Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral, as macrocrystals:
Macrodantin: 25 mg
Macrodantin: 50 mg, 100 mg [contains fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Generic: 25 mg, 50 mg, 100 mg
Capsule, Oral, as monohydrate/macrocrystals:
Macrobid: 100 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40, fd&c yellow #10 (quinoline yellow)]
Generic: 100 mg
Suspension, Oral:
Furadantin: 25 mg/5 mL (230 mL [DSC])
Furadantin: 25 mg/5 mL (230 mL [DSC]) [contains methylparaben, propylparaben]
Generic: 25 mg/5 mL (230 mL, 240 mL)
Pharmacology
Mechanism of Action
Nitrofurantoin is reduced by bacterial flavoproteins to reactive intermediates that inactivate or alter bacterial ribosomal proteins leading to inhibition of protein synthesis, aerobic energy metabolism, DNA, RNA, and cell wall synthesis. Nitrofurantoin is bactericidal in urine at therapeutic doses. The broad-based nature of this mode of action may explain the lack of acquired bacterial resistance to nitrofurantoin, as the necessary multiple and simultaneous mutations of the target macromolecules would likely be lethal to the bacteria.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed; macrocrystalline is absorbed more slowly due to slower dissolution (causes less GI distress)
Distribution
Vd: 0.8 L/kg
Metabolism
Body tissues (except plasma) metabolize 60% of drug to inactive metabolites
Excretion
Suspension: Urine (~40%) and feces (small amounts) as metabolites and unchanged drug
Macrocrystals: Urine (20% to 25% as unchanged drug)
Half-Life Elimination
20 to 60 minutes; prolonged with renal impairment
Protein Binding
60% to 90%
Use in Specific Populations
Special Populations: Renal Function Impairment
Nitrofurantoin accumulates in serum.
Use: Labeled Indications
Cystitis, acute uncomplicated, treatment:
Nitrofurantoin monohydrate/macrocrystals (Macrobid): Treatment of acute uncomplicated cystitis caused by susceptible strains of Escherichia coli or Staphylococcus saprophyticus in patients ≥12 years of age
Nitrofurantoin macrocrystals (Furadantin, Macrodantin): Treatment of acute uncomplicated cystitis when caused by susceptible strains of E. coli, enterococci, Staphylococcus aureus, and certain susceptible strains of Klebsiella and Enterobacter species
Limitations of use: Not indicated for treatment of pyelonephritis or perinephric abscess
Cystitis, recurrent, prophylaxis: Nitrofurantoin macrocrystals (Furadantin, Macrodantin): Chronic suppression of recurrent UTIs
Use: Off Label
Bacteriuria, asymptomatic, in pregnancybyes
Based on the Infectious Diseases Society of America clinical practice guideline for the management of asymptomatic bacteriuria, nitrofurantoin is an effective and recommended agent in the management of asymptomatic bacteriuria (≥105 CFU per mL) in pregnancy.
Data from a randomized, controlled trial support the use of nitrofurantoin for the treatment of asymptomatic bacteriuria in pregnancy Lumbiganon 2009.
Contraindications
Anuria, oliguria, or significant impairment of renal function (creatinine clearance [CrCl] <60 mL/minute or clinically significant elevated serum creatinine); previous history of cholestatic jaundice or hepatic dysfunction associated with prior nitrofurantoin use; hypersensitivity to drug or any component of the formulation.
Note: The manufacturer's contraindication in patients with CrCl <60 mL/minute has been challenged in the literature; limited data suggest that an alternative creatinine clearance threshold may be considered (Oplinger 2013).
Because of the possibility of hemolytic anemia caused by immature erythrocyte enzyme systems (glutathione instability), the drug is contraindicated in pregnant patients at term (38 to 42 weeks gestation), during labor and delivery, or when the onset of labor is imminent; also contraindicated in neonates younger than 1 month of age.
Dosage and Administration
Dosing: Adult
Note: Nitrofurantoin is chemically available as nitrofurantoin macrocrystals and nitrofurantoin monohydrate. Two different preparations are available in the US: A combination of nitrofurantoin monohydrate and nitrofurantoin macrocrystals (Macrobid), which is typically dosed twice daily for the treatment of acute infections and a preparation that consists solely of nitrofurantoin macrocrystals (Furadantin, Macrodantin), which is typically dosed 4 times daily for the treatment of acute infections. Regardless of the formulation used, advise patients to administer with food to improve absorption.
Bacteriuria (≥105 CFU per mL), asymptomatic, in pregnancy (off-label use):
Note: Use during the first trimester should be limited to situations where no alternative therapies are available (ACOG 717 2017; Nordeng 2013); use is contraindicated in pregnant patients at term (38 to 42 weeks' gestation), during labor and delivery, or when the onset of labor is imminent.
Nitrofurantoin monohydrate/macrocrystals (Macrobid): Oral: 100 mg twice daily for 4 to 7 days (ACOG 782 2019; Hooton 2019c; IDSA [Nicolle 2019]; Lumbiganon 2009).
Cystitis, acute uncomplicated or acute simple, treatment:
Note: Consider use of a different empiric agent in patients with suspected pyelonephritis, patients who have received nitrofurantoin in the last 3 months, or patients who have had a urine isolate with documented resistance to nitrofurantoin in the last 3 months (Hooton 2019a; Hooton 2019b; IDSA [Gupta 2011]).
Nitrofurantoin monohydrate/macrocrystals (Macrobid): Oral: 100 mg twice daily; treat females for 5 days (Gupta 2007; IDSA [Gupta 2011]) and males for 7 days (based on expert opinion; Hooton 2019b).
Nitrofurantoin macrocrystals (Furadantin, Macrodantin): Oral: 50 to 100 mg every 6 hours; treat females for 5 days (Gupta 2007; IDSA [Gupta 2011]) and males for 7 days (Hooton 2019b). Note: The recommended duration of therapy with this formulation is based on the recommendation for the nitrofurantoin monohydrate/macrocrystal formulation as well as expert opinion.
Cystitis, recurrent, prophylaxis:
Note: Prophylaxis may be considered in nonpregnant women with bothersome, recurrent uncomplicated cystitis despite non-antimicrobial preventive measures (Albert 2004; Muller 2017). The ideal antibiotic for prophylaxis, as well as the optimal dose, schedule, and duration has not been determined; choice of antibiotic should take into account community patterns of resistance and patient-specific factors (eg, prior efficacy, cost) (Ahmed 2017; Albert 2004; Muller 2017). Prolonged use (>6 months) of nitrofurantoin has been associated with diffuse interstitial pneumonitis and/or pulmonary fibrosis, chronic hepatitis, and the development of neuropathy (Holmberg 1980; manufacturer's labeling).
Continuous prophylaxis:
Nitrofurantoin monohydrate/macrocrystals (Macrobid) (off-label use): Oral: 100 mg once daily at bedtime (Rogers 2004).
Nitrofurantoin macrocrystals (Furadantin, Macrodantin): Oral: 50 to 100 mg once daily at bedtime.
Postcoital prophylaxis: Females with cystitis temporally related to sexual intercourse:
Nitrofurantoin monohydrate/macrocrystals (Macrobid) (off-label use): Oral: 100 mg as a single dose taken within 2 hours of sexual intercourse (Pfau 1983; Rogers 2004; Sen 2008).
Nitrofurantoin macrocrystals (Furadantin, Macrodantin): Oral: 50 to 100 mg as a single dose taken within 2 hours of sexual intercourse (Pfau 1983; Sen 2008).
Dosing: Geriatric
Avoid use; alternative agents preferred. Refer to adult dosing.
Dosing: Pediatric
Urinary tract infection (UTI), treatment:
Furadantin, Macrodantin: Infants, Children, and Adolescents: Oral: 5 to 7 mg/kg/day divided every 6 hours for 7 days or at least 3 days after obtaining sterile urine; maximum dose: 100 mg/dose
Fixed dosing: Furadantin oral suspension: Oral:
7 to <12 kg: 12.5 mg every 6 hours
12 to < 22 kg: 25 mg every 6 hours
22 to <31 kg: 37.5 mg every 6 hours
31 to <42 kg: 50 mg every 6 hours
≥42 kg: 50 to 100 mg every 6 hours
Macrobid (macrocrystal/monohydrate): Adolescents: Oral: 100 mg every 12 hours for 7 days
UTI, prophylaxis: Furadantin, Macrodantin: Infants, Children, and Adolescents: Oral: 1 to 2 mg/kg/day in a single dose (at bedtime) or divided twice daily; maximum daily dose: 100 mg/day. Note: In infants and children <24 months, prophylaxis should only be considered for those with grade III-V reflux or with recurrent febrile UTI; data supporting the routine use of continuous antimicrobial prophylaxis is limited (AAP 2016; AAP [Finnell 2011])
Administration
Oral: Administer with meals to improve absorption and decrease adverse effects; suspension may be mixed with water, milk, or fruit juice. Shake suspension well before use. The monohydrate/macrocrystals capsules (twice-daily formulation [Macrobid]) should not be opened; the macrocrystals capsules (4-times-daily formulation [Macrodantin]) may be opened and the contents mixed with food or juice for immediate use (data on file from manufacturer).
Dietary Considerations
Take with meals to improve absorption and decrease adverse effects.
Storage
Capsules: Store at controlled room temperature, 15°C to 30°C (59°F to 86°F). Dispense in a tight container using a child-resistant closure.
Oral suspension: Avoid exposure to strong light, which may darken the drug. It is stable when stored between 20°C and 25°C (68°F and 77°F). Protect from freezing. Dispense in glass amber bottles.
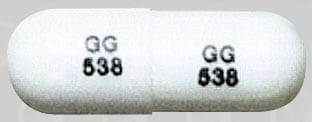
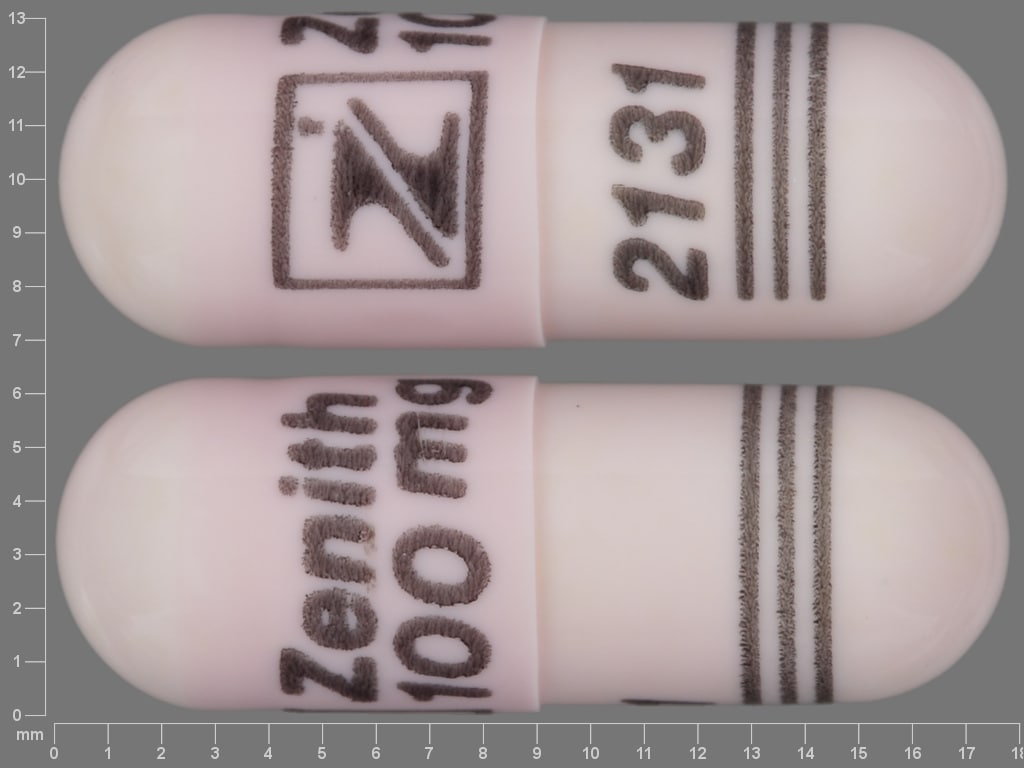
Nitrofurantoin Images
Drug Interactions
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Eplerenone: Nitrofurantoin may enhance the hyperkalemic effect of Eplerenone. Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Magnesium Trisilicate: May decrease the serum concentration of Nitrofurantoin. Avoid combination
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Norfloxacin: Nitrofurantoin may diminish the therapeutic effect of Norfloxacin. Avoid combination
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Probenecid: May increase the serum concentration of Nitrofurantoin. Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Test Interactions
False-positive urine glucose (Benedict's and Fehling's methods); no false positives with enzymatic tests
Adverse Reactions
1% to 10%:
Central nervous system: Headache (6%)
Endocrine & metabolic: Increased serum phosphate (1% to 5%)
Gastrointestinal: Nausea (8%), flatulence (2%)
Hematologic & oncologic: Decreased hemoglobin (1% to 5%), eosinophilia (1% to 5%)
Hepatic: Increased serum alanine aminotransferase (1% to 5%), increased serum aspartate aminotransferase (1% to 5%)
Frequency not defined:
Cardiovascular: Bundle branch block, chest pain, ECG changes, nonspecific T wave on ECG, vasculitis
Central nervous system: Bulging fontanel (infants), confusion, depression, drug fever, peripheral neuropathy, pseudotumor cerebri, psychotic reaction, vertigo
Dermatologic: Eczematous rash, erythema multiforme, erythematous maculopapular rash, exfoliative dermatitis, maculopapular rash, skin rash, Stevens-Johnson syndrome
Gastrointestinal: Anorexia, clostridioides, Clostridium difficile colitis, pancreatitis, sialadenitis, vomiting
Genitourinary: Urine discoloration
Hematologic & oncologic: Agranulocytosis, aplastic anemia, glucose-6-phosphate dehydrogenase deficiency anemia, granulocytopenia, hemolytic anemia, leukopenia, megaloblastic anemia, methemoglobinemia, thrombocytopenia
Hepatic: Cholestatic jaundice, chronic active hepatitis, hepatic necrosis, hepatitis
Hypersensitivity: Anaphylaxis, angioedema, hypersensitivity reaction
Infection: Superinfection
Neuromuscular & skeletal: Arthralgia, asthenia, lupus-like syndrome, myalgia
Ophthalmic: Nystagmus
Respiratory: Acute pulmonary reaction, chronic pulmonary reaction, cough, cyanosis, dyspnea, dyspnea on exertion, interstitial pneumonitis, pleural effusion, pulmonary fibrosis, pulmonary infiltrates
<1%, postmarketing, and/or case reports: Abdominal pain, alopecia, amblyopia, chills, constipation, diarrhea, dizziness, drowsiness, dyspepsia, fever, hepatotoxicity, malaise, optic neuritis, pruritus, pulmonary hypersensitivity, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Hepatic reactions: Rare, but severe and sometimes fatal hepatic reactions (eg, cholestatic jaundice, hepatitis, hepatic necrosis) have been associated with use (onset may be insidious); discontinue immediately if hepatitis occurs. Monitor liver function tests periodically. Use is contraindicated in patients with a history of nitrofurantoin associated cholestatic jaundice or hepatic dysfunction.
- Optic neuritis: Postmarketing cases of optic neuritis have been reported.
- Peripheral neuropathy: Has been associated with peripheral neuropathy (rare); risk may be increased in patients with anemia, renal impairment (CrCl <60 mL/minute), diabetes, vitamin B deficiency, debilitating disease, or electrolyte imbalance; use caution.
- Pulmonary toxicity: Acute, subacute, or chronic (usually after 6 months of therapy) pulmonary reactions (possibly fatal) have been observed; if these occur, discontinue therapy immediately. Monitor closely for malaise, dyspnea, cough, fever, radiologic evidence of diffuse interstitial pneumonitis or fibrosis.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months post antibiotic treatment.
Disease-related concerns:
- Hemolytic anemia: Use caution in patients with G6PD deficiency; may be at increased risk for hemolytic anemia. Discontinue therapy if occurs.
- Renal impairment: Urinary nitrofurantoin concentrations are variable in patients with impaired renal function. The manufacturer contraindicates use in CrCl <60 mL/minute; however, limited data suggest nitrofurantoin is safe and effective for short-term treatment of uncomplicated UTI in patients with CrCl 30 to 60 mL/minute (Cuhna 2017; Oplinger 2013; Santos 2016; Singh 2015). The Beers Criteria recommends avoiding use in geriatric patients ≥65 years with a CrCl <30 mL/minute (Beers Criteria [AGS 2019]).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Sedatives: Effects may be potentiated when used with other sedative drugs or ethanol.
Special populations:
- Elderly: Use in elderly patients, particularly females receiving long-term prophylaxis for recurrent UTIs, has also been associated with an increased risk of hepatic and pulmonary toxicity and peripheral neuropathy. Monitor closely for toxicities during use.
- Pediatric: Use is contraindicated in children <1 month of age (at increased risk for hemolytic anemia).
Other warnings/precautions:
- Appropriate use: Pyelonephritis: Not indicated for the treatment of pyelonephritis or perinephric abscesses.
Monitoring Parameters
Signs of pulmonary reaction; signs of numbness or tingling of the extremities; CBC, periodic liver function tests, periodic renal function tests with long-term use
Pregnancy
Pregnancy Risk Factor
B (contraindicated at term)
Pregnancy Considerations
Nitrofurantoin crosses the placenta (Perry 1967).
Current studies evaluating maternal use of nitrofurantoin during pregnancy and the development of birth defects have had mixed results (ACOG 717 2017). An increased risk of neonatal jaundice was observed following maternal nitrofurantoin use during the last 30 days of pregnancy (Nordeng 2013).
Maternal serum concentrations of nitrofurantoin may be decreased in pregnancy (Philipson 1979). Use of nitrofurantoin may be considered for the treatment of asymptomatic bacteriuria in pregnancy (Nicolle [IDSA 2019]). Nitrofurantoin may be used to treat infections during pregnancy; use during the first trimester should be limited to situations where no alternative therapies are available. Prescriptions should be written when clinically appropriate and for the shortest effective duration for confirmed infections (ACOG 717 2017). Nitrofurantoin is contraindicated in pregnant patients at term (38 to 42 weeks' gestation), during labor and delivery, or when the onset of labor is imminent due to the possibility of hemolytic anemia in the neonate. Alternative antibiotics should be used in pregnant patients with G-6-PD deficiency (ACOG 717 2017; Nordeng 2013).
Patient Education
What is this drug used for?
- It is used to treat or prevent a urinary tract infection (UTI).
Frequently reported side effects of this drug
- Headache
- Nausea
- Vomiting
- Diarrhea
- Lack of appetite
- Abdominal pain
- Dizziness
- Fatigue
- Hair loss
- Urine discoloration
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Nerve problems like sensitivity to heat or cold; decreased sense of touch; burning, numbness, or tingling; pain, or weakness in the arms, hands, legs, or feet
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Severe pulmonary disorder like lung or breathing problems like difficulty breathing, shortness of breath, or a cough that is new or worse
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs
- Involuntary eye movements
- Severe loss of strength and energy
- Clostridioides (formerly Clostridium) -associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.