Boxed Warning
Increased mortality in elderly patients with dementia-related psychosis:
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of 17 placebo-controlled trials (modal duration, 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients between 1.6 and 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was approximately 4.5%, compared with a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (eg, heart failure, sudden death) or infectious (eg, pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patient is not clear. Olanzapine is not approved for treatment of patients with dementia-related psychosis.
Postinjection delirium/sedation syndrome (Zyprexa Relprevv):
Adverse reactions with signs and symptoms consistent with olanzapine overdose, in particular, sedation (including coma) and/or delirium, have been reported following injections of olanzapine extended release (ER). Olanzapine ER must be administered in a registered health care facility with ready access to emergency response services. After each injection, patients must be observed at the health care facility by a health care provider for at least 3 hours. Because of this risk, olanzapine ER is available only through a restricted distribution program called Zyprexa Relprevv Patient Care Program, and requires health care provider, health care facility, patient, and pharmacy enrollment.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution Reconstituted, Intramuscular:
ZyPREXA: 10 mg (1 ea)
Generic: 10 mg (1 ea)
Suspension Reconstituted, Intramuscular:
ZyPREXA Relprevv: 210 mg (1 ea [DSC]); 300 mg (1 ea [DSC]); 405 mg (1 ea [DSC]) [contains polysorbate 80]
Suspension Reconstituted, Intramuscular [preservative free]:
ZyPREXA Relprevv: 210 mg (1 ea); 300 mg (1 ea); 405 mg (1 ea) [contains polysorbate 80]
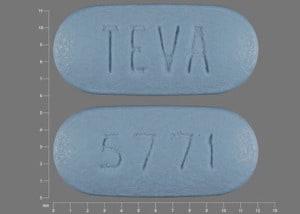
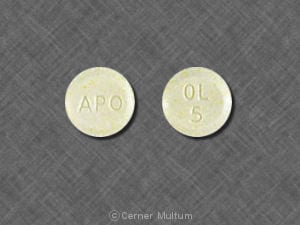
Tablet, Oral:
ZyPREXA: 2.5 mg, 5 mg, 7.5 mg, 10 mg
ZyPREXA: 15 mg [contains fd&c blue #2 aluminum lake]
ZyPREXA: 20 mg
Generic: 2.5 mg, 5 mg, 7.5 mg, 10 mg, 15 mg, 20 mg
Tablet Disintegrating, Oral:
ZyPREXA Zydis: 5 mg, 10 mg, 15 mg, 20 mg [contains aspartame, methylparaben sodium, propylparaben sodium]
Generic: 5 mg, 10 mg, 15 mg, 20 mg
Pharmacology
Mechanism of Action
Olanzapine is a second generation thienobenzodiazepine antipsychotic which displays potent antagonism of serotonin 5-HT2A and 5-HT2C, dopamine D1-4, histamine H1, and alpha1-adrenergic receptors. Olanzapine shows moderate antagonism of 5-HT3 and muscarinic M1-5 receptors, and weak binding to GABA-A, BZD, and beta-adrenergic receptors. Although the precise mechanism of action in schizophrenia and bipolar disorder is not known, the efficacy of olanzapine is thought to be mediated through combined antagonism of dopamine and serotonin type 2 receptor sites.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Well absorbed; not affected by food; tablets and orally disintegrating tablets are bioequivalent
Short-acting injection: Rapidly absorbed
Distribution
Vd: Extensive, 1000 L
Metabolism
Highly metabolized via direct glucuronidation and cytochrome P450 mediated oxidation (CYP1A2, CYP2D6); 40% removed via first pass metabolism
Excretion
Urine (57%, 7% as unchanged drug); feces (30%)
Clearance: Oral:
Children (10 to 18 years; n=8): Apparent: 9.6 ± 2.4 L/hour (Grothe 2000)
Adults: Apparent: 25 L/hour [12 to 47 L/hour (5th to 95th percentile)]; 40% increase in olanzapine clearance in smokers; 30% decrease in females
Onset of Action
Within 1 to 2 weeks for control of aggression, agitation, insomnia; 3 to 6 weeks for control of mania and positive psychotic symptoms. Adequate trial: Typically 6 weeks at maximum tolerated doses
Time to Peak
Maximum plasma concentrations after IM administration are 5 times higher than maximum plasma concentrations produced by an oral dose.
Extended-release injection: ~7 days
Short-acting injection: 15 to 45 minutes
Oral: Children (10 to 18 years; n=8): 4.7 ± 3.7 hours (Grothe 2000); Adults: ~6 hours
Half-Life Elimination
Oral and IM (short-acting): Children: (10 to 18 years; n=8): 37.2 ± 5.1 hours (Grothe 2000); Adults: 30 hours [21 to 54 hours (5th to 95th percentile)]; approximately 1.5 times greater in elderly
Extended-release injection: ~30 days
Protein Binding
Plasma: 93%, bound to albumin and alpha1-glycoprotein
Use in Specific Populations
Special Populations: Elderly
The half-life increases 1.5 times.
Special Populations: Gender
Clearance is approximately 30% lower in women.
Special Populations Note
Cigarette smoking: Clearance is approximately 40% higher in smokers.
Use: Labeled Indications
Agitation/Aggression (acute) associated with psychiatric disorders (short-acting IM): Treatment of acute agitation associated with schizophrenia and bipolar I mania.
Bipolar disorder (oral): Treatment of acute manic or mixed episodes of bipolar I disorder (as monotherapy or in combination with lithium or valproate) and maintenance treatment; treatment of bipolar depression in combination with fluoxetine.
Major depressive disorder (unipolar), treatment resistant (oral): Treatment of treatment-resistant depression in combination with fluoxetine.
Schizophrenia (oral, ER IM): Treatment of the manifestations of schizophrenia.
Use: Off Label
Agitation/Aggression and psychosis associated with dementiabyes
Data from randomized, double-blind, controlled trials support the use of olanzapine in the treatment of psychosis and agitation related to dementia De Deyn 2004, Meehan 2002, Schneider 2006, Street 2000, Sultzer 2008, Verhey 2006.
Based on the American Psychiatric Association (APA) practice guideline on the use of antipsychotics to treat agitation or psychosis in patients with dementia, antipsychotics such as olanzapine may be considered for the treatment of agitation and psychosis in certain patients with dementia; however, evidence for efficacy is modest and use should be limited to patients whose symptoms are dangerous, severe, or cause significant patient distress due to safety risks associated with antipsychotic use. Based on the World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of Alzheimer disease and other dementias, drug treatment with olanzapine for behavioral and psychological aspects (including hyperactivity and psychosis) is recommended at low doses and for short durations, as a last option after addressing causative factors and using psychosocial interventions.
Anorexia nervosacyes
Data from a limited number of clinical trials suggest that olanzapine may be beneficial in achieving more rapid weight gain in patients with anorexia nervosa; however, effects on weight gain were modest, with the largest trial reporting an average weight gain of 1.5 pounds per month with olanzapine Attia 2011, Attia 2019, Bissada 2008.
Based on the WFSBP guidelines for the pharmacological treatment of eating disorders and the APA guideline watch for the treatment of patients with eating disorders, olanzapine may be used in anorexia nervosa for weight gain APA [Yager 2012], WFSBP [Aigner 2011].
Bipolar disorder, hypomaniacyes
Data from a limited number of patients suggest that olanzapine may be beneficial in the treatment of hypomania Dennehy 2003.
Based on the WFSBP guidelines for the biological treatment of bipolar disorders update on the treatment of acute mania and the Canadian Network for Mood and Anxiety Treatments and International Society for Bipolar Disorders 2018 guidelines for the management of patients with bipolar disorder, limited evidence exists for the treatment of hypomania; however, based on clinical experience, treatment should be the same as mania, and clinicians may consider antipsychotics, such as olanzapine, and/or antimanic agents.
Chemotherapy-induced acute and delayed nausea or vomiting (high emetic risk [>90%]), preventiona
Data from a randomized, phase 3 study support the use of oral olanzapine (in combination with dexamethasone and palonosetron) for the prevention of acute and delayed chemotherapy-induced nausea and vomiting in chemotherapy-naive patients receiving highly emetogenic chemotherapy Navari 2011. Data from a multicenter, randomized, phase 3 study also support the use of oral olanzapine (in combination with triplet antiemetic therapy) for prevention of acute and delayed chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy Hashimoto 2020. Data from a randomized, phase 2 study that included chemotherapy-naive patients who received moderately and highly emetogenic chemotherapy regimens also suggest that oral olanzapine (in combination with dexamethasone and palonosetron) may be beneficial for prevention of acute and delayed nausea and vomiting Navari 2007.
Chemotherapy-induced breakthrough nausea or vomiting, treatmentayes
Data from a randomized, controlled, phase 3 study support the use of oral olanzapine in the management of breakthrough nausea and vomiting associated with highly emetogenic chemotherapy Navari 2013.
Based on antiemetic guidelines from the American Society of Clinical Oncology, oral olanzapine may be used for management of breakthrough nausea and vomiting.
Delirium, hyperactive (ICU treatment)cyes
Data from 1 small, prospective, randomized study evaluating oral haloperidol versus oral olanzapine in medical or surgical ICU patients with delirium suggest that both regimens are similar in safety and efficacy Skrobik 2004. However, data from a large, prospective, randomized trial evaluating IV haloperidol, IV ziprasidone, and placebo in medical or surgical ICU patients with delirium did not show a benefit with pharmacologic treatment on the duration of delirium and coma. There was no difference in survival, length of ICU stay, or length of hospital stay Girard 2018.
Based on the Society of Critical Care Medicine guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU (ie, the PADIS guidelines), nonpharmacologic management and treatment of underlying conditions should be implemented as the initial steps to reduce delirium. Antipsychotics (both typical and atypical) are not recommended for the prevention or treatment of delirium in the ICU except in patients who are experiencing distressing symptoms of delirium (eg, agitation, anxiety). In that case, short-term use of antipsychotics (typical or atypical) may be administered until the symptoms resolve SCCM [Devlin 2018].
Delirium, hyperactive (non-ICU treatment)cyes
Data from 1 small, single-blind, randomized study evaluating oral olanzapine, risperidone, and haloperidol in medical or surgical floor patients suggest that olanzapine is as effective as haloperidol in the treatment of delirium Grover 2011.
Based on the National Institute for Health and Clinical Excellence (NICE) and the National Clinical Guideline Centre (NCGC) guidelines for the diagnosis, prevention, and management of delirium, a short-term course of olanzapine (usually for 1 week or less) should be considered for the treatment of delirium in individuals who are distressed or considered a risk to themselves or others and verbal and nonverbal de-escalation techniques are ineffective or inappropriate. It is recommended to use antipsychotic drugs with caution or not at all for patients with conditions such as Parkinson disease or dementia with Lewy bodies.
Delusional infestation (delusional parasitosis)c
Data from a limited number of patients studied in case reports suggest that olanzapine may be beneficial for the treatment of delusional infestation (also called delusional parasitosis)
Huntington disease-associated choreac
Data from a limited number of patients studied in open-label trials suggest that olanzapine may be beneficial for the treatment of chorea associated with Huntington disease Bonelli 2002, Bonelli 2007, Paleacu 2002.
Major depressive disorder (unipolar) with psychotic featuresbyes
Data from 2 randomized, double-blind, controlled trials support the use of the combination of olanzapine with an antidepressant (sertraline or fluoxetine) in the treatment of patients with major depression with psychotic features Meyers 2009, Rothschild 2004.
Based on the APA practice guideline for the treatment of patients with major depressive disorder and the WFSBP guidelines for biological treatment of unipolar depressive disorders, in patients with psychotic depression, the combination of an antidepressant and antipsychotic is recommended at the onset of treatment.
Contraindications
There are no contraindications listed in the manufacturer’s labeling.
Canadian labeling: Hypersensitivity to olanzapine or any component of the formulation
Dosage and Administration
Dosing: Adult
Note: In patients who are medically ill, at risk for postural hypotension, or may metabolize more slowly (eg, nonsmoking, female, ≥65 years of age), a low starting dose (eg, 2.5 mg) and more gradual titration may be better tolerated. Due to the drug's sedating effect, bedtime dosing is preferred; alternatively, divided doses may improve tolerability (Jibson 2019).
Agitation/Aggression (severe, acute) associated with psychiatric disorders (eg, schizophrenia, bipolar disorder) (labeled use), substance intoxications (off-label use), or other organic causes (off-label use): Note: Antipsychotics are appropriate when psychosis is suspected to be the primary cause of agitation/aggression. Avoid in suspected or confirmed intoxications with anticholinergic substances; other agents are used preferentially in some intoxications (eg, stimulants) or alcohol withdrawal. Depending on presentation, may combine oral administration with a benzodiazepine; parenteral administration with a benzodiazepine is not recommended due to risk of respiratory depression (Klein 2018; Moore 2019; WFSBP [Hasan 2012]; Wilson 2012a; Wilson 2012b).
IM: Short-acting injection: Initial: 5 to 10 mg; may repeat based on response and tolerability 2 hours after initial dose and 4 hours after second dose; maximum: 30 mg/day (including oral olanzapine) (Wilson 2012b; manufacturer's labeling).
Oral (off-label route): Initial: 5 to 10 mg; may repeat based on response and tolerability every 2 hours up to 20 mg/day (Wilson 2012b).
IV: Short-acting injection (alternative agent) (off-label route): Note: IM administration is preferred in most clinical situations. If IV administration is used, limit to settings where patients can be closely monitored for respiratory depression (eg, emergency department) (Chan 2013; Cole 2017; Khorassani 2019; Martel 2016; Taylor 2017).
Initial: 5 to 10 mg single dose; if needed, may repeat once with an additional 2.5 to 5 mg dose ≥10 minutes after initial dose based on response and tolerability; total maximum dose: 10 mg (Cole 2017; Martel 2016; Taylor 2017).
Agitation/Aggression and psychosis associated with dementia, severe or refractory (alternative agent) (off-label use): Note: For short-term use while addressing underlying causes of severe symptoms (APA [Reus 2016]). In dementia with Lewy bodies, antipsychotics are generally avoided. If use is required, doses >2.5 mg/day are not recommended (Farlow 2019).
IM: Short-acting injection: Initial dose: 2.5 or 5 mg; may repeat based on response and tolerability with up to 2 additional 1.25 to 5 mg doses at intervals ≥2 hours after the initial dose and ≥1 hour after the second dose; maximum: 12.5 mg per episode (Meehan 2002).
Oral: Initial: 2.5 mg once daily, may increase dose based on response and tolerability in increments of 2.5 to 5 mg/day at intervals ≥1 week up to 10 mg/day (De Deyn 2004; Street 2000; Verhey 2006). In patients without a clinically significant response after an adequate trial (eg, up to 4 weeks), taper and withdraw therapy. Only continue in patients with demonstrated benefit; attempt to taper and withdraw at regular intervals (eg, within 4 months of initiation) (APA [Reus 2016]).
Anorexia nervosa (off-label use): Note: For acutely ill patients who do not gain weight with nutritional rehabilitation plus psychotherapy (Walsh 2019; WFSBP [Aigner 2011]).
Oral: Initial: 2.5 mg once daily; may increase dose based on response and tolerability in increments of 2.5 mg every 1 to 2 weeks up to 10 mg/day (Attia 2011; Attia 2019; Bissada 2008).
Bipolar disorder:
Acute manic or mixed episodes (labeled use) and acute hypomania (off-label use) (monotherapy or adjunctive therapy): Oral: Initial: 10 to 15 mg once daily; may increase dose based on response and tolerability in 5 mg increments at intervals of ≥1 day up to 20 mg/day (maximum per manufacturer's labeling); however, experts suggest some patients may require doses up to 50 mg/day for optimal response (CANMAT [Yatham 2018]; Citrome 2009; Stovall 2019).
Bipolar major depression, acute (alternative agent; monotherapy or adjunctive therapy) (off-label, except labeled use as adjunctive to fluoxetine): Oral: Initial: 5 mg once daily; may increase dose based on response and tolerability in 5 mg increments at intervals of every 1 to 7 days up to 15 mg/day (adjunctive therapy) or up to 20 mg/day (monotherapy) (Brown 2006; Shelton 2019; Tohen 2003, Tohen 2012; Wang 2014; WFSBP [Grunze 2010]). A fixed-dose olanzapine/fluoxetine combination may be used instead of separate components. See “Dosing Conversion” below.
Maintenance treatment (monotherapy [labeled use for manic or mixed episodes; off-label use for depression episodes] or adjunctive therapy [off-label use]): Note: Continue dose and combination regimen that was used to achieve control of the acute episode (CANMAT [Yatham 2018]).
Oral: Usual dose: 5 to 20 mg/day; maximum dose: 20 mg/day (manufacturer's labeling); however, for patients who required doses up to 50 mg/day to achieve remission, continue remission-achieving dose, as tolerated (Stovall 2019).
Chemotherapy-induced acute and delayed nausea or vomiting (high emetic risk [>90%]), prevention (off-label use): Oral: 5 or 10 mg on day of chemotherapy (day 1), followed by 5 or 10 mg once daily on days 2 to 4, in combination with antiemetics used for high emetic risk agents (Hashimoto 2020; Navari 2011; Navari 2016; Sutherland 2018). For cisplatin-based high emetic-risk therapy, the 5 mg dose (in combination with triplet antiemetic therapy) is effective and may be associated with less daytime sedation (Hashimoto 2020).
Chemotherapy-induced breakthrough nausea or vomiting, treatment (off-label use): Oral: 5 to 10 mg once daily for 3 days (Navari 2013; Sutherland 2018).
Delirium, hyperactive (treatment): Note: Nonpharmacologic interventions and treatment of underlying conditions are initial steps to prevent and manage delirium. Antipsychotics may be used as short-term adjunctive treatment if distressing symptoms (eg, agitation, anxiety, combative behavior) are present (SCCM [Devlin 2018]). Reassess daily for continued need; consider discontinuation and/or taper as symptoms resolve, especially at transitions of care to prevent unnecessary continuation of therapy (D’Angelo 2019; Marshall 2016; Tietze 2019).
ICU (off-label use):
Oral or via NG tube: Initial: 5 to 10 mg once daily (or 2.5 mg once daily in patients >60 years of age); titrate daily as needed in 2.5 to 5 mg increments up to 20 mg/day (Skrobik 2004; Tietze 2019).
IM: Short-acting injection: 5 to 10 mg once; may repeat if needed after 2 to 4 hours; maximum total dose including oral: 30 mg/day (Tietze 2019).
Non-ICU (off-label use):
Oral: Initial: 1.25 to 5 mg once daily or as needed; titrate daily based on symptoms in 2.5 to 5 mg increments up to 20 mg/day (Grover 2011; Roy-Byrne 2019).
IM: Short-acting injection: Initial: 2.5 to 5 mg once daily or as needed. Maximum dose (including oral): 20 mg/day (Grover 2011; Roy-Byrne 2019).
Delusional infestation (delusional parasitosis) (off-label use): Oral: Initial: 2.5 mg once daily; increase dose based on response and tolerability at intervals ≥1 week up to 7.5 mg/day (Campbell 2019; Suh 2019). Further increases up to 20 mg/day may be necessary in some patients for optimal response (Freudenmann 2008; Heller 2013). After achieving adequate response, maintain for ≥1 to 3 months before attempting to taper (Suh 2019).
Huntington disease-associated chorea, moderate to severe (alternative agent) (off-label use): Oral: Initial: 2.5 mg once daily; may increase dose based on response and tolerability in 2.5 to 5 mg increments at intervals ≥3 days up to 10 mg/day (Paleacu 2002; Suchowersky 2019). Further increases up to 30 mg/day may be necessary in some patients for optimal response (Bonelli 2002; Paleacu 2002).
Major depressive disorder (unipolar):
Psychotic depression (adjunctive therapy with an antidepressant) (off-label use): Oral: Initial: 5 mg once daily; may increase dose based on response and tolerability in increments of 5 mg at intervals of 3 to 7 days up to 20 mg/day (Meyers 2009; Rothschild 2004; WFSBP [Bauer 2013]). After 4 to 6 months of sustained recovery, some experts suggest discontinuing the antipsychotic and continuing antidepressant monotherapy (Rothschild 2003; Rothschild 2019; Wijkstra 2010).
Treatment-resistant depression (adjunctive therapy with an antidepressant) (off-label, except labeled use as adjunctive to fluoxetine): Oral: Initial: 5 mg once daily; may gradually increase dose based on response and tolerability up to 20 mg/day (CANMAT [Kennedy 2016]; Nelson 2019). A fixed-dose olanzapine/fluoxetine combination may be used instead of separate components. See “Dosing Conversion” below.
Schizophrenia (alternative agent) (PORT [Kreyenbuhl 2010]):
Oral: Initial: 5 mg once daily increasing to 10 mg once daily within several days or 10 mg once daily. Thereafter may increase dose based on response and tolerability in increments of 5 mg/day at intervals ≥1 week up to 20 mg/day; maximum dose: 20 mg/day (manufacturer's labeling). Further increases up to 30 mg/day may be necessary in some patients for optimal response (Stroup 2019). Note: Doses up to 50 mg/day have been evaluated in clinical studies; however, doses >30 mg/day are associated with increased adverse effects and generally not recommended (Citrome 2009).
IM: ER injection (olanzapine pamoate): Note: Establish tolerability using oral olanzapine prior to changing to ER injection. Overlap of oral olanzapine with initial dose of ER injection is not necessary. Due to the potential for a severe adverse reaction, patients must be observed for at least 3 hours after every injection. Maximum dose: 300 mg every 2 weeks or 405 mg every 4 weeks.
Conversion of oral olanzapine to ER IM olanzapine:
Oral olanzapine 10 mg daily: Initial dose: 210 mg every 2 weeks for 4 doses or 405 mg every 4 weeks for 2 doses; Maintenance dose: 150 mg every 2 weeks or 300 mg every 4 weeks.
Oral olanzapine 15 mg daily: Initial dose: 300 mg every 2 weeks for 4 doses; Maintenance dose: 210 mg every 2 weeks or 405 mg every 4 weeks.
Oral olanzapine 20 mg daily: Initial and maintenance dose: 300 mg every 2 weeks.
Dosage adjustment in elevated-risk patients: Initial: A lower starting dose of 150 mg every 4 weeks is recommended in patients who are debilitated, at risk for orthostatic hypotension, may metabolize olanzapine more slowly (eg, nonsmoking, female, patients ≥65 years of age), or who may be more sensitive to adverse effects; increase dose with caution as clinically indicated.
Dosing conversion:
Olanzapine/fluoxetine fixed-dose combination: When using individual components of olanzapine with fluoxetine rather than the fixed-dose combination product, corresponding approximate dosage equivalents are as follows:
Olanzapine 2.5 mg + fluoxetine 20 mg = combination strength 3/25
Olanzapine 5 mg + fluoxetine 20 mg = combination strength 6/25
Olanzapine 12.5 mg + fluoxetine 20 mg = combination strength 12/25
Olanzapine 5 mg + fluoxetine 50 mg = combination strength 6/50
Olanzapine 12.5 mg + fluoxetine 50 mg = combination strength 12/50
Discontinuation of therapy: Gradual dose reduction is advised to avoid withdrawal symptoms (ie, insomnia, headache, GI symptoms) unless discontinuation is due to significant adverse effects. In general, when discontinuing antipsychotic therapy for a chronic psychiatric disorder (eg, schizophrenia, bipolar disorder), decreasing the dose gradually over weeks to months (eg, reducing the dose by 10% per month) with close monitoring is suggested to allow for detection of prodromal symptoms of disease recurrence (APA [Lehman 2004]; CPA 2005).
Switching antipsychotics: An optimal universal strategy for switching antipsychotic drugs has not been established. Strategies include: Cross-titration (gradually discontinuing the first antipsychotic while gradually increasing the new antipsychotic) and abrupt change (abruptly discontinuing the first antipsychotic and either increasing the new antipsychotic gradually or starting it at a treatment dose). In patients with schizophrenia at high risk of relapse, the current medication may be maintained at full dose as the new medication is increased (ie, overlap); once the new medication is at therapeutic dose, the first medication is gradually decreased and discontinued over 1 to 2 weeks (Cerovecki 2013; Remington 2005; Takeuchi 2017). Based upon clinical experience, some experts generally prefer cross-titration and overlap approaches rather than abrupt change (Post 2019; Stroup 2019).
Dosing: Geriatric
Refer to adult dosing.
Short-acting IM, Oral: Consider lower starting dose of 2.5 to 5 mg daily for elderly patients; may increase as clinically indicated and tolerated with close monitoring of orthostatic blood pressure.
ER IM: Consider lower starting dose of 150 mg every 4 weeks for elderly patients; increase dose with caution as clinically indicated.
Dosing: Pediatric
Bipolar I disorder (acute manic or mixed episodes): Oral:
Children 4 to <6 years: Limited data available: Initial: 1.25 mg once daily; increase at weekly intervals according to response and tolerability to target dose: 10 mg/day. Dosing based on an open-label trial in 15 children (mean age: 5 ± 0.8 years; mean weight: 20.8 kg; mean required dose: 6.3 ± 2.3 mg/day) that showed significant improvement in manic symptoms (Biederman, 2005)
Children 6-12 years: Limited data available: Initial: 2.5 mg once daily; increase dose in 2.5 or 5 mg increments at weekly intervals to target dose of 10 mg once daily; maximum dose: 20 mg/day (Frazier, 2001; Kowatch, 2006; Wozniak, 2009)
Adolescents: Initial: 2.5-5 mg once daily; increase dose in 2.5 or 5 mg increments at weekly intervals to target dose of 10 mg once daily; maximum dose: 20 mg/day. In adolescent flexible-dosing (2.5-20 mg/day) clinical trials, the mean modal dose was 10.7 mg/day (mean dose: 8.9 mg/day) (Kowatch, 2006; Tohen, 2007)
Schizophrenia: Children ≥8 years (Limited data available) and Adolescents: Oral: Initial: 2.5-5 mg once daily; increase dose in 2.5 or 5 mg increments at weekly intervals to target dose of 10 mg once daily; maximum dose: 20 mg/day. Note: Doses up to 30 mg/day were used in one study of adolescents who were treatment refractory; however, some patients did not tolerate doses > 20 mg/day (Kumra, 2008); safety and efficacy of doses >20 mg/day have not been fully evaluated. In adolescent flexible-dosing (2.5-20 mg/day) clinical trials, the mean modal dose was 12.5 mg/day (mean dose: 11.1 mg/day). Dosing in children is based on two double-blind comparison studies which included both children and adolescents [n=35, age: 8-19 years with seven children; n=13, age: 7-16 years (mean age: 12.8 + 2.4 years)] (Shaw, 2006; Sikich, 2008).
Anorexia nervosa: Children ≥9 years and Adolescents: Limited data available: Oral: 1.25-2.5 mg once daily has been shown in one small trial and several case reports to improve BMI and other disease-related symptoms (eg, eating attitudes, anxiety); another case series used initial doses of 2.5 mg once daily and final doses of 5 mg to 10 mg once daily; reported range: 1.25-12.5 mg/day; however, it has been suggested that higher doses (>2.5 mg once daily) may not be associated with greater efficacy (Boachie, 2003; Dunican, 2007; Legerro, 2010; Mehler, 2001; Mehler-Wex, 2007).
Tourette syndrome, tic disorder: Children ≥7 years and Adolescents: Limited data available: Oral:
Patient weight ≤40 kg: Initial: 2.5 mg every other day for 3 days, increase to 2.5 mg every day for remainder of week; increase to 5 mg/day by second week if needed; then increase in 5 mg increments at weekly intervals as tolerated; maximum dose: 20 mg/day
Patient weight >40 kg: Initial: 2.5 mg every day for 3 days; increase to 5 mg every day for remainder of week if needed, then increase in 5 mg increments at weekly intervals as tolerated; maximum dose: 20 mg/day
An open-label study of 10 pediatric patients (7-13 years of age) reported significant reductions in tic severity [Yale Global Tic Severity Scale (YGTSS)] from baseline at a mean final dose of 14.5 mg/day after 8 weeks of treatment (Stephens, 2004). An open-label trial of 12 children and adolescents (7-14 years of age) reported a significant reduction (30%) in total tic severity (YGTSS) at a final mean dose of 11.3 mg/day (range: 2.5-20 mg/day) (McCracken, 2008)
Agitation (acute, associated with bipolar disorder or schizophrenia): Limited data available: IM (short-acting): Children: 5 mg; Adolescents: 10 mg. Dosing based on a retrospective report of IM olanzapine use in an inpatient psychiatric setting which included 50 pediatric patients [children (n=15; mean age: 11 years); adolescents (n=35; mean age: 15 years)] and evaluated 163 doses administered; results showed a 90.2% response rate (Khan, 2006)
Reconstitution
Injection, extended-release: Dilute as directed to final concentration of 150 mg/mL. Shake vigorously to mix; will form yellow, opaque suspension. Following reconstitution, suspension may be stored at room temperature and used within 24 hours. Shake vigorously to resuspend prior to administration. If foam forms, let vial stand to allow foam to dissipate. Use immediately once suspension is in syringe. Suspension may be irritating to skin; wear gloves during reconstitution.
Injection, short-acting: Reconstitute 10 mg vial with 2.1 mL SWFI. Resulting solution is ~5 mg/mL. Use immediately (within 1 hour) following reconstitution. Discard any unused portion. Do not mix diazepam, lorazepam, or haloperidol in the same syringe.
Administration
Short-acting injection: May be administered IM or IV (off-label route); do not administer injection subcutaneously. For IM administration, inject slowly, deep into muscle. For off-label IV route, administer by rapid IV push (Taylor 2017). If dizziness and/or drowsiness are noted, patient should remain recumbent until examination indicates postural hypotension and/or bradycardia are not a problem.
Extended-release injection: For IM gluteal injection only; do not administer IV or subcutaneously. After needle insertion into muscle, aspirate to verify that no blood appears. Do not massage injection site. Use diluent, syringes, and needles provided in convenience kit; obtain a new kit if aspiration of blood occurs.
Tablet: May be administered without regard to meals.
Orally-disintegrating: Remove from foil blister by peeling back (do not push tablet through the foil); place tablet in mouth immediately upon removal; tablet dissolves rapidly in saliva and may be swallowed with or without liquid. May be administered with or without food/meals.
Dietary Considerations
Tablets may be taken without regard to meals. Some products may contain phenylalanine.
Storage
Injection, extended-release: Store at controlled room temperature, not to exceed 30°C (86°F).
Injection, short-acting: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F); do not freeze. Protect from light.
Tablet and orally disintegrating tablet: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light and moisture.
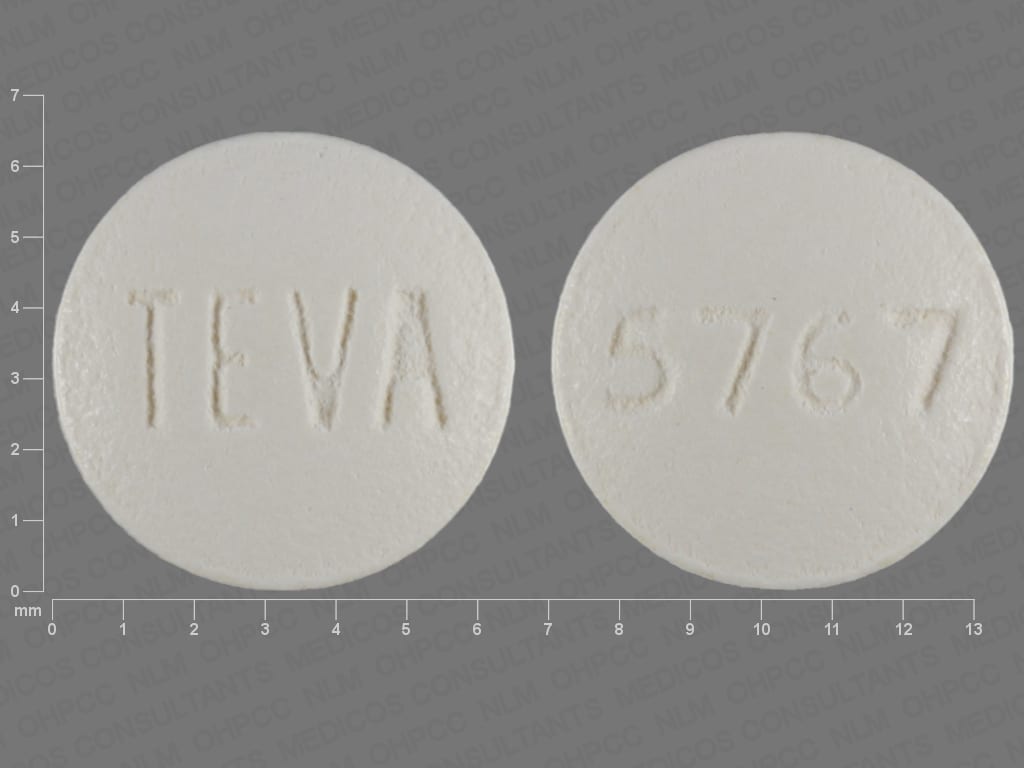
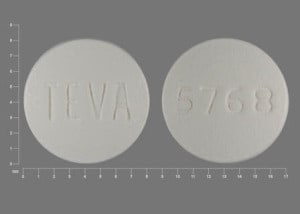
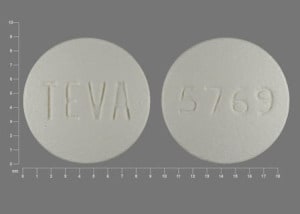
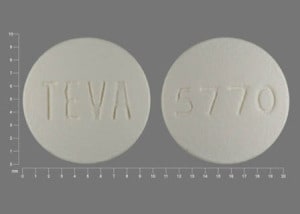
OLANZapine Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Acetylcholinesterase Inhibitors (Central): May enhance the neurotoxic (central) effect of Antipsychotic Agents. Severe extrapyramidal symptoms have occurred in some patients. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Amisulpride: Antipsychotic Agents may enhance the adverse/toxic effect of Amisulpride. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Amisulpride: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Avoid combination
Amphetamines: Antipsychotic Agents may diminish the stimulatory effect of Amphetamines. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Antihepaciviral Combination Products: May decrease the serum concentration of OLANZapine. Monitor therapy
Anti-Parkinson Agents (Dopamine Agonist): Antipsychotic Agents (Second Generation [Atypical]) may diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Management: Consider using an alternative antipsychotic agent when possible in patients with Parkinson disease. If an atypical antipsychotic is necessary, consider using clozapine or quetiapine, which may convey the lowest interaction risk. Consider therapy modification
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Benzodiazepines: OLANZapine may enhance the adverse/toxic effect of Benzodiazepines. Management: Avoid concomitant use of parenteral benzodiazepines and IM olanzapine due to risks of additive adverse events (e.g., cardiorespiratory depression). Olanzapine prescribing information provides no specific recommendations regarding oral administration. Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Broccoli: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Bromopride: May enhance the adverse/toxic effect of Antipsychotic Agents. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
BuPROPion: May enhance the neuroexcitatory and/or seizure-potentiating effect of Agents With Seizure Threshold Lowering Potential. Monitor therapy
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: May decrease the serum concentration of OLANZapine. Monitor therapy
Ceritinib: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Clarithromycin: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Clarithromycin. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
CloZAPine: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of CloZAPine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
CYP1A2 Inducers (Moderate): May decrease the serum concentration of OLANZapine. Monitor therapy
CYP1A2 Inducers (Weak): May decrease the serum concentration of OLANZapine. Exceptions: CarBAMazepine; Ombitasvir, Paritaprevir, and Ritonavir; Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir; RifAMPin; Ritonavir; Tobacco (Smoked). Monitor therapy
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of OLANZapine. Monitor therapy
CYP1A2 Inhibitors (Strong): May increase the serum concentration of OLANZapine. Monitor therapy
Deutetrabenazine: May enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, the risk for akathisia, parkinsonism, or neuroleptic malignant syndrome may be increased. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Domperidone: QT-prolonging Agents (Moderate Risk) may enhance the QTc-prolonging effect of Domperidone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Droperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Flupentixol: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Flupentixol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Guanethidine: Antipsychotic Agents may diminish the therapeutic effect of Guanethidine. Monitor therapy
Haloperidol: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
LamoTRIgine: May enhance the sedative effect of OLANZapine. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Lithium: May enhance the neurotoxic effect of Antipsychotic Agents. Lithium may decrease the serum concentration of Antipsychotic Agents. Specifically noted with chlorpromazine. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mequitazine: Antipsychotic Agents may enhance the arrhythmogenic effect of Mequitazine. Management: Consider alternatives to one of these agents when possible. While this combination is not specifically contraindicated, mequitazine labeling describes this combination as discouraged. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylphenidate: Antipsychotic Agents may enhance the adverse/toxic effect of Methylphenidate. Methylphenidate may enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Metoclopramide: May enhance the adverse/toxic effect of Antipsychotic Agents. Avoid combination
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
MetyroSINE: May enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Ondansetron: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pentamidine (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Piribedil: Antipsychotic Agents may diminish the therapeutic effect of Piribedil. Piribedil may diminish the therapeutic effect of Antipsychotic Agents. Management: Use of piribedil with antiemetic neuroleptics is contraindicated, and use with antipsychotic neuroleptics, except for clozapine, is not recommended. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
QT-prolonging Agents (Highest Risk): May enhance the QTc-prolonging effect of OLANZapine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
QT-prolonging Antidepressants (Moderate Risk): QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Antipsychotics (Moderate Risk): May enhance the QTc-prolonging effect of OLANZapine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Amisulpride; CloZAPine; Droperidol; Flupentixol; OLANZapine; Pimozide. Monitor therapy
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Kinase Inhibitors (Moderate Risk): QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Miscellaneous Agents (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Quinagolide: Antipsychotic Agents may diminish the therapeutic effect of Quinagolide. Monitor therapy
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
RifAMPin: May decrease the serum concentration of OLANZapine. Monitor therapy
Ritonavir: May decrease the serum concentration of OLANZapine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Saquinavir: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Saquinavir. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Serotonergic Agents (High Risk): May enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, serotonergic agents may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotic Agents may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Sulpiride: Antipsychotic Agents may enhance the adverse/toxic effect of Sulpiride. Avoid combination
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrabenazine: May enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Tobacco (Smoked): May diminish the therapeutic effect of OLANZapine. Tobacco (Smoked) may decrease the serum concentration of OLANZapine. Monitor therapy
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Valproate Products: May decrease the serum concentration of OLANZapine. Monitor therapy
Voriconazole: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
Oral:
>10%:
Cardiovascular: Orthostatic hypotension (3% to ≥20%)
Central nervous system: Drowsiness (dose dependent; adolescents and adults: 20% to 39%), extrapyramidal reaction (dose dependent; adults: ≤32%; adolescents: ≤10%), akathisia (adolescents and adults: 3% to 27%), parkinsonian-like syndrome (14% to 20%; includes akinesia, cogwheel rigidity, extrapyramidal syndrome, hypertonia, hypokinesia, masked facies, and tremor), dizziness (adults: 11% to 18%; adolescents: 7% to 8%), headache (adolescents: 17%), fatigue (dose dependent; adolescents and adults: 2% to 14%), insomnia (12%)
Endocrine & metabolic: Increased serum prolactin (adolescents: 47%; adults: 30%), weight gain (adults: 5% to 6%; has been reported as high as 40%; adolescents: 29% to 31%)
Gastrointestinal: Increased appetite (adolescents: 17% to 29%; adults: 3% to 6%), xerostomia (dose dependent; adults: 3% to 22%; adolescents: 4% to 7%), dyspepsia (adults: 7% to 11%; adolescents: 3%), constipation (adolescents and adults: 4% to 11%)
Hepatic: Increased serum AST (adolescents: 28%), decreased serum bilirubin (adolescents: 22%), increased serum ALT (≥3 x ULN; adolescents and adults: 5% to 12%)
Neuromuscular & skeletal: Weakness (dose dependent; 8% to 20%)
Miscellaneous: Accidental injury (12%)
1% to 10%:
Cardiovascular: Chest pain (3%), peripheral edema (3%), tachycardia (3%), hypertension (2%)
Central nervous system: Personality disorder (5% to 8%), abnormal gait (6%), hypertonia (3%), restlessness (adolescents: 3%), falling (older adults: ≥2%), articulation impairment (2%)
Endocrine & metabolic: Increased gamma-glutamyl transferase (adolescents: 10%; adults: 2%), increased uric acid (4%), menstrual disease (2%; including amenorrhea, hypomenorrhea, delayed menstruation, oligomenorrhea), breast changes (male and female adolescents: ≤2%; including discharge, enlargement, galactorrhea, gynecomastia, lactation disorder)
Gastrointestinal: Abdominal pain (adolescents: 6%), vomiting (≤4%), diarrhea (adolescents: 3%)
Genitourinary: Urinary incontinence (adults and older adults: ≥2%), sexual disorder (2%; adolescents: ≤1%; anorgasmia, delayed ejaculation, erectile dysfunction, changes in libido, abnormal orgasm, sexual dysfunction), urinary tract infection (2%)
Hematologic & oncologic: Bruise (5%)
Hepatic: Increased liver enzymes (adolescents: ≤8%), increased serum alkaline phosphatase (≥1%)
Neuromuscular & skeletal: Tremor (4% to 7%; dose dependent), limb pain (adolescents and adults: 5% to 6%), arthralgia (adults: 5%; adolescents: 2%), back pain (5%), muscle rigidity (adolescents: 2%), dyskinesia (1%)
Ophthalmic: Amblyopia (3%)
Respiratory: Rhinitis (7%), cough (6%), nasopharyngitis (adolescents: 4%), pharyngitis (4%), epistaxis (adolescents: 3%), respiratory tract infection (adolescents: 3%), sinusitis (adolescents: 3%)
Miscellaneous: Fever (≤6%)
Injection: Frequency not always defined. Unless otherwise noted, adverse events are reported for placebo-controlled trials in adult patients on extended release IM injection (Zyprexa Relprevv). Also refer to adverse reactions noted with oral therapy.
Cardiovascular: Hypertension (2% to 3%), hypotension (short-acting solution for IM injection: 2%), prolonged Q-T interval on ECG (2%), orthostatic hypotension (short-acting solution for IM injection: 1%)
Central nervous system: Headache (13% to 18%), sedation (8% to 13%), drowsiness (both IM injection formulations: 5% to 6%), akathisia (short-acting solution for IM injection: 5%), dizziness (both IM injection formulations: 4%), fatigue (3% to 4%), extrapyramidal reaction (solution for IM injection: 2% to 4%), abnormality in thinking (3%), auditory hallucination (3%), parkinsonian-like syndrome (short-acting solution for IM injection: 3%), restlessness (3%), pain (2% to 3%), abnormal dreams (2%), procedural pain (2%), sleep disorder (2%), dysarthria (1% to 2%)
Dermatologic: Acne vulgaris (2%)
Endocrine & metabolic: Weight gain (6% to 7%)
Gastrointestinal: Diarrhea (5% to 7%), vomiting (6%), xerostomia (2% to 6%), increased appetite (1% to 6%), nausea (long-acting IM formula: 4% to 5%; short-acting solution for injection: <1%), tooth infection (4%), toothache (3% to 4%), abdominal pain (3%), flatulence (1% to 2%)
Genitourinary: Vaginal discharge (4%)
Hepatic: Increased liver enzymes (3% to 4%)
Infection: Viral infection (2%)
Local: Pain at injection site (both IM injection formulations: 1% to 4%), abscess at injection site
Neuromuscular & skeletal: Arthralgia (3%), back pain (5%), muscle spasm (1% to 3%), stiffness (4%), tremor (long-acting IM formula: 3%; short-acting solution for injection: 1%)
Otic: Otalgia (4%)
Respiratory: Cough (9%), nasal congestion (7%), nasopharyngitis (3% to 6%), upper respiratory tract infection (3% to 4%), pharyngolaryngeal pain (3%), sneezing (2%)
Miscellaneous: Fever (2%)
<1%, postmarketing, and/or case reports: Abdominal distension, accommodation disturbance, agranulocytosis, alopecia, anaphylactoid reaction, angioedema, ataxia, cerebrovascular accident, chills, coma, confusion, delirium, diabetes mellitus, diabetic ketoacidosis, diabetic coma, difficulty in micturition, DRESS syndrome, dry eye syndrome, dysarthria, facial edema, hangover effect, hepatic injury (cholestatic or mixed), hepatitis, hyperbilirubinemia, hypercholesterolemia, hyperglycemia, hyperlipidemia, hypermenorrhea, hypertriglyceridemia, hypoproteinemia, impotence, increased creatine phosphokinase, intestinal obstruction, jaundice, ketosis, leukocytosis (eosinophilia), leukopenia, liver steatosis, mastalgia, mydriasis, myopathy, nausea, neuroleptic malignant syndrome, neutropenia, osteoporosis, pancreatitis, polyuria, postinjection delirium/sedation syndrome, priapism, pruritus, pulmonary edema, pulmonary embolism, respiratory depression (Cole 2007), restless legs syndrome, rhabdomyolysis, seizure, skin photosensitivity, skin rash, sleep apnea syndrome (obstructive) (Health Canada 2016; Shirani 2011), speech disturbance, stupor, suicidal tendencies, syncope, tardive dyskinesia, thrombocytopenia, tongue edema, transient ischemic attacks, urinary frequency, urinary retention, urinary urgency, urticaria, vasodilation, venous thrombosis, withdrawal syndrome
Warnings/Precautions
Concerns related to adverse effects:
- Altered cardiac conduction: May alter cardiac conduction and prolong the QT interval; life-threatening arrhythmias have occurred with therapeutic doses of antipsychotics (Haddad 2002; Ray 2009). Risk may be increased by conditions or concomitant medications which cause bradycardia, hypokalemia, and/or hypomagnesemia. Use caution in patients with a history of conduction abnormalities.
- Anticholinergic effects: May cause anticholinergic effects (constipation, xerostomia, blurred vision, urinary retention); use with caution in patients with decreased gastrointestinal motility, paralytic ileus, urinary retention, BPH, xerostomia, or visual problems (including narrow-angle glaucoma). Relative to other neuroleptics, olanzapine has a moderate potency of cholinergic blockade (Richelson 1999).
- Blood dyscrasias: Leukopenia, neutropenia, and agranulocytosis (sometimes fatal) have been reported in clinical trials and postmarketing reports with antipsychotic use; presence of risk factors (eg, preexisting low WBC or history of drug-induced leuko-/neutropenia) should prompt periodic blood count assessment. Discontinue therapy at first signs of blood dyscrasias or if absolute neutrophil count <1,000/mm3.
- Cerebrovascular effects: An increased incidence of cerebrovascular effects (eg, transient ischemic attack, stroke), including fatalities, has been reported in placebo-controlled trials of olanzapine for the unapproved use in elderly patients with dementia-related psychosis.
- CNS depression: May cause CNS depression, which impair physical and mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving). May be moderate to highly sedating in comparison with other antipsychotics (APA [Lehman 2004]); dose-related effects have been observed.
- Dyslipidemia: Dose-related increases in cholesterol and triglycerides have been noted. Use with caution in patients with preexisting abnormal lipid profile. Compared with other antipsychotics, the risk of dyslipidemia is high (Solmi 2017).
- Esophageal dysmotility/aspiration: Antipsychotic use has been associated with esophageal dysmotility and aspiration; risks increase with age. Use with caution in patients at risk of aspiration pneumonia (ie, Alzheimer disease), particularly in patients >75 years (Herzig 2017; Maddalena 2004).
- Extrapyramidal symptoms: May cause extrapyramidal symptoms (EPS), including pseudoparkinsonism, acute dystonic reactions, akathisia, and tardive dyskinesia (risk of these reactions is generally much lower relative to typical/conventional antipsychotics; frequencies reported are similar to placebo). Risk of dystonia (and probably other EPS) may be greater with increased doses, use of conventional antipsychotics, males, and younger patients. Factors associated with greater vulnerability to tardive dyskinesia include older in age, female gender combined with postmenopausal status, Parkinson disease, pseudoparkinsonism symptoms, affective disorders (particularly major depressive disorder), concurrent medical diseases such as diabetes, previous brain damage, alcoholism, poor treatment response, and use of high doses of antipsychotics (APA [Lehman 2004]; Soares-Weiser 2007). Consider therapy discontinuation with signs/symptoms of tardive dyskinesia.
- Falls: May increase the risk for falls due to somnolence, orthostatic hypotension, and motor or sensory instability. Complete fall risk assessments at baseline and periodically during treatment in patients with diseases or on medications that may also increase fall risk.
- Hyperglycemia: Atypical antipsychotics have been associated with development of hyperglycemia; in some cases, may be extreme and associated with ketoacidosis, hyperosmolar coma, or death. Olanzapine may have a greater association with hyperglycemia than other atypical antipsychotics. Use with caution in patients with diabetes or other disorders of glucose regulation; monitor for worsening of glucose control. Patients with risk factors for diabetes (eg, obesity or family history) should have a baseline fasting blood sugar (FBS) and periodic assessment of glucose regulation. Compared with other antipsychotics, the risk of hyperglycemia is high (Solmi 2017).
- Hyperprolactinemia: May cause dose-related increases in prolactin levels; clinical significance of hyperprolactinemia in patients with breast cancer or other prolactin-dependent tumors is unknown. Clinical manifestations of increased prolactin levels included menstrual-, sexual- and breast-related events.
- Multiorgan hypersensitivity reactions (drug reaction with eosinophilia and systemic symptoms [DRESS]): Potentially serious, sometimes fatal, multiorgan hypersensitivity reactions (DRESS) have been reported. Symptoms may include a cutaneous reaction (rash or exfoliative dermatitis), eosinophilia, fever, and/or lymphadenopathy with systemic complications (eg, hepatitis, nephritis, pneumonitis, myocarditis, pericarditis). Discontinue olanzapine if DRESS is suspected.
- Neuroleptic malignant syndrome (NMS): Use may be associated with NMS; monitor for mental status changes, fever, muscle rigidity, and/or autonomic instability.
- Orthostatic hypotension: May cause orthostatic hypotension; use with caution in patients at risk of this effect or in those who would not tolerate transient hypotensive episodes (cerebrovascular disease, cardiovascular disease, hypovolemia, or concurrent medication use that may predispose to hypotension/bradycardia).
- Suicidal ideation: The possibility of a suicide attempt is inherent in psychotic illness or bipolar disorder; use with caution in high-risk patients during initiation of therapy. Prescriptions should be written for the smallest quantity consistent with good patient care.
- Temperature regulation: Impaired core body temperature regulation may occur; caution with strenuous exercise, heat exposure, dehydration, and concomitant medication possessing anticholinergic effects.
- Weight gain: Significant weight gain (>7% of baseline weight) has been observed with antipsychotic therapy; incidence varies with product. Dose-related changes have been observed with olanzapine. Monitor waist circumference and BMI. Compared with other antipsychotics, the risk of weight gain is high (Solmi 2017).
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with severe cardiac disease, hemodynamic instability, prior myocardial infarction, ischemic heart disease, or hypercholesterolemia.
- Dementia: [US Boxed Warning]: Elderly patients with dementia-related psychosis treated with antipsychotics are at an increased risk of death compared with placebo. Most deaths appeared to be either cardiovascular (eg, heart failure, sudden death) or infectious (eg, pneumonia) in nature. Use with caution in patients with Lewy body dementia or Parkinson disease dementia due to greater risk of adverse effects, increased sensitivity to extrapyramidal effects, and association with irreversible cognitive decompensation or death. (APA [Reus 2016]). Olanzapine is not approved for the treatment of dementia-related psychosis.
- Hepatic impairment: Use with caution in patients with hepatic disease or impairment; may increase transaminases (primarily ALT).
- Parkinson disease: Use with caution in patients with Parkinson disease; antipsychotic may aggravate motor disturbances (APA [Lehman 2004]; APA [Reus 2016]).
- Renal impairment: Use with caution in patients with renal disease.
- Seizures: Use with caution in patients at risk of seizures, including those with a history of seizures, head trauma, brain damage, alcoholism, or concurrent therapy with medications that may lower seizure threshold. Elderly patients may be at increased risk of seizures because of an increased prevalence of predisposing factors.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Adolescents: Use in patients ≥13 years of age may result in increased weight gain and sedation, as well as greater increases in LDL cholesterol, total cholesterol, triglycerides, prolactin, and liver transaminase levels when compared with adults. Adolescent patients should be maintained on the lowest dose necessary.
- Smokers: Olanzapine levels may be lower in patients who smoke. Smokers may require a daily dose 30% higher than nonsmokers in order to obtain an equivalent olanzapine concentration (Tsuda 2014); however, the manufacturer does not routinely recommend dosage adjustments.
Dosage form-specific concerns:
- Intramuscular formulations: There are two Zyprexa formulations for intramuscular injection: Zyprexa Relprevv is an extended-release formulation and Zyprexa IntraMuscular is short-acting.
Extended-release IM injection (Zyprexa Relprevv):
Postinjection delirium/sedation syndrome: [US Boxed Warning]: Sedation (including coma) and delirium (including agitation, anxiety, confusion, disorientation) have been observed following use of Zyprexa Relprevv; events associated with an inadvertent rapid rise in serum concentrations; administer at a registered health care facility where patients should be continuously monitored (≥3 hours) for symptoms of olanzapine overdose; symptom development highest in first hour but may occur within or after 3 hours; risk of syndrome is cumulative with each injection; recovery expected by 72 hours. Upon determining alert status, patient should be escorted to their destination and not drive or operate heavy machinery for the remainder of the day.
Unexplained deaths: Two unexplained deaths in patients who received Zyprexa Relprevv have been reported. The patients died 3 to 4 days after receiving an appropriate dose of the drug. Both patients were found to have high blood concentrations of olanzapine postmortem. It is unclear if these deaths were the result of postinjection delirium sedation syndrome (PDSS) (FDA Safety Communication 2013).
Restricted distribution program: Zyprexa Relprevv is only available under a restricted distribution program. Only prescribers, health care facilities, and pharmacies registered with the program are able to prescribe, distribute, or dispense Zyprexa Relprevv for patients who are enrolled in and meet all conditions of the program.
Short-acting IM injection (Zyprexa IntraMuscular): Patients should remain recumbent if drowsy/dizzy until hypotension, bradycardia, and/or hypoventilation have been ruled out. Closely monitor for orthostasis prior to any repeat dosing. Concurrent use of IM/IV benzodiazepines is not recommended (fatalities have been reported, though causality not determined).
- Phenylalanine: Some products may contain phenylalanine.
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer’s labeling.
Other warnings/precautions:
- Discontinuation of therapy: When discontinuing antipsychotic therapy, the American Psychiatric Association (APA), Canadian Psychiatric Association (CPA), and World Federation of Societies of Biological Psychiatry (WFSBP) guidelines recommend gradually tapering antipsychotics to avoid physical withdrawal symptoms, including anorexia, anxiety, diaphoresis, diarrhea, dizziness, dyskinesia, headache, myalgia, nausea, paresthesia, restlessness, tremulousness, and vomiting (APA [Lehman 2004]; CPA 2005; Lambert 2007; WFSBP [Hasan 2012]). The risk of withdrawal symptoms is highest following abrupt discontinuation of highly anti-cholinergic or dopaminergic antipsychotics (Cerovecki 2013). Additional factors such as duration of antipsychotic exposure, the indication for use, medication half-life, and risk for relapse should be considered. In schizophrenia, there is no reliable indicator to differentiate the minority who will not from the majority who will relapse with drug discontinuation. However, studies in which the medication of well-stabilized patients were discontinued indicate that 75% of patients relapse within 6 to 24 months. Indefinite maintenance antipsychotic medication is generally recommended, and especially for patients who have had multiple prior episodes or 2 episodes within 5 years (APA [Lehman 2004]).
- IV administration: IV administration has only been studied in emergency department settings, where patients can be closely monitored for respiratory depression (ie, pulse oximetry) (Chan 2013; Cole 2017; Martel 2016; Taylor 2017).
Monitoring Parameters
Mental status; vital signs (as clinically indicated); blood pressure (baseline; repeat 3 months after antipsychotic initiation, then yearly); weight, height, BMI, waist circumference (baseline; repeat at 4, 8, and 12 weeks after initiating or changing therapy, then quarterly; consider switching to a different antipsychotic for a weight gain ≥5% of initial weight); CBC (as clinically indicated; monitor frequently during the first few months of therapy in patients with pre-existing low WBC or history of drug-induced leukopenia/neutropenia); electrolytes and liver function (annually and as clinically indicated); personal and family history of obesity, diabetes, dyslipidemia, hypertension, or cardiovascular disease (baseline; repeat annually); fasting plasma glucose level/HbA1c (baseline; repeat 3 months after starting antipsychotic, then yearly); fasting lipid panel (baseline; repeat 3 months after initiation of antipsychotic; if LDL level is normal repeat at 2-5 year intervals or more frequently if clinical indicated); changes in menstruation, libido, development of galactorrhea, erectile and ejaculatory function (at each visit for the first 12 weeks after the antipsychotic is initiated or until the dose is stable, then yearly); abnormal involuntary movements or parkinsonian signs (baseline; repeat weekly until dose stabilized for at least 2 weeks after introduction and for 2 weeks after any significant dose increase); tardive dyskinesia (every 12 months; high-risk patients every 6 months); ocular examination (yearly in patients >40 years; every 2 years in younger patients) (ADA 2004; APA [Lehman 2004]; Marder 2004)
Additional monitoring parameters with administration of injection formulations:
IM, short-acting and IV: Sedation; vital signs (blood pressure, pulse, respiratory rate); EKG (in patients at risk for QT prolongation) (Cole 2017; Taylor 2017).
IM, extended release: Sedation/delirium for 3 hours after each dose.
Pregnancy
Pregnancy Considerations
Olanzapine crosses the placenta and can be detected in cord blood at birth (Newport 2007; Schoretsanitis 2019).
Based on available data, an increased risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes has not been observed following maternal use of olanzapine (Brunner 2013; Damkier 2018; Huybrechts 2016). Antipsychotic use during the third trimester of pregnancy has a risk for abnormal muscle movements (extrapyramidal symptoms) and/or withdrawal symptoms in newborns following delivery. Symptoms in the newborn may include agitation, feeding disorder, hypertonia, hypotonia, respiratory distress, somnolence, and tremor; these effects may be self-limiting or require hospitalization.
The pharmacokinetic properties of olanzapine are not significantly altered by pregnancy (Westin 2018); however, serum levels may change, even at a stable dose, possibly due to decreased CYP1A2 activity during the second and third trimesters (Stiegler 2014; Westin 2018). The ACOG recommends that therapy during pregnancy be individualized; treatment with psychiatric medications during pregnancy should incorporate the clinical expertise of the mental health clinician, obstetrician, primary health care provider, and pediatrician. Safety data related to atypical antipsychotics during pregnancy are limited, as such, routine use is not recommended. However, if a woman is inadvertently exposed to an atypical antipsychotic while pregnant, continuing therapy may be preferable to switching to an agent that the fetus has not yet been exposed to; consider risk:benefit (ACOG 2008). If treatment is needed in a woman planning a pregnancy or if treatment is initiated during pregnancy, olanzapine may be used (Larsen 2015). The potential for excessive maternal weight gain and the development of gestational diabetes associated with olanzapine therapy should be considered (Damkier 2018).
Olanzapine may cause hyperprolactinemia, which may decrease reproductive function in both males and females.
Health care providers are encouraged to enroll women 18 to 45 years of age exposed to olanzapine during pregnancy in the Atypical Antipsychotics Pregnancy Registry (1-866-961-2388 or https://www.womensmentalhealth.org/pregnancyregistry).
Patient Education
What is this drug used for?
- It is used to treat bipolar problems.
- It is used to treat schizophrenia.
- It is used to treat low mood (depression).
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Agitation
- Loss of strength and energy
- Constipation
- Dry mouth
- Nausea
- Weight gain
- Increased appetite
- Back pain
- Injection site irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- High blood sugar like confusion, fatigue, more thirst, hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Anxiety
- Confusion
- Severe fatigue
- Weakness
- Severe headache
- Abnormal movements twitching
- Change in balance
- Difficulty swallowing
- Difficulty speaking
- Mood changes
- Thoughts of suicide
- Behavioral changes
- Severe dizziness
- Passing out
- Slow heartbeat
- Fast heartbeat
- Lack of sweating
- Seizures
- Drooling
- Vision changes
- Trouble with memory
- Chest pain
- Swelling in the arms or legs
- Burning or numbness feeling
- Swollen glands
- Enlarged breasts
- Nipple discharge
- Sexual dysfunction
- No menstrual periods
- Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, severe headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot.
- Tardive dyskinesia like unable to control body movements; tongue, face, mouth, or jaw sticking out; mouth puckering; or puffing cheeks.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.