Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension, Oral:
Trileptal: 300 mg/5 mL (250 mL) [contains alcohol, usp, methyl hydroxybenzoate, propyl hydroxybenzoate, propylene glycol, saccharin sodium; lemon flavor]
Generic: 300 mg/5 mL (250 mL)
Tablet, Oral:
Trileptal: 150 mg, 300 mg, 600 mg [scored]
Generic: 150 mg, 300 mg, 600 mg
Tablet Extended Release 24 Hour, Oral:
Oxtellar XR: 150 mg, 300 mg, 600 mg
Pharmacology
Mechanism of Action
Pharmacological activity results from both oxcarbazepine and its monohydroxy metabolite (MHD). Precise mechanism of anticonvulsant effect has not been defined. Oxcarbazepine and MHD block voltage-sensitive sodium channels, stabilizing hyperexcited neuronal membranes, inhibiting repetitive firing, and decreasing the propagation of synaptic impulses. These actions are believed to prevent the spread of seizures. Oxcarbazepine and MHD also increase potassium conductance and modulate the activity of high-voltage activated calcium channels.
Pharmacokinetics/Pharmacodynamics
Absorption
Complete
Distribution
MHD: Vd: 49 L
Metabolism
Oxcarbazepine is extensively metabolized in the liver to its active 10-monohydroxy metabolite (MHD); MHD undergoes further metabolism via glucuronide conjugation; 4% of dose is oxidized to the 10,11-dihydroxy metabolite (DHD) (inactive); 70% of serum concentration appears as MHD, 2% as unchanged oxcarbazepine, and the rest as minor metabolites; Note: Unlike carbamazepine, autoinduction of metabolism has not been observed and biotransformation of oxcarbazepine does not result in an epoxide metabolite
Excretion
Urine (95%, <1% as unchanged oxcarbazepine, 27% as unchanged MHD, 49% as MHD glucuronides, 3% as DHD (inactive), and 13% as conjugate of oxcarbazepine and MHD); feces (<4%)
Clearance (per body weight):
Children 2 to <4 years: Increased by ∼80% compared to adults
Children 4 to 12 years: Increased by ∼40% compared to adults
Children ≥13 years: Values approach adult clearance
Time to Peak
Children 2 to 12 years: Immediate release: Oxcarbazepine: 1 hour; MHD: 3 to 4 hours (Rey 2004)
Adults: Immediate release: MHD: Tablets: Median: 4.5 hours (range: 3 to 13 hours); Suspension: Median 6 hours; Extended release: MHD: 7 hours
Half-Life Elimination
Children (Rey, 2004): 2 to 5 years: MHD: Single dose: Mean range: 4.8 to 6.7 hours; 6 to 12 years: MHD: Single dose: Mean range: 7.2 to 9.3 hours
Adults: Immediate release: Parent drug: 2 hours; MHD: 9 hours; renal impairment (CrCl 30 mL/minute): MHD: 19 hours; Extended release: Parent drug: 7 to 11 hours; MHD: 9 to 11 hours
Protein Binding
Oxcarbazepine: 67%; MHD: 40%, primarily to albumin; parent drug and metabolite do not bind to alpha-1 acid glycoprotein
Use in Specific Populations
Special Populations: Renal Function Impairment
If CrCl <30 mL/minute, elimination half-life of MHD is prolonged to 19 hours and there is a 2-fold increase in AUC.
Special Populations: Elderly
Max plasma concentration and AUC values of MHD were 30% to 60% higher.
Use: Labeled Indications
Focal (partial) onset seizures:
Immediate-release: Monotherapy or adjunctive therapy in the treatment of focal (partial) onset seizures in adults, as monotherapy in the treatment of focal (partial) onset seizures in children ≥4 years of age with epilepsy, and as adjunctive therapy in children ≥2 years of age with focal (partial) onset seizures.
Extended-release: Treatment of focal (partial) onset seizures in adults and in children ≥6 years of age.
Use: Off Label
Neuropathic painbyes
Data from a multicenter, double-blind, placebo-controlled study supports the use of oxcarbazepine monotherapy in the treatment of neuropathic pain of diabetic origin Dogra 2005, Zhou 2013.
Based on the American Academy of Neurology evidence-based guidelines for the Treatment of Painful Diabetic Neuropathy, oxcarbazepine is probably not effective and should probably not be considered for the management of painful diabetic neuropathy. However, based on the International Association for the Study of Pain (IASP) evidence-based recommendations for the Pharmacologic Management of Neuropathic Pain, oxcarbazepine given for painful diabetic neuropathy is suggested for patients who have not responded to first- and second-line medications Dworkin 2007.
Based on the European Academy of Neurology guidelines for the treatment of trigeminal neuralgia, oxcarbazepine is recommended in the long-term management of primary trigeminal neuralgia EAN [Bendtsen 2019].
Contraindications
Hypersensitivity to oxcarbazepine, eslicarbazepine acetate, or any component of the formulation
Documentation of allergenic cross-reactivity for carbamazepine and analogues is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Adjunctive therapy, focal (partial) onset seizures (epilepsy): Oral:
Immediate release: Initial: 600 mg daily in 2 divided doses; dose may be increased by as much as 600 mg/day increments at weekly intervals; maximum recommended dose: 1,200 mg/day in 2 divided doses. Although doses >1,200 mg/day were somewhat more efficacious, most patients were unable to tolerate 2,400 mg/day (due to CNS effects).
Extended release: Initial: 600 mg once daily; dosage may be increased by 600 mg/day increments at weekly intervals. Recommended daily dose is 1,200 to 2,400 mg once daily. Although daily doses >1,200 mg daily were somewhat more efficacious, most patients were unable to tolerate 2,400 mg daily (due to CNS effects).
Conversion to monotherapy, focal (partial) onset seizures (epilepsy): Patients receiving concomitant antiepileptic drugs (AEDs): Oral: Immediate release: Initial: 600 mg daily in 2 divided doses while simultaneously reducing the dose of concomitant AEDs. Withdraw concomitant AEDs completely over 3 to 6 weeks, while increasing the oxcarbazepine dose in increments of 600 mg daily at weekly intervals, reaching the maximum oxcarbazepine dose (2,400 mg/day) in about 2 to 4 weeks (lower doses have been effective in patients in whom monotherapy has been initiated).
Initiation of monotherapy, focal (partial) onset seizures (epilepsy): Oral:
Immediate release: Initial: 600 mg daily in 2 divided doses. Increase dose by 300 mg daily every third day to a dose of 1,200 mg daily. Higher dosages (2,400 mg daily) have been shown to be effective in patients converted to monotherapy from other AEDs.
Extended release: Initial: 600 mg once daily; dosage may be increased by 600 mg/day increments at weekly intervals. Recommended daily dose is 1,200 to 2,400 mg once daily. Although daily doses >1,200 mg/day may be somewhat more efficacious, higher doses are associated with increased adverse effects.
Conversion from immediate release to extended release: Higher doses of extended release formulation may be necessary.
Dosage adjustment with concomitant strong CYP3A4 inducers or UGT inducers (eg, carbamazepine, phenobarbital, phenytoin, rifampin): Extended release: Consider initiating dose at 900 mg once daily.
Neuropathic pain (off-label use): Oral: Initial: 300 mg/day; increase dose after 3 days to 300 mg twice daily, then adjust dose based on response and tolerability in increments of 300 mg every 5 days up to a maximum dose of 900 mg twice daily. Mean dose during clinical trial maintenance period was 1,445 mg/day (Dogra 2005).
Dosing: Geriatric
Immediate release: Refer to adult dosing.
Extended release: Initial: 300 mg or 450 mg once daily should be considered; dosage may be increased by 300 to 450 mg daily increments at weekly intervals to desired clinical response.
Dosing: Pediatric
Note: Immediate-release preparations (oral suspension and tablets) are interchangeable on a mg per mg basis; immediate-release and extended-release preparations are not bioequivalent and not interchangeable on a mg per mg basis.
Partial-onset seizures, monotherapy: Oral: Immediate release (Trileptal):
Children ≥4 years and Adolescents ≤16 years:
Initiation of monotherapy: Patients not receiving concomitant anti-epileptic drugs (AEDs):
Initial: 8 to 10 mg/kg/day in 2 divided doses; usual initial daily dose in adults is 600 mg/day; increase dose every third day by 5 mg/kg/day to achieve the recommended monotherapy maintenance dose by weight, as follows:
Maintenance dose:
20 to <25 kg: 600 to 900 mg/day in 2 divided doses.
25 to <35 kg: 900 to 1,200 mg/day in 2 divided doses.
35 to <45 kg: 900 to 1,500 mg/day in 2 divided doses.
45 to <50 kg: 1,200 to 1,500 mg/day in 2 divided doses.
50 to <60 kg: 1,200 to 1,800 mg/day in 2 divided doses.
60 to <70 kg: 1,200 to 2,100 mg/day in 2 divided doses.
≥70 kg: 1,500 to 2,100 mg/day in 2 divided doses.
Conversion to monotherapy: Patients receiving concomitant AEDs: Initial: 8 to 10 mg/kg/day in 2 divided doses (usual initial daily dose in adults is 600 mg/day), with a simultaneous initial reduction of the dose of concomitant AEDs; withdraw concomitant AEDs completely over 3 to 6 weeks, while increasing oxcarbazepine dose as needed by no more than 10 mg/kg/day at approximately weekly intervals; increase oxcarbazepine dose to achieve the recommended monotherapy maintenance dose.
Adolescents ≥17 years:
Initiation of monotherapy: Patients not receiving prior AEDs: Initial: 300 mg twice daily. Increase dose by 300 mg/day every third day to a maintenance dose of 1,200 mg/day in 2 divided doses.
Conversion to monotherapy: Patients receiving concomitant AEDs: Initial: 300 mg twice daily while simultaneously reducing the dose of concomitant AEDs. Withdraw concomitant AEDs completely over 3 to 6 weeks, while increasing the oxcarbazepine dose in increments of 600 mg/day at weekly intervals up to target maintenance dose of 2,400 mg/day in 2 divided doses in about 2 to 4 weeks.
Partial-onset seizures, adjunctive therapy: Oral:
Immediate release (Trileptal):
Children 2 to <4 years:
Patient weight <20 kg: Initial: 8 to 10 mg/kg/day in 2 divided doses; may consider initiating at a higher dose of 16 to 20 mg/kg/day due to increased clearance in this age; increase dose slowly over 2 to 4 weeks; maximum daily dose: 60 mg/kg/day.
Patient weight ≥20 kg: Initial: 8 to 10 mg/kg/day in 2 divided doses (usual maximum initial daily dose: 600 mg/day); increase dose slowly over 2 to 4 weeks; maximum daily dose: 60 mg/kg/day.
Note: In children 2 to 4 years of age, 50% of patients were titrated to a final dose of at least 55 mg/kg/day with target dose of 60 mg/kg/day. Due to a higher drug clearance, children 2 to <4 years of age may require up to twice the dose per body weight compared to adults.
Children ≥4 years and Adolescents ≤16 years:
Initial: 8 to 10 mg/kg/day in 2 divided doses; usual maximum initial daily dose: 600 mg/day; increase dose slowly over 2 weeks to the target maintenance dose by weight, as follows:
Maintenance dose:
20 to 29 kg: 900 mg/day in 2 divided doses.
29.1 to 39 kg: 1,200 mg/day in 2 divided doses.
>39 kg: 1,800 mg/day in 2 divided doses.
Note: Use of these pediatric target maintenance doses in one clinical trial resulted in doses ranging from 6 to 51 mg/kg/day (median dose: 31 mg/kg/day) in pediatric patients 4 to 16 years of age (Glauser 2000). Due to a higher drug clearance, children 4 to ≤12 years of age may require a 50% higher dose per body weight compared to adults.
Adolescents ≥17 years: Initial: 300 mg twice daily; dose may be increased by ≤600 mg/day increments at weekly intervals up to target maintenance dose of 1,200 mg/day in 2 divided doses. Although doses >1,200 mg/day were somewhat more efficacious, most patients were unable to tolerate 2,400 mg/day (due to CNS effects).
Extended release (Oxtellar XR):
Children and Adolescents 6 to ≤16 years:
Initial: 8 to 10 mg/kg/day once daily; maximum initial daily dose: 600 mg/day during the first week of therapy. Increase dose at weekly intervals in 8 to 10 mg/kg/day increments over 2 to 3 weeks (maximum dosage incremental increase: 600 mg/dose) to the target maintenance dose based on weight, as follows:
Maintenance dose:
20 to 29 kg: 900 mg once daily.
29.1 to 39 kg: 1,200 mg once daily.
>39 kg: 1,800 mg once daily.
Adolescents ≥17 years: Initial: 600 mg once daily; dosage may be increased by 600 mg/day increments at weekly intervals. Recommended daily dose is 1,200 to 2,400 mg once daily. Although daily doses >1,200 mg daily were somewhat more efficacious, most patients were unable to tolerate 2,400 mg/day (due to CNS effects).
Conversion from immediate release (Trileptal) to extended release (Oxtellar XR): Children ≥6 years and Adolescents: Higher doses of Oxtellar XR may be necessary; on a mg per mg basis dosage forms are not bioequivalent.
Dosage adjustment with concomitant drugs: Strong inducers of CYP3A4 and/or UGT (eg, rifampin, carbamazepine, phenytoin, phenobarbital):
Immediate release: Children ≥2 years and Adolescents: During oxcarbazepine titration, monitor serum concentrations of 10-monohydroxy (MHD) metabolite (active); additional oxcarbazepine dose adjustments may be necessary if inducer initiated, dose modified or discontinued.
Extended release: Children ≥6 years and Adolescents:
Initial: Consider higher initial doses of oxcarbazepine:
6 to ≤16 years: Oral: 12 to 15 mg/kg/day once daily (maximum daily dose: 900 mg/day).
≥17 years: Oral: 900 mg/day.
Additional oxcarbazepine dose adjustments may be necessary if inducer initiated, dose modified, or discontinued.
Administration
Immediate release: Administer twice daily without regard to meals.
Suspension: Prior to using for the first time, firmly insert the plastic adapter provided with the bottle. Cover adapter with child-resistant cap when not in use. Shake bottle for at least 10 seconds, remove child-resistant cap, and insert the oral dosing syringe provided to withdraw appropriate dose. Dose may be taken directly from oral syringe or may be mixed in a small glass of water immediately prior to swallowing. Rinse syringe with warm water after use and allow to dry thoroughly. Discard any unused portion after 7 weeks of first opening bottle.
Extended release: Administer once daily on an empty stomach at least 1 hour before or 2 hours after food. Swallow whole; do not cut, crush, or chew the tablets.
Storage
Store tablets and suspension at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Store suspension in the original container; use within 7 weeks of first opening container. Dispense extended release tablets in a tight, light-resistant container; protect from light and moisture.
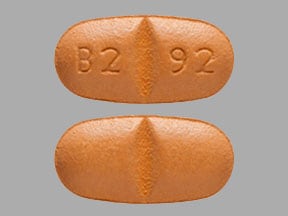
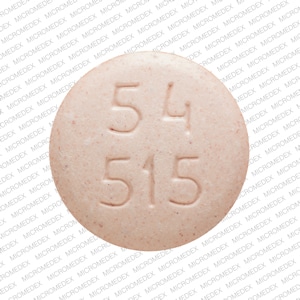
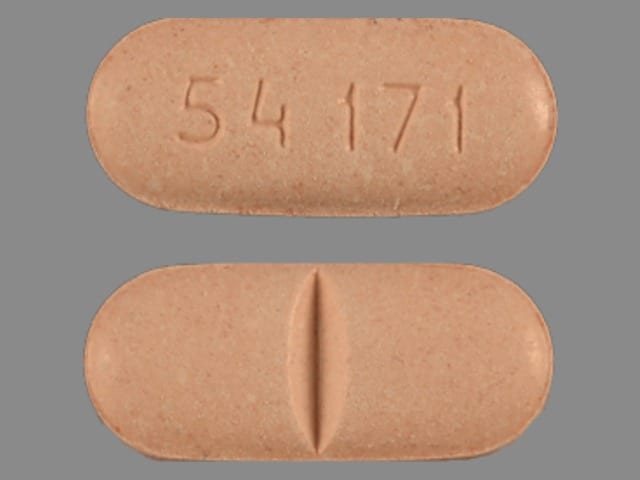
OXcarbazepine Images
Drug Interactions
Alcohol (Ethyl): May enhance the CNS depressant effect of OXcarbazepine. Monitor therapy
Bictegravir: OXcarbazepine may decrease the serum concentration of Bictegravir. Management: When possible consider using an alternative anticonvulsant with concurrent bictegravir, emtricitabine, and tenofovir alafenamide. If the combination must be used, monitor closely for evidence of reduced antiviral effectiveness. Consider therapy modification
CloZAPine: CYP3A4 Inducers (Weak) may decrease the serum concentration of CloZAPine. Monitor therapy
Cobicistat: OXcarbazepine may decrease the serum concentration of Cobicistat. Management: Consider an alternative antiepileptic when possible. Consider therapy modification
CYP3A4 Inducers (Strong): May decrease the serum concentration of OXcarbazepine. Specifically, the concentrations of the 10-monohydroxy active metabolite of oxcarbazepine may be decreased. Exceptions: Fosphenytoin; Phenytoin. Monitor therapy
Dolutegravir: OXcarbazepine may decrease the serum concentration of Dolutegravir. Avoid combination
Doravirine: OXcarbazepine may decrease the serum concentration of Doravirine. Avoid combination
Elvitegravir: OXcarbazepine may decrease the serum concentration of Elvitegravir. Management: For elvitegravir plus a ritonavir-boosted protease inhibitor, use of oxcarbazepine is not recommended; for elvitegravir/cobicistat/emtricitabine/tenofovir combination products, consider using an alternative antiepileptic when possible. Avoid combination
Eslicarbazepine: May enhance the adverse/toxic effect of OXcarbazepine. Avoid combination
Estrogen Derivatives (Contraceptive): OXcarbazepine may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
Fosphenytoin-Phenytoin: May decrease serum concentrations of the active metabolite(s) of OXcarbazepine. Specifically, concentrations of the major active 10-monohydroxy metabolite may be reduced. OXcarbazepine may increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
Lacosamide: Antiepileptic Agents (Sodium Channel Blockers) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Ledipasvir: OXcarbazepine may decrease the serum concentration of Ledipasvir. Avoid combination
LevETIRAcetam: OXcarbazepine may decrease the serum concentration of LevETIRAcetam. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Mianserin: May diminish the therapeutic effect of Anticonvulsants. Monitor therapy
NiMODipine: CYP3A4 Inducers (Weak) may decrease the serum concentration of NiMODipine. Monitor therapy
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Perampanel: May increase the serum concentration of OXcarbazepine. OXcarbazepine may decrease the serum concentration of Perampanel. Management: Increase the perampanel starting dose to 4 mg/day when perampanel is used with oxcarbazepine. Patients receiving this combination should be followed closely for response, especially with any changes to oxcarbazepine therapy. Consider therapy modification
Progestins (Contraceptive): OXcarbazepine may decrease the serum concentration of Progestins (Contraceptive). Management: Contraceptive failure is possible. Use of an additional or alternative, nonhormonal method of contraception is recommended. Consider therapy modification
Rilpivirine: OXcarbazepine may decrease the serum concentration of Rilpivirine. Avoid combination
Rivaroxaban: OXcarbazepine may decrease the serum concentration of Rivaroxaban. Monitor therapy
Selegiline: OXcarbazepine may enhance the serotonergic effect of Selegiline. Avoid combination
Simeprevir: OXcarbazepine may decrease the serum concentration of Simeprevir. Avoid combination
Sofosbuvir: OXcarbazepine may decrease the serum concentration of Sofosbuvir. Avoid combination
Tenofovir Alafenamide: OXcarbazepine may decrease the serum concentration of Tenofovir Alafenamide. Avoid combination
Thiazide and Thiazide-Like Diuretics: May enhance the adverse/toxic effect of OXcarbazepine. Specifically, there may be an increased risk for hyponatremia. Monitor therapy
Ubrogepant: CYP3A4 Inducers (Weak) may decrease the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 100 mg and second dose (if needed) of 100 mg when used with a weak CYP3A4 inducer. Consider therapy modification
Ulipristal: OXcarbazepine may decrease the serum concentration of Ulipristal. Avoid combination
Valproate Products: May decrease the serum concentration of OXcarbazepine. Monitor therapy
Test Interactions
Thyroid function tests; may depress serum T4 without affecting T3 levels or TSH
Adverse Reactions
Incidence of adverse effects is from monotherapy and adjunctive AED studies. Incidence in children was similar.
>10%:
Central nervous system: Dizziness (20% to 49%), drowsiness (12% to 36%), headache (8% to 32%), ataxia (2% to 31%), fatigue (3% to 21%), abnormal gait (3% to 17%), vertigo (2% to 15%)
Gastrointestinal: Vomiting (7% to 36%), nausea (15% to 29%), abdominal pain (5% to 13%)
Neuromuscular & skeletal: Tremor (4% to 16%)
Ophthalmic: Diplopia (10% to 40%), nystagmus (2% to 26%), visual disturbance (1% to 14%)
1% to 10%:
Cardiovascular: Chest pain (2%), edema (2%), lower extremity edema (2%), hypotension (1% to 2%)
Central nervous system: Emotional lability (3% to 8%), anxiety (7%), equilibrium disturbance (7%), confusion (2% to 7%), nervousness (2% to 7%), amnesia (4% to 5%), seizure (2% to 5%), falling (4%), abnormality in thinking (2% to 4%), insomnia (2% to 4%), hypoesthesia (3%), dysmetria (1% to 3%), speech disorder (1% to 3%), abnormal electroencephalogram (2%), agitation (2%), lack of concentration (2%), feeling abnormal (1% to 2%), myasthenia (1% to 2%)
Dermatologic: Skin rash (4%), diaphoresis (3%), acne vulgaris (1% to 2%)
Endocrine & metabolic: Hyponatremia (1% to 10%), hot flash (2%), increased thirst (2%), weight gain (2%)
Gastrointestinal: Diarrhea (7%), constipation (4% to 6%), dyspepsia (2% to 6%), anorexia (5%), dysgeusia (5%), upper abdominal pain (3%), xerostomia (3%), gastritis (2% to 3%), toothache (2%)
Genitourinary: Urinary tract infection (5%), urinary frequency (2%), vaginitis (2%)
Hematologic & oncologic: Bruise (2% to 4%), lymphadenopathy (2%), purpuric rash (2%), rectal hemorrhage (2%)
Hypersensitivity: Hypersensitivity reaction (2%)
Infection: Viral infection (7%), infection (2%)
Neuromuscular & skeletal: Asthenia (2% to 7%), back pain (4%), muscle spasm (2%), sprain (2%)
Ophthalmic: Blurred vision (4%), accommodation disturbance (2%)
Otic: Otalgia (2%), otic infection (2%)
Respiratory: Upper respiratory tract infection (7% to 10%), rhinitis (5% to 10%), cough (5%), epistaxis (4%), pulmonary infection (4%), sinusitis (3% to 4%), bronchitis (3%), nasopharyngitis (3%), pharyngitis (3%), pneumonia (2%)
Miscellaneous: Fever (3%), head trauma (2%)
Frequency not defined:
Cardiovascular: Bradycardia, cardiac failure, flushing, hypertension, orthostatic hypotension, palpitations, syncope, tachycardia
Central nervous system: Aggressive behavior, apathy, aphasia, aura, cerebral hemorrhage, delirium, delusions, dystonia, euphoria extrapyramidal reaction, hemiplegia, hyperkinesia, hyperreflexia, hypertonia, hypokinesia, hyporeflexia, hypotonia, hysteria, impaired consciousness, intoxicated feeling, malaise, manic behavior, migraine, neuralgia, nightmares, oculogyric crisis, panic disorder, paralysis, paranoia, personality disorder, precordial pain, psychomotor retardation, psychosis, rigors, speech disturbance, stupor, voice disorder
Dermatologic: Alopecia, contact dermatitis, eczema, erythematosus rash, facial rash, folliculitis, genital pruritus, maculopapular rash, miliaria, psoriasis, skin photosensitivity, urticaria, vitiligo
Endocrine & metabolic: Change in libido, decreased T4, heavy menstrual bleeding, hyperglycemia, hypocalcemia, hypoglycemia, hypokalemia, increased gamma-glutamyl transferase, intermenstrual bleeding, weight loss
Gastrointestinal: Aphthous stomatitis, biliary colic, bloody stools, cholelithiasis, colitis, duodenal ulcer, dysphagia, enteritis, eructation, esophagitis, flatulence, gastric ulcer, gingival hemorrhage, gingival hyperplasia, hematemesis, hemorrhoids, hiccups, increased appetite, retching, sialadenitis, stomatitis
Genitourinary: Dysuria, hematuria, leukorrhea, priapism, urinary tract pain
Hematologic & oncologic: Thrombocytopenia
Hepatic: Increased liver enzymes
Hypersensitivity: Angioedema
Neuromuscular & skeletal: Right hypochondrium pain, systemic lupus erythematosus, tetany
Ophthalmic: Blepharoptosis, cataract, conjunctival hemorrhage, hemianopia, mydriasis, ocular edema, photophobia, scotoma, xerophthalmia
Otic: Otitis externa, tinnitus
Renal: Nephrolithiasis, polyuria, renal pain
Respiratory: Asthma, dyspnea, laryngismus, pleurisy
<1%, postmarketing, and/or case reports: Acute generalized exanthematous pustulosis, agranulocytosis, anaphylaxis, aplastic anemia, atrioventricular block, bone fracture (long-term therapy), decreased bone mineral density (long-term therapy), DRESS syndrome, dysarthria, erythema multiforme, hepatitis (Hsu 2010), hypothyroidism, increased serum amylase, increased serum lipase, leukopenia, osteoporosis (long-term therapy), pancreatitis, pancytopenia, SIADH, Stevens-Johnson syndrome, suicidal ideation, suicidal tendencies, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- Blood dyscrasias: Agranulocytosis, leukopenia, and pancytopenia have been reported with use (rare); discontinuation and conversion to alternate therapy may be required.
- Bone disorders: Long term use has been associated with decreased bone mineral density, osteopenia, osteoporosis, and fractures.
- CNS effects: Use has been associated with CNS-related adverse events, most significant of these were cognitive symptoms including psychomotor slowing, difficulty with concentration, and speech or language problems, somnolence or fatigue, and coordination abnormalities, including ataxia and gait disturbances. Caution patients about performing tasks which require mental alertness (eg, operating machinery or driving).
- Dermatologic reactions: Potentially serious, sometimes fatal, dermatologic reactions (eg, Stevens-Johnson, toxic epidermal necrolysis) have been reported in adults and children; the median time to onset was 19 days after treatment initiation. Monitor for signs and symptoms of skin reactions; discontinuation and conversion to alternate therapy may be required. Recurrence of serious skin reactions have been reported with oxcarbazepine rechallenge.
- Hepatic dysfunction: Hepatitis has been reported rarely (Hsu 2010). Promptly evaluate any symptoms of hepatic dysfunction (eg, anorexia, nausea/vomiting, right upper quadrant pain, pruritus) and discontinue therapy immediately if significant abnormalities are confirmed.
- Hypersensitivity reactions: Rare cases of anaphylaxis and angioedema have been reported, even after initial dosing; permanently discontinue should symptoms occur. Use caution in patients with previous hypersensitivity to carbamazepine (cross-sensitivity occurs in 25% to 30% of patients). Potentially serious, sometimes fatal drug reaction with eosinophilia and systemic symptoms (DRESS) also known as multiorgan hypersensitivity reactions have also been reported in close association with initiation of oxcarbazepine; monitor for signs and symptoms of possible disparate manifestations associated with lymphatic, hepatic, renal, cardiovascular, and/or hematologic organ systems; discontinuation and conversion to alternate therapy may be required.
- Hyponatremia: Clinically significant hyponatremia (serum sodium <125 mmol/L) and syndrome of inappropriate antidiuretic hormone secretion (SIADH) may develop during use; generally develops in the first 3 months of therapy but may occur >1 year after treatment initiation. Measure serum sodium concentration if hyponatremia symptoms develop (eg, nausea, malaise, headache, lethargy, confusion, impaired consciousness, seizures). Consider monitoring serum sodium during treatment, especially in patients at risk for hyponatremia (eg, elderly patients, concomitant use of medications known to lower sodium levels). Dosage reduction, discontinuation of therapy or fluid restriction may be considered in patients that develop hyponatremia.
- Hypothyroidism: Hypothyroidism has been reported; consider monitoring thyroid function, particularly in pediatric patients. Discontinuation of therapy has been associated with return of normal thyroxine levels.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; patients should be instructed to notify healthcare provider immediately if symptoms occur.
Disease-related concerns:
- Cardiovascular disease: Clinical trials excluded patients with significant cardiovascular disease or ECG abnormalities. Monitor body weight/fluid retention in patients with HF; evaluate serum sodium with worsening cardiac function or fluid retention.
- Renal impairment: Single-dose studies show that half-life of the primary active metabolite is prolonged 3- to 4-fold and AUC is doubled in patients with CrCl <30 mL/minute; dose adjustment required in these patients.
- Seizure disorder: Exacerbation of or new onset primary generalized seizures has been reported, particularly in children. In case of seizure aggravation, discontinue oxcarbazepine.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Asian ancestry: Consider screening patients of Asian descent for the variant human leukocyte antigen (HLA) allele B*1502 prior to initiating therapy. This genetic variant has been associated with a significantly increased risk of developing Stevens-Johnson syndrome and/or toxic epidermal necrolysis in patients receiving carbamazepine. Structural similarity of oxcarbazepine to carbamazepine, available clinical evidence, and data from nonclinical studies showing a direct interaction of oxcarbazepine with the HLA-B*1502 protein suggest patients receiving oxcarbazepine may also be at a similar risk. Consider avoiding use of oxcarbazepine in patients with a positive result. Screening is not recommending in low-risk populations or in current oxcarbazepine patients (risk usually during first few months of therapy).
Other warnings/precautions:
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal.
Monitoring Parameters
Seizure frequency; serum sodium as deemed necessary (particularly during first 3 months of therapy); symptoms of CNS depression (dizziness, headache, somnolence); hypersensitivity reactions. Additional serum sodium monitoring recommended during maintenance treatment in patients receiving other medications known to decrease sodium levels, in patients with signs/symptoms of hyponatremia, and in patients with an increase in seizure frequency or severity. Periodic thyroid function tests (particularly pediatric patients) and CBC. Monitor for suicidality (eg, suicidal thoughts, depression, behavioral changes). Serum levels of concomitant antiepileptic drugs during titration as necessary.
Pregnancy
Pregnancy Considerations
Oxcarbazepine, the active metabolite MHD and the inactive metabolite DHD, crosses the placenta and can be detected in the newborn (Myllynen 2001).
According to the manufacturer, limited data collected from pregnancy registries suggest congenital malformations may be associated with oxcarbazepine monotherapy, including craniofacial defects (such as oral clefts) and cardiac malformations (such as ventricular septal defects). However, use of oxcarbazepine in pregnancy is limited in comparison to other antiepileptic drugs and additional information may be needed to evaluate specific birth defects and other pregnancy outcomes (de Jong 2016; Martinez Ferri 2018; Tomson 2019; Weston 2016). In general, the risk of teratogenic effects is higher with AED polytherapy than monotherapy (Harden 2009). In case reports, symptoms similar to neonatal abstinence syndrome have been observed in newborns following in utero oxcarbazepine exposure (Chen 2017; Rolnitsky 2013).
Due to pregnancy-induced physiologic changes, plasma concentrations of the active metabolite, MHD, gradually decrease during pregnancy; patients should be monitored during pregnancy and postpartum.
Oxcarbazepine may decrease plasma concentrations of hormonal contraceptives. Use of an additional, nonhormonal contraceptive or alternative nonhormonal birth control is recommended.
Data collection to monitor pregnancy and infant outcomes following exposure to oxcarbazepine is ongoing. Patients exposed to oxcarbazepine during pregnancy are encouraged to enroll themselves into the NAAED Pregnancy Registry by calling 1-888-233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to help control certain kinds of seizures.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Nausea
- Vomiting
- Lack of appetite
- Abdominal pain
- Dizziness
- Fatigue
- Tremors
- Anxiety
- Trouble sleeping
- Change in taste
- Common cold symptoms
- Diarrhea
- Constipation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Swelling in your throat
- Infection
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Low sodium like headache, difficulty focusing, trouble with memory, confusion, weakness, seizures, or change in balance.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Change in amount of urine passed
- Unable to pass urine
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Swollen glands
- Severe muscle pain
- Severe muscle weakness
- Severe joint pain
- Severe joint swelling
- Confusion
- Difficulty focusing
- Vision changes
- Change in speech
- Chest pain
- Severe loss of strength and energy
- Bruising
- Bleeding
- Involuntary eye movements
- Trouble with memory
- Abnormal gait
- Change in balance
- Agitation
- Irritability
- Panic attacks
- Behavioral changes
- Mood changes
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.