What is Otrexup?
Otrexup is a single-dose auto-injector containing a prescription medicine, methotrexate.
Methotrexate is used to:
- treat certain adults with severe, active rheumatoid arthritis (RA), and children with active polyarticular juvenile idiopathic arthritis (pJIA), after treatment with other medicines including non-steroidal anti-inflammatory (NSAIDS) have been used and did not work well.
- control the symptoms of severe, resistant, disabling psoriasis in adults when other types of treatment have been used and did not work well.
Otrexup is available in doses of 10, 12.5, 15, 17.5, 20, 22.5 and 25 mg. Your doctor will prescribe a different way to take methotrexate if you need to take methotrexate by mouth or in some other way. Your doctor may also change your prescription if your dose does not match the available Otrexup doses, such as doses of less than 10 mg, more than 25 mg, or doses in between the available Otrexup doses.
Otrexup should not be used for the treatment of cancer.
Otrexup should not be used for the treatment of children with psoriasis.
What is the most important information I should know about Otrexup?
Otrexup can cause serious side effects that can lead to death, including:
1. Organ system toxicity. People who use methotrexate for the treatment of cancer, psoriasis, or rheumatoid arthritis, have an increased risk of death from organ toxicity. Types of organ toxicity can include:
- gastrointestinal
- bone marrow
- liver
- immune system
- nerve
- lung
- kidneys
- skin
Your doctor will do blood tests and other types of tests before you take and while you are taking Otrexup to check for signs and symptoms of organ toxicity. Call your doctor right away if you have any of the following symptoms of organ toxicity:
- vomiting
- diarrhea
- mouth sores
- fever
- confusion
- weakness
- temporary blindness
- seizures
- headache
- back pain
- neck stiffness
- paralysis
- irritability
- sleepiness
- problems with coordination
- dry cough
- trouble breathing
- severe skin rash
2. Women who are pregnant are at increased risk for death of the baby and birth defects. Women who are pregnant or who plan to become pregnant must not take Otrexup. A pregnancy test should be performed before starting Otrexup.
Contraception should be used by both females and males while taking Otrexup. Pregnancy should be avoided if either partner is receiving Otrexup:
- for a minimum of 3 months after treatment with Otrexup for males.
- during and for 6 months after treatment with Otrexup for females.
Who should not take Otrexup?
Do not take Otrexup if you:
- are pregnant or planning to become pregnant. See “What is the most important information I should know about Otrexup?"
- are breastfeeding.
- Otrexup can pass into your breast milk and may harm your baby. Do not breastfeed while taking Otrexup. Talk to your doctor about the best way to feed your baby if you take Otrexup.
- have alcohol problems (alcoholism).
- have liver problems.
- have problems fighting infection (immunodeficiency syndrome).
- have been told you have (or think you have) a blood disorder such as low levels of white blood cells, red blood cells (anemia), or platelets.
- have had an allergy to methotrexate or any of the ingredients in Otrexup. See the end of this leaflet for a complete list of ingredients in Otrexup.
Talk to your doctor before taking this medicine if you have any of these conditions.
What should I tell my healthcare provider before taking Otrexup?
Before you take Otrexup, tell your doctor if you have any other medical conditions.
Tell your doctor about all of the medicines you take, including prescription, over-the-counter medicines, vitamins, and herbal supplements.
Otrexup may affect how other medicines work, and other medicines may affect how Otrexup works causing side effects.
Ask your doctor or pharmacist for a list of medicines if you are not sure.
Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
How should I take Otrexup?
- Read the Instructions for Use that come with Otrexup.
- Take Otrexup exactly as your doctor tells you to take it.
- Inject Otrexup only 1 time each week. Do not take Otrexup every day. Taking Otrexup every day may cause death from toxicity.
- Your doctor will show you or your caregiver how to inject Otrexup. You should not inject Otrexup until you have been trained on the right way to use it.
- Check Otrexup before you inject it. Otrexup should be yellow in color and should not have any lumps or particles in it.
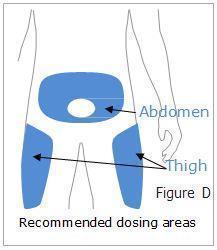
- Otrexup should be injected in the stomach (abdomen) or thigh.
- Do not inject Otrexup within 2 inches of the belly button (navel).
- Do not inject Otrexup in the arms or any other areas of the body.
- Do not inject Otrexup in areas where the skin is tender, bruised, red, scaly, hard, or has scars or stretch marks.
- If you are not sure if Otrexup was injected, or if you have hard time giving the injection, do not inject another dose. Call your pharmacist or doctor right away.
- If you inject too much Otrexup, call your doctor or go to the nearest hospital emergency room right away.
What should I avoid while taking Otrexup?
- Do not drink alcohol while taking Otrexup. Drinking alcohol can increase your chances of getting serious side effects.
- Otrexup can cause dizziness and tiredness. Do not drive a car, operate machinery, or do anything that needs you to be alert until you know how Otrexup affects you.
- Certain vaccinations should be avoided while taking Otrexup. Talk to your doctor before you or members of your household receive any vaccines.
What are the possible side effects of Otrexup?
Otrexup may cause serious side effects, including:
See “What is the most important information I should know about Otrexup?"
- fertility problems. Methotrexate, the active ingredient in Otrexup, may affect your ability to have a baby. Males may have a decreased sperm count, and females may have changes to their menstrual cycle. This can happen while taking Otrexup and for a short period of time after you stop.
- certain cancers. Some people who have taken methotrexate have had a certain type of cancer called Non-Hodgkin’s lymphoma and other tumors. Your doctor may tell you to stop taking Otrexup if this happens.
- tissue and bone problems. Taking Methotrexate while having radiation therapy may increase the risk of your tissue or bone not receiving enough blood. This may lead to death of the tissue or bone.
Common side effects of Otrexup include:
- nausea
- stomach pain
- indigestion (dyspepsia)
- mouth sores
- rash
- stuffy or runny nose and sore throat
- diarrhea
- abnormal liver function tests
- vomiting
- headache
- bronchitis
- low red, white, and platelet blood cell count
- hair loss
- dizziness
- sensitivity to light
- burning skin lesions
- lung problems
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Otrexup. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of Otrexup
Methotrexate is sometimes prescribed for purposes other than those listed in Patient Information leaflet. Do not use Otrexup for a condition for which it was not prescribed. Do not give Otrexup to other people, even if they have the same symptoms that you have. It may harm them.
This Patient Information leaflet summarizes the most important information about Otrexup. If you would like more information, talk to your doctor. You can ask your doctor or pharmacist for information about Otrexup that is written for health professionals.
For more information, go to www.Otrexup.com or call 1-855-Otrexup (1-855-687-3987).
How should I store Otrexup?
Store Otrexup at room temperature between 68°F to 77°F (20°C to 25°C).
- Do not freeze
- Keep Otrexup out of the light.
Keep Otrexup and all medicines out of the reach of children.
How should I dispose of Otrexup?
- Do not throw away in the household trash. Put used Otrexup in a FDA-cleared sharps disposal container right away after use.
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- made of a heavy-duty plastic
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out
- upright stable during use
- leak-resistant
- properly labeled to warn of hazardous waste inside the container
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about the safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA’s website at: HTTP://WWW.FDA.GOV/SAFESHARPSDISPOSAL.
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
- Safely dispose of Otrexup that is out of date or is no longer needed.
What are the ingredients in Otrexup?
Active ingredient: methotrexate
Inactive ingredients: hydrochloric acid, sodium chloride, sodium hydroxide and water for injection, USP.
Instructions for use for Otrexup
Otrexup (oh-TREKS-up)
(methotrexate) injection
for subcutaneous use
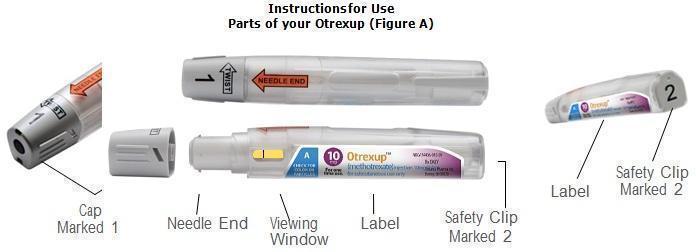
Prepare to Use Otrexup
- Do not remove cap (marked 1) or safety clip (marked 2) until you are ready to inject Otrexup.
- Wash your hands well with soap and warm water.
- Check the expiration date on the label. Do not use if expired.
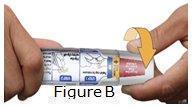
- Check the seal. Do not use Otrexup if the seal is broken (See Figure B).
- In addition to Otrexup, you will need the following items: 1 alcohol swab and 1 cotton ball or gauze.
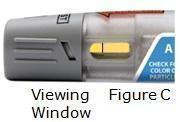
Check the Liquid
- Look at the viewing window (See Figure C).
- The liquid should be yellow in color and should not have any lumps or particles in it.
- You may see an air bubble. This is normal.
Choose an Injection Site
- Otrexup should be injected into the stomach (abdomen) or thigh. Do not inject Otrexup within 2 inches of the belly button (navel) (See Figure D).
- Do not inject Otrexup in the arms or any other areas of the body.
- Do not inject Otrexup in areas where the skin is tender, bruised, red, scaly, hard, or has scars or stretch marks.
- Wipe the area with an alcohol swab.
- Allow the skin to dry and do not touch this area again before giving Otrexup. Do not fan or blow on the clean area.
Give your Injection
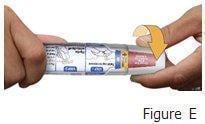
Step 1: Remove Cap (marked 1)
- Twist cap marked 1 to remove (See Figure E). This will break the seal.
- You may notice 1 or 2 drops of medicine. This is normal.
- Do not touch the needle end with your hands or fingers. This could inject the medicine into your hand.
- Do not replace the cap after it has been removed.
- After the cap is removed Otrexup must be used or disposed of safely (See step 5).
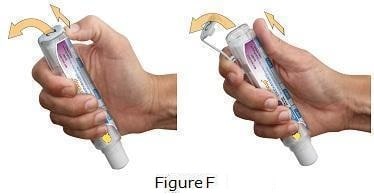
STEP 2: Remove the Safety Clip (marked 2)
- Flip the Safety Clip marked 2 (See Figure F).
STEP 3: Inject Otrexup
- Place needle end of Otrexup flat against thigh or stomach (abdomen) at a 90° and firmly push device against the injection site until fully depressed. You will hear a click, hold for 3 seconds (slowly count 1,2,3) (See Figure G).
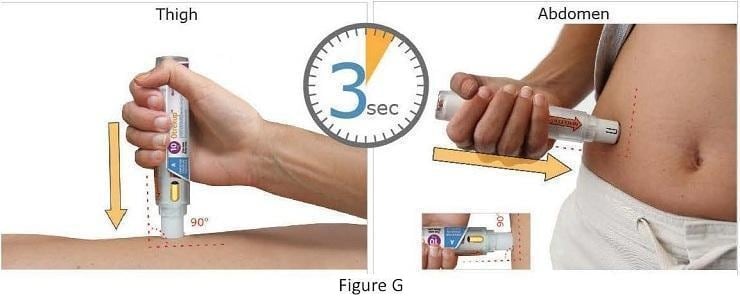
- After counting to 3, remove Otrexup from the injection site. You may notice a small amount of blood or liquid at the administration site, which is normal.
- Press a cotton ball or gauze on the area for 10 seconds. Do not rub the area.
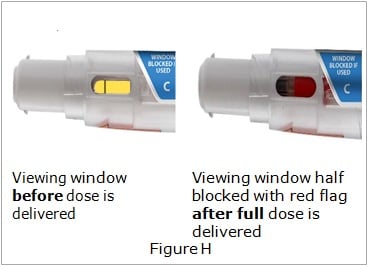
Step 4: Check the Viewing Window
- Check the viewing window (See Figure H).
- The viewing window will be half blocked with a red flag to show that the full dose was delivered. (See Figure H).
- Dispose of Otrexup in a puncture-proof disposable container (See Step 5).
- If the viewing window is not half blocked with a red flag, call your doctor or pharmacist, or call 1-855-Otrexup (1-855-687-3987) for help.
- Do not use another Otrexup without talking to your doctor.
Step 5:
Dispose of Otrexup
- Do not throw away in the household trash. Put used Otrexup in a FDA-cleared sharps disposal container right away after use.
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- made of a heavy-duty plastic
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out
- upright and stable during use
- leak-resistant
- properly labeled to warn of hazardous waste inside the container
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about the safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA’s website at: http://www.fda.gov/safesharpsdisposal.
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
- Safely dispose of Otrexup that is out of date or no longer needed.
How should I store Otrexup?
- Store Otrexup at room temperature between 68°F to 77°F (20°C to 25°C). Do not freeze.
- Keep Otrexup out of the light.





