Boxed Warning
Suicidality in children and adolescents:
Antidepressants increased the risk compared with placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of nortriptyline or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared with placebo in adults older than 24 years; there was a reduction in risk with antidepressants compared with placebo in adults 65 years and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Appropriately monitor patients of all ages who are started on antidepressant therapy and observe them closely for clinical worsening, suicidality, or unusual changes in behavior. Advise families and caregivers of the need for close observation and communication with the health care provider. Nortriptyline is not approved for use in pediatric patients.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Pamelor: 10 mg, 25 mg [contains fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Pamelor: 50 mg
Pamelor: 75 mg [contains fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Generic: 10 mg, 25 mg, 50 mg, 75 mg
Solution, Oral:
Generic: 10 mg/5 mL (10 mL [DSC], 473 mL)
Pharmacology
Mechanism of Action
Traditionally believed to increase the synaptic concentration of serotonin and/or norepinephrine in the central nervous system by inhibition of their reuptake by the presynaptic neuronal membrane. Inhibits the activity of histamine, 5-hydroxytryptamine, and acetylcholine. It increases the pressor effect of norepinephrine but blocks the pressor response of phenethylamine. However, additional receptor effects have been found including desensitization of adenyl cyclase, down regulation of beta-adrenergic receptors, and down regulation of serotonin receptors.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapid (Alexanderson 1972)
Distribution
Vd: 21.1 to 31.1 L/kg (Alexanderson 1972)
Metabolism
Primarily hepatic; extensive first-pass effect (Rubin 1985)
Excretion
Urine (as metabolites and small amounts of unchanged drug) (Alexanderson 1972)
Onset of Action
Depression: Individual responses may vary; however, 4 to 8 weeks of treatment are needed before determining if a patient with depression is partially or non-responsive (APA 2010)
Time to Peak
Serum: 4 to 9 hours (Alexanderson 1972)
Half-Life Elimination
Adults: 14 to 51 hours (mean: 26 hours) (Dawling 1980)
Elderly: 23.5 to 79 hours (mean: 45 hours) (Dawling 1980)
Protein Binding
Extensively bound to plasma proteins (Alexanderson 1972)
Use: Labeled Indications
Major depression, unipolar: Treatment of symptoms of unipolar major depression
Use: Off Label
Chronic paincyes
Data from a limited number of patients in a randomized, double-blind, placebo-controlled study and a retrospective chart review suggest that nortriptyline may be beneficial for the treatment of chronic pain Atkinson 1998, Orbai 2010. Additional data may be necessary to further define the role of nortriptyline in this condition.
Based on the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine Practice Guidelines for Chronic Pain Management, nortriptyline, as well as other tricyclic antidepressants, is effective and recommended for pain relief in a variety of chronic pain etiologies. The American Pain Society lists tricyclic antidepressants as co-analgesics in the management of pain (eg, neuropathic pain) APS.2008.
Diabetic neuropathycyes
Data from a limited number of patients in a controlled trial suggest that nortriptyline may be beneficial for the treatment of neuropathic pain, including diabetic neuropathy Gilron 2009.
Based on the American Diabetes Association position statement for the treatment of diabetic neuropathy, TCAs, including nortriptyline, are effective and recommended in the management of diabetic neuropathy, but should be used with caution due to the risk for cardiovascular adverse effects
Myofascial paincyes
Data from a limited number of patients in an open-label trial comparing the use of amitriptyline to nortriptyline suggests that nortriptyline may be beneficial for the treatment of patients with myofascial pain (Haviv 2015). In addition, clinical experience suggests the utility of tricyclic antidepressants in the management of myofascial pain when conventional treatments have failed Desai 2013, Graff-Radford 2004.
Based on the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine Practice Guidelines for Chronic Pain Management, nortriptyline, as well as other tricyclic antidepressants, is effective and recommended for pain relief in a variety of chronic pain etiologies.
Orofacial painc
Clinical experience suggests the utility of nortriptyline in the management of orofacial pain Feinmann 1993, Romero-Reyes 2014. Additional data may be necessary to further define the role of nortriptyline in the management of orofacial pain.
Postherpetic neuralgiabyes
Data from a limited number of patients in controlled trials suggest that nortriptyline may be beneficial for pain relief in the treatment of postherpetic neuralgia (PHN) Chandra 2006, Raja 2002, Watson 1998.
Based on
Smoking cessationbyes
Data from controlled trials and meta-analyses indicate that nortriptyline is effective in promoting smoking cessation.
Guidelines from the US Preventative Task Force (USPSTF) and from the Public Health Service (PHS), along with a therapeutic position statement from the American Society of Health-System Pharmacists (ASHP) recommend behavioral interventions combined with FDA-approved pharmacotherapy (eg, nicotine, bupropion, varenicline) for smoking cessation. PHS and ASHP guidelines also state that nortriptyline or clonidine may be considered as second-line therapies.
Contraindications
Hypersensitivity to nortriptyline and similar chemical class dibenzazepines, or any component of the formulation; use in a patient during the acute recovery phase of MI; use of MAO inhibitors intended to treat psychiatric disorders (concurrently or within 14 days of discontinuing either nortriptyline or the MAO inhibitor); initiation of nortriptyline in a patient receiving linezolid or intravenous methylene blue
Dosage and Administration
Dosing: Adult
Major depression, unipolar: Oral: Initial: 25 mg once daily (APA 2010); adjust dose based on response and tolerability to a usual dose of 25 mg 3 to 4 times/day; total daily doses may be given once daily. Maximum: 150 mg/day.
Chronic pain (off-label use): Oral: Initial: 10 to 25 mg once daily at bedtime; may increase as tolerated as soon as every 3 days up to 150 mg/day (APS 2008; Atkinson 1998; Orbai 2010). Patients with neuropathic pain and an inadequate response to nortriptyline alone may benefit from a combination with gabapentin (Gilron 2009).
Diabetic neuropathy (off-label use): Oral: Initial: 10 to 25 mg/day; may gradually increase based on response and tolerability to a target dose of 25 to 100 mg/day. Additional data may be necessary to further define the role of nortriptyline in this condition (ADA [Pop-Busui 2017].
Myofascial pain (off-label use): Oral: Initial: 12.5 mg once daily at bedtime; may increase as tolerated up to 35 mg/day. If after 4 weeks at 25 to 35 mg/day there is no change in pain intensity, then consider alternative therapy (Haviv 2015).
Orofacial pain (off-label use): Oral: Initial: 10 to 30 mg once daily at bedtime; gradually titrated up to 100 mg/day as tolerated (Feinmann 1993; Romero-Reyes 2014).
Postherpetic neuralgia (off-label use): Oral: Initial: 10 to 20 mg once daily at bedtime; may increase as needed every 3 to 5 days in 10 mg once daily increments up to 160 mg/day (Raja 2002; Watson 1998).
Smoking cessation (off-label use): Oral: Initial: 25 mg once daily begun 10 to 28 days prior to selected “quit” date; titrate dose to 75 to 100 mg/day; continue therapy for ≥12 weeks after “quit” day (PHS 2008)
Discontinuation of therapy:When discontinuing antidepressant treatment that has lasted for >3 weeks, gradually taper the dose (eg, over 2 to 4 weeks) to minimize withdrawal symptoms and detect reemerging symptoms (APA 2010; WFSBP [Bauer 2015]). Reasons for a slower titration (eg, over 4 weeks) include use of a drug with a half-life <24 hours (eg, paroxetine, venlafaxine), prior history of antidepressant withdrawal symptoms, or high doses of antidepressants (APA 2010; Hirsch 2019). If intolerable withdrawal symptoms occur, resume the previously prescribed dose and/or decrease dose at a more gradual rate (Shelton 2001). Select patients (eg, those with a history of discontinuation syndrome) on long-term treatment (>6 months) may benefit from tapering over >3 months (WFSBP [Bauer 2015]). Evidence supporting ideal taper rates is limited (Shelton 2001; WFSBP [Bauer 2015]).
MAO inhibitor recommendations:
Switching to or from an MAO inhibitor intended to treat psychiatric disorders:
Allow 14 days to elapse between discontinuing an MAO inhibitor intended to treat psychiatric disorders and initiation of nortriptyline.
Allow 14 days to elapse between discontinuing nortriptyline and initiation of an MAO inhibitor intended to treat psychiatric disorders.
Dosing: Geriatric
Depression: Oral: Initial: 30 to 50 mg/day, given as a single daily dose or in divided doses.
Discontinuation of therapy: Refer to adult dosing.
MAO inhibitor recommendations: Refer to adult dosing.
Dosing: Pediatric
Attention-deficit/hyperactivity disorder (ADHD): Limited data available: Note: Should not be used first-line; use should be reserved for cases where other therapies have failed or not tolerated (AACAP [Pliszka 2007]; Dopheide 2005).
Children ≥6 years and Adolescents: Oral: Initial: 0.5 mg/kg/day; may increase by 0.5 mg/kg/day increments at weekly intervals; maximum daily dose: 2 mg/kg/day up to 100 mg/day (AACAP [Pliszka 2007]; Prince 2000; Spencer 1996; Wilens 1993); in one trial, the daily dose was divided twice daily with a dose administered before school and a dose after dinner; reported mean effective dose: 1.8 mg/kg/day (Prince 2000).
Enuresis: Limited data available: Note: Due to the risk of serious side effects (eg, arrhythmias, heart block, seizures), TCAs are considered third line treatment for enuresis; may consider use in patients who have failed all other therapies; high relapse rate when discontinued (Deshpande 2012; Kliegman 2007). Administer dose 30 minutes before bedtime; usual treatment duration: ≤3 months.
Children ≥6 years and Adolescents: Oral: General dosing: Initial: 10 to 20 mg/day; titrate up to maximum daily dose of 40 mg/day (Kliegman 2007).
Depression: Oral: Note: Controlled clinical trials have not shown tricyclic antidepressants to be superior to placebo for the treatment of depression in children and adolescents; not recommended as first line medication; may be beneficial for patient with comorbid conditions (ADHD enuresis) (AACAP [Birmaher 2007]; Dopheide 2006; Wagner 2005).
Children 6 to 12 years: Limited data available: 1 to 3 mg/kg/day in 4 divided doses; maximum daily dose: 150 mg/day (Kliegman 2007).
Adolescents: 30 to 50 mg/day in 3 to 4 divided doses or as a single daily dose; maximum daily dose: 150 mg/day.
Neuropathic pain: Limited data available: Children and Adolescents: Oral: Usual range: 0.05 to 1 mg/kg/dose at bedtime; begin at the lower end of dosing range and titrate every 3 days to effect; the analgesic effects of TCA's are typically observed at a lower dose compared to TCA doses for depression; maximum daily dose: 3 mg/kg/day or 150 mg/day, whichever is less (APS 2016; Kliegman 2011).
Discontinuation of therapy: Consider planning antidepressant discontinuation for lower-stress times, recognizing non-illness-related factors could cause stress or anxiety and be misattributed to antidepressant discontinuation (Hathaway 2018). Upon discontinuation of antidepressant therapy, gradually taper the dose to minimize the incidence of discontinuation syndromes (withdrawal) and allow for the detection of reemerging disease state symptoms (eg, relapse). Evidence supporting ideal taper rates after illness remission is limited. APA and NICE guidelines suggest tapering therapy over at least several weeks with consideration to the half-life of the antidepressant; antidepressants with a shorter half-life may need to be tapered more conservatively. After long-term (years) antidepressant treatment, WFSBP guidelines recommend tapering over 4 to 6 months, with close monitoring during and for 6 months after discontinuation. If intolerable discontinuation symptoms occur following a dose reduction, consider resuming the previously prescribed dose and/or decrease dose at a more gradual rate (APA 2010; Bauer 2002; Fenske 2009; Haddad 2001; NCCMH 2010; Schatzberg 2006; Shelton 2001; Warner 2006).
MAO inhibitor recommendations:
Switching to or from an MAO inhibitor intended to treat psychiatric disorders:
Allow 14 days to elapse between discontinuing an MAO inhibitor intended to treat psychiatric disorders and initiation of nortriptyline.
Allow 14 days to elapse between discontinuing nortriptyline and initiation of an MAO inhibitor intended to treat psychiatric disorders.
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from light.
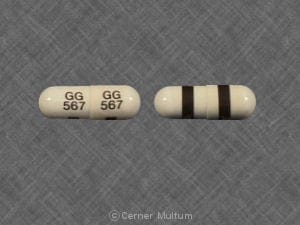
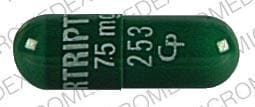
Nortriptyline Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Almotriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Alosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Alpha-/Beta-Agonists: Tricyclic Antidepressants may enhance the vasopressor effect of Alpha-/Beta-Agonists. Management: Avoid, if possible, the use of alpha-/beta-agonists in patients receiving tricyclic antidepressants. If combined, monitor for evidence of increased pressor effects and consider reductions in initial dosages of the alpha-/beta-agonist. Consider therapy modification
Alpha1-Agonists: Tricyclic Antidepressants may enhance the therapeutic effect of Alpha1-Agonists. Tricyclic Antidepressants may diminish the therapeutic effect of Alpha1-Agonists. Monitor therapy
Alpha2-Agonists: Tricyclic Antidepressants may diminish the antihypertensive effect of Alpha2-Agonists. Management: Consider avoiding this combination. If used, monitor for decreased effects of the alpha2-agonist. Exercise great caution if discontinuing an alpha2-agonist in a patient receiving a TCA. Exceptions: Apraclonidine; Brimonidine (Ophthalmic); Lofexidine. Consider therapy modification
Alpha2-Agonists (Ophthalmic): Tricyclic Antidepressants may diminish the therapeutic effect of Alpha2-Agonists (Ophthalmic). Monitor therapy
Altretamine: May enhance the orthostatic hypotensive effect of Tricyclic Antidepressants. Monitor therapy
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Amphetamines: Tricyclic Antidepressants may enhance the adverse/toxic effect of Amphetamines. Tricyclic Antidepressants may potentiate the cardiovascular effects of Amphetamines. Amphetamines may enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased cardiovascular effects when these agents are combined. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Antiemetics (5HT3 Antagonists): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Alosetron; Ondansetron; Ramosetron. Monitor therapy
Antipsychotic Agents: Serotonergic Agents (High Risk) may enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, serotonergic agents may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotic Agents may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: May increase the metabolism of Tricyclic Antidepressants. Consider therapy modification
Beta2-Agonists: Tricyclic Antidepressants may enhance the adverse/toxic effect of Beta2-Agonists. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the adverse/toxic effect of Tricyclic Antidepressants. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
BusPIRone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: May decrease the serum concentration of Tricyclic Antidepressants. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Cimetidine: May decrease the metabolism of Tricyclic Antidepressants. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Cinacalcet: May increase the serum concentration of Tricyclic Antidepressants. Management: Seek alternatives when possible. If these combinations are used, monitor closely for increased effects/toxicity and/or elevated serum concentrations (when testing is available) of the tricyclic antidepressant. Consider therapy modification
Citalopram: Tricyclic Antidepressants may enhance the serotonergic effect of Citalopram. Tricyclic Antidepressants may increase the serum concentration of Citalopram. Citalopram may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA and citalopram concentrations/effects. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Cocaine (Topical): May enhance the adverse/toxic effect of Tricyclic Antidepressants. Monitor therapy
Cyclobenzaprine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Dapoxetine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Do not use serotonergic agents (high risk) with dapoxetine or within 7 days of serotonergic agent discontinuation. Do not use dapoxetine within 14 days of monoamine oxidase inhibitor use. Dapoxetine labeling lists this combination as contraindicated. Avoid combination
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Desmopressin: Tricyclic Antidepressants may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dexmethylphenidate-Methylphenidate: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Dextromethorphan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Dronedarone: Tricyclic Antidepressants may enhance the arrhythmogenic effect of Dronedarone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
DULoxetine: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. DULoxetine may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations and effects if these agents are combined. Monitor therapy
Eletriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Ergot Derivatives: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Nicergoline. Monitor therapy
Escitalopram: Tricyclic Antidepressants may enhance the serotonergic effect of Escitalopram. Escitalopram may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Fexinidazole [INT]: Tricyclic Antidepressants may enhance the QTc-prolonging effect of Fexinidazole [INT]. Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
FLUoxetine: May enhance the serotonergic effect of Tricyclic Antidepressants. FLUoxetine may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Consider therapy modification
FluvoxaMINE: May enhance the serotonergic effect of Tricyclic Antidepressants. FluvoxaMINE may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Monitor therapy
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Guanethidine: Tricyclic Antidepressants may diminish the therapeutic effect of Guanethidine. Monitor therapy
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Iobenguane Radiopharmaceutical Products: Tricyclic Antidepressants may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lasmiditan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Linezolid: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Avoid combination
Lofexidine: Tricyclic Antidepressants may diminish the therapeutic effect of Lofexidine. Management: Consider avoiding this drug combination when possible. If concurrent administration is required, monitor blood pressure carefully at the beginning of the combined therapy and when either drug is stopped. Adjust the dosage accordingly. Consider therapy modification
Lorcaserin: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Lorcaserin may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations and effects if these agents are combined. Monitor therapy
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Metaxalone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylene Blue: Tricyclic Antidepressants may enhance the serotonergic effect of Methylene Blue. This could result in serotonin syndrome. Avoid combination
Metoclopramide: May enhance the adverse/toxic effect of Tricyclic Antidepressants. Management: Seek alternatives to this combination when possible. Monitor patients receiving metoclopramide with tricyclic antidepressants for signs of extrapyramidal symptoms, neuroleptic malignant syndrome, and serotonin syndrome. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
MetyroSINE: May enhance the adverse/toxic effect of Tricyclic Antidepressants. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Monoamine Oxidase Inhibitors (Antidepressant): May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Avoid combination
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nefazodone: Tricyclic Antidepressants may enhance the serotonergic effect of Nefazodone. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Nicorandil: Tricyclic Antidepressants may enhance the hypotensive effect of Nicorandil. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Ondansetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Oxitriptan: Serotonergic Agents (High Risk) may enhance the serotonergic effect of Oxitriptan. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
PARoxetine: May enhance the serotonergic effect of Tricyclic Antidepressants. PARoxetine may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Consider therapy modification
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pitolisant: Tricyclic Antidepressants may diminish the therapeutic effect of Pitolisant. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Protease Inhibitors: May increase the serum concentration of Tricyclic Antidepressants. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QuiNIDine: Tricyclic Antidepressants may enhance the QTc-prolonging effect of QuiNIDine. QuiNIDine may increase the serum concentration of Tricyclic Antidepressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Ramosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Rasagiline: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Avoid combination
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Safinamide: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Avoid combination
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Selegiline: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Avoid combination
Serotonergic Agents (High Risk, Miscellaneous): Tricyclic Antidepressants may enhance the serotonergic effect of Serotonergic Agents (High Risk, Miscellaneous). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Serotonergic Non-Opioid CNS Depressants: Tricyclic Antidepressants may enhance the CNS depressant effect of Serotonergic Non-Opioid CNS Depressants. Tricyclic Antidepressants may enhance the serotonergic effect of Serotonergic Non-Opioid CNS Depressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and CNS depression when these agents are combined. Monitor therapy
Serotonergic Opioids (High Risk): Tricyclic Antidepressants may enhance the CNS depressant effect of Serotonergic Opioids (High Risk). Serotonergic Opioids (High Risk) may enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity and CNS depression. Consider therapy modification
Serotonin 5-HT1D Receptor Agonists (Triptans): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Almotriptan; Eletriptan. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes when these agents are combined. Exceptions: DULoxetine. Monitor therapy
Sertraline: May enhance the serotonergic effect of Tricyclic Antidepressants. Sertraline may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Sodium Phosphates: Tricyclic Antidepressants may enhance the adverse/toxic effect of Sodium Phosphates. Specifically, the risk of seizure and/or loss of consciousness may be increased in patients with significant sodium phosphate induced fluid/electrolyte abnormalities. Monitor therapy
St John's Wort: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. St John's Wort may decrease the serum concentration of Serotonergic Agents (High Risk). Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Sulfonylureas: Cyclic Antidepressants may enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Syrian Rue: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Terbinafine (Systemic): May increase the serum concentration of Nortriptyline. Management: Monitor for increased effects/toxicity of nortriptyline during concomitant administration with terbinafine. Reduced dosages of nortriptyline may be needed. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thyroid Products: May enhance the arrhythmogenic effect of Tricyclic Antidepressants. Thyroid Products may enhance the stimulatory effect of Tricyclic Antidepressants. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Tobacco (Smoked): May decrease the serum concentration of Nortriptyline. Monitor therapy
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Tricyclic Antidepressants: May enhance the anticholinergic effect of other Tricyclic Antidepressants. Tricyclic Antidepressants may enhance the CNS depressant effect of other Tricyclic Antidepressants. Tricyclic Antidepressants may enhance the serotonergic effect of other Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Monitor closely for increased TCA adverse effects, including serotonin syndrome/serotonin toxicity, CNS depression, and anticholinergic effects. Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Valproate Products: May increase the serum concentration of Tricyclic Antidepressants. Monitor therapy
Vilazodone: Tricyclic Antidepressants may enhance the serotonergic effect of Vilazodone. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) if these agents are combined. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Tricyclic Antidepressants may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Vortioxetine: Tricyclic Antidepressants may enhance the serotonergic effect of Vortioxetine. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) if these agents are combined. Monitor therapy
Yohimbine: Tricyclic Antidepressants may increase the serum concentration of Yohimbine. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
Some reactions listed are based on reports for other agents in this same pharmacologic class and may not be specifically reported for nortriptyline.
Frequency not defined:
Cardiovascular: Acute myocardial infarction, cardiac arrhythmia, cerebrovascular accident, edema, flushing, heart block, hypertension, hypotension, palpitations, tachycardia
Central nervous system: Agitation, anxiety, ataxia, confusion, delusion, disorientation, dizziness, drowsiness, drug fever, EEG pattern changes, extrapyramidal reaction, fatigue, hallucination, headache, hypomania, insomnia, nightmares, numbness, panic, peripheral neuropathy, psychosis (exacerbation), restlessness, seizure, tingling of extremities, tingling sensation, withdrawal symptoms
Dermatologic: Alopecia, diaphoresis (excessive), pruritus, skin photosensitivity, skin rash, urticaria
Endocrine & metabolic: Decreased libido, decreased serum glucose, galactorrhea not associated with childbirth, gynecomastia, increased libido, increased serum glucose, SIADH, weight gain, weight loss
Gastrointestinal: Abdominal cramps, anorexia, constipation, diarrhea, epigastric distress, melanoglossia, nausea, paralytic ileus, parotid gland enlargement, stomatitis, sublingual adenitis, unpleasant taste, vomiting, xerostomia
Genitourinary: Breast hypertrophy, impotence, nocturia, testicular swelling, urinary hesitancy, urinary retention, urinary tract dilation
Hematologic & oncologic: Agranulocytosis, eosinophilia, petechia, purpuric disease, thrombocytopenia
Hepatic: Abnormal hepatic function tests, cholestatic jaundice
Neuromuscular & skeletal: Asthenia, tremor
Ophthalmic: Accommodation disturbance, blurred vision, eye pain, mydriasis
Otic: Tinnitus
Renal: Polyuria
<1%, postmarketing, and/or case reports: Angle-closure glaucoma, cardiac disorder (unmasking of Brugada syndrome), serotonin syndrome, suicidal ideation, suicidal tendencies
Warnings/Precautions
Major psychiatric warnings:
- Suicidal thinking/behavior: [US Boxed Warning]: Antidepressants increase the risk of suicidal thinking and behavior in children, adolescents, and young adults (18 to 24 years of age) with major depressive disorder (MDD) and other psychiatric disorders; consider risk prior to prescribing. Short-term studies did not show an increased risk in patients >24 years of age and showed a decreased risk in patients ≥65 years. Closely monitor patients for clinical worsening, suicidality, or unusual changes in behavior, particularly during the initial 1 to 2 months of therapy or during periods of dosage adjustments (increases or decreases); the patient's family or caregiver should be instructed to closely observe the patient and communicate condition with healthcare provider. A medication guide concerning the use of antidepressants should be dispensed with each prescription. Nortriptyline is not FDA approved for use in children.
- The possibility of a suicide attempt is inherent in major depression and may persist until remission occurs. Worsening depression and severe abrupt suicidality that are not part of the presenting symptoms may require discontinuation or modification of drug therapy. Use caution in high-risk patients during initiation of therapy.
- Prescriptions should be written for the smallest quantity consistent with good patient care. The patient's family or caregiver should be alerted to monitor patients for the emergence of suicidality and associated behaviors such as anxiety, agitation, panic attacks, insomnia, irritability, hostility, impulsivity, akathisia, hypomania, and mania; patients should be instructed to notify their healthcare provider if any of these symptoms or worsening depression or psychosis occur.
Concerns related to adverse effects:
- Anticholinergic effects: May cause anticholinergic effects (constipation, xerostomia, blurred vision, urinary retention); use with caution in patients with decreased gastrointestinal motility, paralytic ileus, urinary retention, BPH, xerostomia, or visual problems. The degree of anticholinergic blockade produced by this agent is moderate relative to other antidepressants (APA 2010).
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving). The degree of sedation is low-moderate relative to other antidepressants (Bauer 2013).
- Fractures: Bone fractures have been associated with antidepressant treatment. Consider the possibility of a fragility fracture if an antidepressant-treated patient presents with unexplained bone pain, point tenderness, swelling, or bruising (Rabenda 2013; Rizzoli 2012).
- Hematologic effects: TCAs may rarely cause bone marrow suppression; monitor for any signs of infection and obtain CBC if symptoms (eg, fever, sore throat) evident.
- Ocular effects: May cause mild pupillary dilation which in susceptible individuals can lead to an episode of narrow-angle glaucoma. Consider evaluating patients who have not had an iridectomy for narrow-angle glaucoma risk factors.
- Orthostatic hypotension: May cause orthostatic hypotension (risk is low relative to other antidepressants); use with caution in patients at risk of this effect or in those who would not tolerate transient hypotensive episodes (cerebrovascular disease, cardiovascular disease, hypovolemia, or concurrent medication use which may predispose to hypotension/bradycardia) (APA 2010).
- Serotonin syndrome: Potentially life-threatening serotonin syndrome (SS) has occurred with serotonergic agents (eg, SSRIs, SNRIs), particularly when used in combination with other serotonergic agents (eg, triptans, TCAs, fentanyl, lithium, tramadol, buspirone, St John wort, tryptophan) or agents that impair metabolism of serotonin (eg, MAO inhibitors intended to treat psychiatric disorders, other MAO inhibitors [ie, linezolid and intravenous methylene blue]). Monitor patients closely for signs of SS such as mental status changes (eg, agitation, hallucinations, delirium, coma); autonomic instability (eg, tachycardia, labile blood pressure, diaphoresis); neuromuscular changes (eg, tremor, rigidity, myoclonus); GI symptoms (eg, nausea, vomiting, diarrhea); and/or seizures. Discontinue treatment (and any concomitant serotonergic agent) immediately if signs/symptoms arise.
- Syndrome of inappropriate antidiuretic hormone secretion and hyponatremia: Antidepressant agents have been associated with the development of syndrome of inappropriate antidiuretic hormone secretion and hyponatremia, predominately in the elderly. Other risk factors include volume depletion, concurrent use of diuretics, female gender, low body weight, and severe physical illness. TCAs have a lower risk for hyponatremia in comparison to SSRIs (De Picker 2014).
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with a history of cardiovascular disease (including previous MI, stroke, tachycardia, or conduction abnormalities); in general, avoid use in patients with or suspected of having Brugada syndrome. The risk of conduction abnormalities with this agent is moderate relative to other antidepressants (APA 2010).
- Diabetes: Use with caution in patients with diabetes mellitus; may alter glucose regulation (APA 2010).
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Mania/hypomania: May precipitate a shift to mania or hypomania in patients with bipolar disorder. Monotherapy in patients with bipolar disorder should be avoided. Patients presenting with depressive symptoms should be screened for bipolar disorder including details regarding family history of suicide, bipolar disorder, and depression. Nortriptyline is not FDA approved for the treatment of bipolar depression.
- Renal impairment: Use with caution in patients with renal impairment.
- Seizure disorder: Use with caution in patients with a history of seizures.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
Other warnings/precautions:
- Discontinuation syndrome: Abrupt discontinuation or interruption of antidepressant therapy has been associated with a discontinuation syndrome. Symptoms arising may vary with antidepressant however commonly include nausea, vomiting, diarrhea, headaches, lightheadedness, dizziness, diminished appetite, sweating, chills, tremors, paresthesias, fatigue, somnolence, and sleep disturbances (eg, vivid dreams, insomnia). Less common symptoms include electric shock-like sensations, cardiac arrhythmias (more common with tricyclic antidepressants), myalgias, parkinsonism, arthralgias, and balance difficulties. Psychological symptoms may also emerge such as agitation, anxiety, akathisia, panic attacks, irritability, aggressiveness, worsening of mood, dysphoria, mood lability, hyperactivity, mania/hypomania, depersonalization, decreased concentration, slowed thinking, confusion, and memory or concentration difficulties. Greater risks for developing a discontinuation syndrome have been associated with antidepressants with shorter half-lives, longer durations of treatment, and abrupt discontinuation. For antidepressants of short or intermediate half-lives, symptoms may emerge within 2 to 5 days after treatment discontinuation and last 7 to 14 days (APA 2010; Fava 2006; Haddad 2001; Shelton 2001; Warner 2006).
- Electroconvulsive therapy: May increase the risks associated with electroconvulsive therapy (ECT); consider discontinuing, when possible, prior to ECT treatment.
- Surgery: Recommended by the manufacturer to discontinue prior to elective surgery; risks exist for drug interactions with anesthesia and for cardiac arrhythmias. However, definitive drug interactions have not been widely reported in the literature and continuation of tricyclic antidepressants is generally recommended as long as precautions are taken to reduce the significance of any adverse events that may occur. Norepinephrine should be considered the vasopressor of choice for TCA-related hypotension (Pass 2004). Therapy should not be abruptly discontinued in patients receiving high doses for prolonged periods.
Monitoring Parameters
Serum sodium in at-risk populations (as clinically indicated), blood pressure, heart pulse rate and ECG in older adults and patients with preexisting cardiac disease; blood glucose; weight and BMI; therapeutic blood levels (as clinically indicated); suicide ideation (especially at the beginning of therapy or when doses are increased or decreased) (APA 2010; De Picker 2014)
Pregnancy
Pregnancy Considerations
Nortriptyline and its metabolites cross the human placenta and can be detected in cord blood (Loughhead 2006). Tricyclic antidepressants may be associated with irritability, jitteriness, and convulsions (rare) in the neonate (Yonkers 2009).
The ACOG recommends that therapy for depression during pregnancy be individualized; treatment should incorporate the clinical expertise of the mental health clinician, obstetrician, primary health care provider, and pediatrician (ACOG 2008). According to the American Psychiatric Association (APA), the risks of medication treatment should be weighed against other treatment options and untreated depression. For women who discontinue antidepressant medications during pregnancy and who may be at high risk for postpartum depression, the medications can be restarted following delivery (APA 2010). Treatment algorithms have been developed by the ACOG and the APA for the management of depression in women prior to conception and during pregnancy (Yonkers 2009).
Pregnant women exposed to antidepressants during pregnancy are encouraged to enroll in the National Pregnancy Registry for Antidepressants (NPRAD). Women 18 to 45 years of age or their health care providers may contact the registry by calling 844-405-6185. Enrollment should be done as early in pregnancy as possible.
Patient Education
What is this drug used for?
- It is used to treat low mood (depression).
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Dry mouth
- Fatigue
- Nausea
- Vomiting
- Diarrhea
- Change in taste
- Abdominal cramps
- Trouble sleeping
- Weight gain
- Weight loss
- Sweating a lot
- Flushing
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes
- Severe headache
- Dizziness
- Passing out
- Vision changes
- Eye pain
- Eye swelling or redness
- Confusion
- Sexual dysfunction
- Chest pain
- Seizures
- Chills
- Sore throat
- Bruising
- Bleeding
- Severe abdominal pain
- Severe loss of strength and energy
- Mouth irritation
- Mouth sores
- Tongue discoloration
- Severe constipation
- Noise or ringing in the ears
- Trouble urinating
- Change in amount of urine passed
- Hair loss
- Enlarged breasts
- Nipple discharge
- Change in sex drive
- Testicle swelling
- Nightmares
- Burning or numbness feeling
- Tremors
- Yellow skin or eyes
- Abnormal movements
- Sensing things that seem real but are not
- Fast heartbeat
- Abnormal heartbeat
- A significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.