fecal bile acid excretion and reduction of intestinal lactase activity may occur. Oral doses of >12 g/day produce malabsorption of fats, nitrogen, cholesterol, carotene, glucose, xylose, lactose, sodium, calcium, cyanocobalamin and iron.
- Nephrotoxicity: [US Boxed Warning]: May cause nephrotoxicity; usual risk factors include preexisting renal impairment, concomitant nephrotoxic medications, advanced age and dehydration. Discontinue treatment if signs of nephrotoxicity occur; renal damage is usually reversible.
- Neuromuscular blockade and respiratory paralysis: [US Boxed Warning]: May cause neuromuscular blockade and respiratory paralysis; especially when given soon after anesthesia or muscle relaxants.
- Neurotoxicity: [US Boxed Warning]: May cause neurotoxicity; symptoms also include numbness, skin tingling, muscle twitching and seizures. Usual risk factors include preexisting renal impairment and concomitant neuro-/nephrotoxic medications. Discontinue treatment if signs of ototoxicity occur; risk of hearing loss continues after drug withdrawal.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Hearing impairment: Use with caution in patients with preexisting vertigo, tinnitus, or hearing loss.
- Neuromuscular disorders: Use with caution in patients with neuromuscular disorders, including myasthenia gravis and Parkinson disease.
- Renal impairment: Use with caution in patients with preexisting renal insufficiency; dosage modification required.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC, 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors, 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
Other warnings/precautions:
- Parenteral administration: More toxic than other aminoglycosides when given parenterally; do not administer parenterally.
- Surgical irrigation: Do not use as surgical irrigation due to significant systemic absorption of the drug.
Monitoring Parameters
Serum creatinine/BUN at baseline and periodically during chronic therapy; audiometry in symptomatic patients
Pregnancy
Pregnancy Risk Factor
D
Pregnancy Considerations
Animal reproduction studies have not been conducted. Aminoglycosides cross the placenta. Aminoglycosides may cause fetal harm if administered to a pregnant woman. There are several reports of total irreversible bilateral congenital deafness in children whose mothers received another aminoglycoside (streptomycin) during pregnancy. Although serious side effects to the fetus/infant have not been reported following maternal use of all aminoglycosides, a potential for harm exists. Large oral doses may cause malabsorption of some nutrients in the mother.
Patient Education
What is this drug used for?
- It is used to prevent infections during bowel surgery.
- It is used to lower the signs of hepatic coma.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Muscle weakness
- Severe dizziness
- Passing out
- Noise or ringing in the ears
- Hearing loss
- Hearing changes
- Burning or numbness feeling
- Seizures
- Twitching
- Change in balance
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.