Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule Extended Release, Oral:
Generic: 250 mg, 500 mg
Capsule Extended Release, Oral [preservative free]:
Generic: 250 mg, 500 mg
Powder, Oral:
Generic: (100 g, 500 g, 1000 g)
Tablet, Oral:
Niacin-50: 50 mg [starch free, sugar free, wheat free]
Niacor: 500 mg [scored]
Generic: 50 mg, 100 mg, 250 mg, 500 mg
Tablet, Oral [preservative free]:
Generic: 50 mg [DSC], 100 mg, 500 mg
Tablet Extended Release, Oral:
Niaspan: 500 mg [contains fd&c yellow #6 aluminum lake]
Niaspan: 750 mg
Niaspan: 750 mg [DSC], 1000 mg [contains fd&c yellow #6 aluminum lake]
Slo-Niacin: 250 mg [scored]
Slo-Niacin: 500 mg, 750 mg [scored; contains fd&c red #40]
Generic: 500 mg, 750 mg, 1000 mg
Tablet Extended Release, Oral [preservative free]:
Generic: 250 mg, 500 mg, 1000 mg
Pharmacology
Mechanism of Action
Niacin (nicotinic acid) is bioconverted to nicotinamide which is further converted to nicotinamide adenine dinucleotide (NAD+) and the hydride equivalent (NADH) which are coenzymes necessary for tissue metabolism, lipid metabolism, and glycogenolysis (Belenky 2006; Sauve 2008). The mechanism by which niacin (in lipid-lowering doses) affects plasma lipoproteins is not fully understood. It may involve several actions including partial inhibition of release of free fatty acids from adipose tissue, and increased lipoprotein lipase activity, which may increase the rate of chylomicron triglyceride removal from plasma. Ultimately, niacin reduces total cholesterol, apolipoprotein (apo) B, triglycerides, VLDL, LDL, lipoprotein (a), and increases HDL and other important components and subfractions (eg, LPA-I) (Kamanna 2000)
Pharmacokinetics/Pharmacodynamics
Absorption
Immediate release formulation: Rapid and extensive. Extent of niacin ER absorption from niacin ER/lovastatin is increased (22% to 30%) with food.
Distribution
Mainly to hepatic, renal, and adipose tissue
Metabolism
Extensive first-pass metabolism; converted to nicotinamide adenine dinucleotide, nicotinuric acid (after conjugation with glycine), and other metabolites. At doses used to treat hyperlipidemia, metabolic pathways are saturable.
Excretion
Urine 60% to 88% (unchanged drug [up to 12% recovered after multiple dosing] and metabolites)
Time to Peak
Serum: Immediate release formulation: 30 to 60 minutes; extended release formulation: 4 to 5 hours
Half-Life Elimination
25 to 48 minutes
Protein Binding
<20% bound to serum proteins
Use in Specific Populations
Special Populations: Gender
Steady-state plasma concentrations and metabolites are generally higher in women.
Use: Labeled Indications
Dietary supplement: Use as a dietary supplement.
Dyslipidemias: Treatment of dyslipidemias (Fredrickson types IIa and IIb or primary hypercholesterolemia) as mono- or adjunctive therapy; to lower the risk of recurrent MI in patients with a history of MI and hyperlipidemia; to slow progression or promote regression of coronary artery disease; adjunctive therapy for severe hypertriglyceridemia in adults at risk of pancreatitis
Note: Niacin is no longer considered a primary or secondary agent for dyslipidemias. Although niacin consistently affects surrogate markers, especially LDL-C, it has not been shown to reduce cardiovascular disease outcomes beyond that achieved with statin use and may be associated with harm (ACC [Lloyd-Jones 2017]; Garg 2017; Wierzbicki 2014). In two large clinical trials, the addition of niacin to patients receiving simvastatin did not reduce cardiovascular morbidity or mortality (Boden 2011; Landray 2014). May consider use in patients with very high triglyceride levels (>500 mg/dL) or in dyslipidemia for patients who do not achieve the desired response or have intolerance to a statin or other alternative therapy (Boden 2014; Flink 2015).
Use: Off Label
Pellagrac
Data from a limited number of patients studied (case reports) suggest that niacin may be beneficial for the treatment of pellagra Delgado-Sanchez 2008, Oldham 2012, Prousky 2003. Clinical experience also suggests the utility of niacin in the treatment of pellagra Hegyi 2004, Jen 2010. Additional data may be necessary to further define the role of niacin in this condition. Note: Niacinamide may be preferred over niacin based on a more favorable side effect profile Hegyi 2004, Jen 2010.
Contraindications
Hypersensitivity to niacin, niacinamide, or any component of the formulation; active hepatic disease or significant or unexplained persistent elevations in hepatic transaminases; active peptic ulcer; arterial hemorrhage
Dosage and Administration
Dosing: Adult
Note: Formulations of niacin (regular release versus extended release) are not interchangeable.
Dietary supplement (OTC labeling): Oral: 50 mg twice daily or 100 mg once daily. Note: Many over-the-counter formulations exist.
Dyslipidemia: Oral: Note: Niacin is no longer recommended, except in specific clinical situations (eg, high triglyceride levels [>500 mg/dL], if not able to achieve desired response, or intolerance to other therapies) (ACC [Lloyd-Jones 2017]; Boden 2014; Garg 2017; Landray 2014; Wierzbicki 2014).
Regular release formulation (Niacor): Initial: 250 mg once daily (with evening meal); increase frequency and/or dose every 4 to 7 days to desired response or first-level therapeutic dose (1.5 to 2 g daily in 2 to 3 divided doses); after 2 months, may increase at 2- to 4-week intervals to 3 g daily in 3 divided doses (maximum dose: 6 g daily in 3 divided doses). Note: Many over-the-counter formulations exist.
Sustained release (or controlled release) formulations: Note: Several over-the-counter formulations exist. Slo-Niacin: Usual dosage is 250 to 750 mg once daily, taken morning or evening, or as directed. Before using more than 500 mg daily, patient should consult health care provider.
Extended release formulation (Niaspan): Initial: 500 mg at bedtime for 4 weeks, then 1 g at bedtime for 4 weeks; adjust dose to response and tolerance; may increase daily dose every 4 weeks by not more than 500 mg daily to a maximum of 2 g daily. Recommended maintenance dose: 1,000 to 2,000 mg at bedtime.
Pellagra (off-label use): Oral: Regular release formulation: 50 to 100 mg 3 to 4 times daily; maximum: 500 mg daily (Prousky 2003; Delgado-Sanchez 2008; DesGroseilliers 1976; Oldham 2012). Some experts prefer niacinamide for treatment due to more favorable side effect profile (Hegyi 2004; Jen 2010).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Formulations of niacin (regular release [crystalline] versus extended release) are not interchangeable.
Dyslipidemias: Very limited data available (Miller 2015): Note: Niacin (nicotinic acid) is rarely used in pediatric patients for treatment of dyslipidemias and is not considered a primary agent nor a routine secondary, adjunctive agent for dyslipidemia management in pediatric patients (AAP [Daniels 2008]; AHA [McCrindle 2007]; NHLBI 2011)
Children ≥10 years and Adolescents (Miller 2015; NHLBI 2011): Oral:
Regular release: Initial: 100 to 250 mg/day in 3 divided doses with meals; maximum initial daily dose: 10 mg/kg/day; increase weekly by 100 mg/day or increase every 2 to 3 weeks by 250 mg/day as tolerated; evaluate efficacy and adverse effects with laboratory tests at 20 mg/kg/day or 1,000 mg/day (whichever is less); continue to increase if needed and as tolerated; re-evaluate at each 500 mg increment; daily doses up to 2,250 mg/day have been used (Colletti 1993)
Sustained release: Reported range: 500 to 1,500 mg/day; initiate at a low dose administered once daily (based on experience in adults); reported initial daily dose has not exceeded 10 mg/kg/day; titrate every 3 to 4 weeks (in adults, doses are titrated every 4 weeks) (AHA [McCrindle 2007]; Colletti 1993)
Pellagra; treatment: Children and Adolescents: Oral: Regular release: 50 to 300 mg/day in divided doses 3 times daily; usual treatment duration is 3 to 4 weeks (Kliegman 2016; WHO 2000)
Dosing adjustment for toxicity: Children ≥10 years and Adolescents: In a trial of pediatric patients, discontinuation of niacin therapy was reported for hepatotoxicity (eg, transaminases increases, either persistent or if symptoms of nausea, fever, and/or malaise), headache, abdominal pain and/or severe flushing (Colletti 1993)
Dosing: Adjustment for Toxicity
Hepatic toxicity: Transaminases rise ≥3 times ULN, either persistent or if symptoms of nausea, fever, and/or malaise occur: Discontinue therapy.
Administration
Administer with food. To attenuate flushing symptoms, may premedicate with aspirin 30 minutes before dose; avoid ingestion of alcohol, hot or spicy foods/liquids concurrently with niacin. May also use other NSAIDs to prevent flushing according to the manufacturer.
Niaspan: Administer at bedtime after a low-fat snack. Two of the 500 mg and one of the 1,000 mg tablet strengths are interchangeable, but three of the 500 mg and two of the 750 mg tablet strengths are not interchangeable. When switching from immediate-release tablet, initiate Niaspan with the recommended titration schedule. If therapy is interrupted for an extended period, dose should be retitrated.
Long-acting forms should not be crushed, broken, or chewed. Slo-Niacin may be broken along the score line. Do not substitute long-acting forms for immediate release ones.
Dietary Considerations
Should be taken with meal; low-fat meal if treating dyslipidemia. Avoid alcohol, hot or spicy foods/liquids around the time of niacin dose.
Dietary adequate intake (National Academy of Sciences, 1998):
0 to 5 months: 2 mg daily
6 to 11 months: 3 mg daily
Dietary recommended daily allowances (National Academy of Sciences, 1998):
1 to 3 years: 6 mg daily
4 to 8 years: 8 mg daily
9 to 13 years: 12 mg daily
14 to 18 years: Females: 14 mg daily; Males: 16 mg daily
≥19 years: Females: 14 mg daily; Males: 16 mg daily
Pregnancy (all ages): 18 mg daily
Lactation (all ages): 17 mg daily
Storage
Store at room temperature.
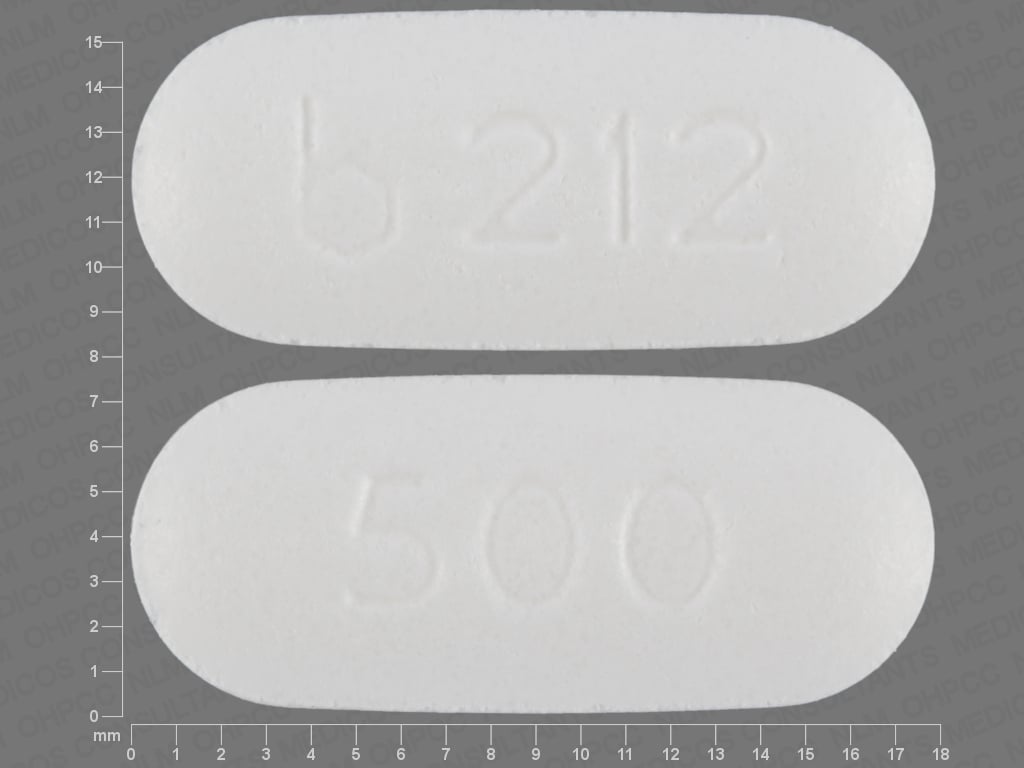
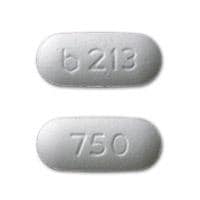
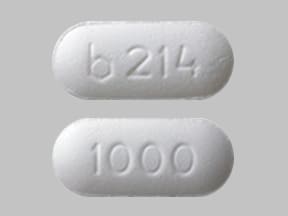
Niacin Images
Drug Interactions
Alcohol (Ethyl): May enhance the adverse/toxic effect of Niacin. Consider therapy modification
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Niacin. Consider therapy modification
HMG-CoA Reductase Inhibitors (Statins): Niacin may enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Rosuvastatin: Niacin may enhance the myopathic (rhabdomyolysis) effect of Rosuvastatin. Monitor therapy
Simvastatin: Niacin may enhance the myopathic (rhabdomyolysis) effect of Simvastatin. Niacin may increase the serum concentration of Simvastatin. Management: Use of simvastatin with niacin should be avoided in Chinese patients; some non-US labeling state this combination is not recommended in any Asian patients. Consider therapy modification
Test Interactions
False elevations in some fluorometric determinations of plasma or urinary catecholamines; false-positive urine glucose (Benedict's reagent)
Adverse Reactions
Frequency not defined.
Cardiovascular: Atrial fibrillation, cardiac arrhythmia, edema, flushing, hypotension, orthostatic hypotension, palpitations, tachycardia
Central nervous system: Chills, dizziness, headache, insomnia, migraine, myasthenia, nervousness, pain, paresthesia
Dermatologic: Acanthosis nigricans, burning sensation of skin, diaphoresis, hyperpigmentation, maculopapular rash, pruritus, skin discoloration, skin rash, urticaria, xeroderma
Endocrine & metabolic: Decreased glucose tolerance, decreased serum phosphate, gout, hyperuricemia, increased amylase, increased lactate dehydrogenase
Gastrointestinal: Abdominal pain, diarrhea, dyspepsia, eructation, flatulence, nausea, peptic ulcer, vomiting
Hematologic & oncologic: Decreased platelet count, prolonged prothrombin time
Hepatic: Hepatitis, increased serum bilirubin, increased serum transaminases (dose-related), jaundice,
Neuromuscular & skeletal: Increased creatine phosphokinase, leg cramps, myalgia, myopathy (with concurrent HMG-CoA reductase inhibitor), weakness
Ophthalmic: Blurred vision, cystoid macular edema, toxic amblyopia
Respiratory: Cough, dyspnea
<1%, postmarketing, and/or case reports: Hepatic necrosis, hypersensitivity reaction (includes anaphylaxis, angioedema, laryngismus, vesiculobullous rash), rhabdomyolysis (with concurrent HMG-CoA reductase inhibitor), syncope
Warnings/Precautions
Concerns related to adverse effects:
- Flushing/pruritus: Flushing and pruritus are common adverse effects of niacin; may be attenuated with a gradual increase in dose, administering with food, avoidance of concurrent ingestion of ethanol, hot or spicy foods/liquids, and/or by taking aspirin 30 minutes before dosing. May also use other NSAIDs according to the manufacturer. Flushing associated with extended-release preparation is significantly reduced (Guyton 2007). For immediate-release preparations, may administer in 2 to 3 divided doses to reduce the frequency and severity of flushing/pruritus. Consider discontinuation if persistent severe cutaneous symptoms occur during therapy.
- GI effects: May cause GI distress, vomiting, diarrhea, or aggravate peptic ulcer; GI distress may be attenuated with a gradual increase in dose and administration with food. Use is contraindicated in patients with active peptic ulcer disease; use with caution in patients with a past history of peptic ulcer. Consider discontinuation if unexplained abdominal pain/weight loss or other GI symptoms occur during therapy.
- Hematologic effects: Dose-related reductions in platelet count and increases of prothrombin time may occur.
- Hepatotoxicity: Cases of severe hepatotoxicity, including fulminant hepatic necrosis, have occurred when immediate-release (crystalline) niacin products have been substituted with sustained-release (modified-release, timed-release) niacin products at equivalent doses. Patients should be initiated with low doses (eg, niacin extended-release 500 mg at bedtime) with titration to achieve desired response. Liver function tests should be monitored in all patients receiving lipid-lowering doses of niacin. Discontinue use if hepatic transaminase levels rise, particularly to 3 x ULN and are persistent, or if they are associated with symptoms of nausea, fever, and/or malaise.
- Hypophosphatemia: Has been associated with small but statistically significant dose-related reductions in phosphorus levels. Monitor phosphorus levels periodically in patients at risk for hypophosphatemia.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with unstable angina or in the acute phase of an MI. In patients with preexisting coronary artery disease, the incidence of atrial fibrillation was observed more frequently in those receiving immediate-release (crystalline) niacin as compared to placebo (Coronary Drug Project Research Group 1975). Consider discontinuation if new-onset atrial fibrillation occurs during therapy.
- Diabetes: Use is associated with new-onset diabetes or worsening glucose tolerance in patients with preexisting diabetes (Garg 2017; Goldie 2016). Use with caution in patients with diabetes. Monitor glucose; adjustment of diet and/or hypoglycemic therapy may be necessary. Consider discontinuation if persistent hyperglycemia occurs during therapy.
- Gout: May be associated with hyperuricemia. Use with caution in patients predisposed to gout. Consider discontinuation if acute gout occurs during therapy.
- Hepatic impairment: Use with caution in patients with a past history of hepatic impairment; monitor liver function tests. Contraindicated with active liver disease or unexplained persistent transaminase elevation.
- Renal impairment: Use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Product interchangeability: Formulations of niacin (immediate-release versus extended-release) are not interchangeable (bioavailability varies): cases of severe hepatotoxicity, including fulminant hepatic necrosis, have occurred in patients who have substituted niacin products at equivalent doses.
Other warnings/precautions:
- Alcohol use: Use with caution in patients who consume large amounts of ethanol due to the increased risk of liver dysfunction.
Monitoring Parameters
Blood glucose (in diabetic patients); if on concurrent HMG-CoA reductase inhibitor, may periodically check CPK and serum potassium; liver function tests pretreatment, every 6 to 12 weeks for first year, then periodically (approximately every 6 months), monitor liver function more frequently if history of transaminase elevation with prior use; lipid profile; platelets (if on anticoagulants); PT (if on anticoagulants); uric acid (if predisposed to gout); phosphorus (if predisposed to hypophosphatemia)
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Animal reproduction studies have not been conducted. Water soluble vitamins cross the placenta. When used as a dietary supplement, niacin requirements may be increased in pregnant women compared to nonpregnant women (IOM 1998). It is not known if niacin at lipid-lowering doses is harmful to the developing fetus. If a woman becomes pregnant while receiving niacin for primary hypercholesterolemia, niacin should be discontinued. If a woman becomes pregnant while receiving niacin for hypertriglyceridemia, the benefits and risks of continuing niacin should be assessed on an individual basis.
Patient Education
What is this drug used for?
- It is used to lower bad cholesterol and raise good cholesterol (HDL).
- It is used to lower triglycerides.
- This vitamin is used to treat niacin deficiency.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Flushing
- Itching
- Diarrhea
- Cough
- Nausea
- Vomiting
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Muscle pain
- Muscle weakness
- Chest pain
- Severe dizziness
- Passing out
- Shortness of breath
- Sweating a lot
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.