Boxed Warning
Gastrointestinal events:
Severe diarrhea occurred in 25% of panobinostat treated patients. Monitor for symptoms, institute antidiarrheal treatment, interrupt panobinostat, and then reduce dose or discontinue panobinostat.
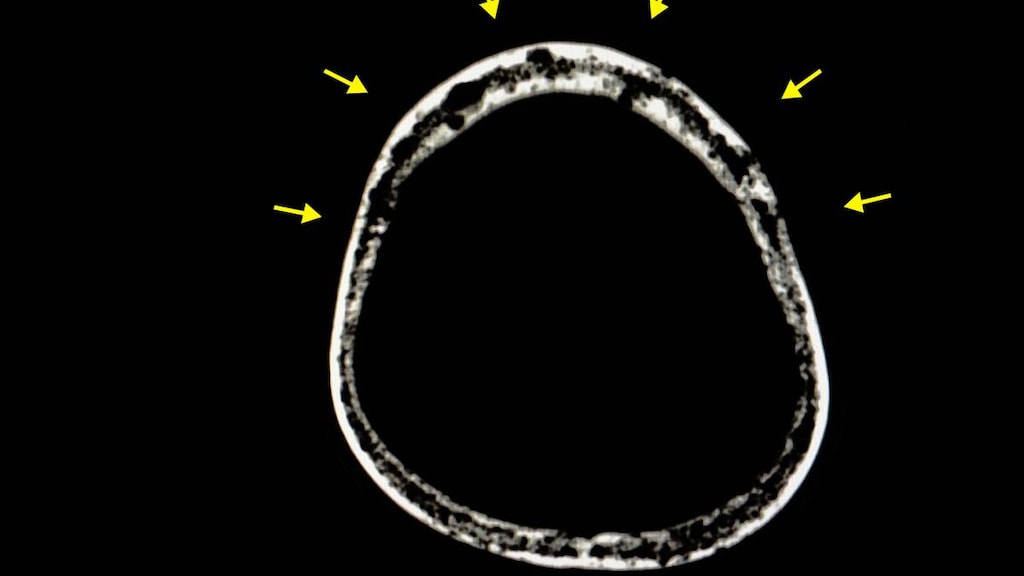
Cardiovascular events:
Severe and fatal cardiac ischemic events, severe arrhythmias, and ECG changes have occurred in patients receiving panobinostat. Arrhythmias may be exacerbated by electrolyte abnormalities. Obtain ECG and electrolytes at baseline and periodically during treatment as clinically indicated.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Farydak: 10 mg [contains brilliant blue fcf (fd&c blue #1)]
Farydak: 15 mg, 20 mg
Pharmacology
Mechanism of Action
Panobinostat is a histone deacetylase (HDAC) inhibitor; inhibits enzymatic activity of HDACs resulting in increased acetylation of histone proteins. Accumulation of acetylated histones and other proteins induces cell cycle arrest and/or apoptosis of some transformed cells. Panobinostat has minimal activity in multiple myeloma as a single-agent; however, synergistic activity is demonstrated when combined with bortezomib and dexamethasone (San-Miguel 2014).
Pharmacokinetics/Pharmacodynamics
Metabolism
Extensive via reduction, hydrolysis, oxidation, and glucuronidation; CYP3A accounts for ~40 % of elimination, CYP2D6 and CYP2C19 are minor pathways.
Excretion
Feces (44% to 77%; <4% as unchanged drug); Urine (29% to 51%; <3% as unchanged drug)
Time to Peak
Within 2 hours
Half-Life Elimination
~37 hours
Protein Binding
~90%; to plasma proteins
Use in Specific Populations
Special Populations: Renal Function Impairment
In patients with mild, moderate, and severe renal impairment, the AUC was 64%, 99%, and 59% of the normal renal function group, respectively.
Special Populations: Hepatic Function Impairment
In patients with mild and moderate hepatic impairment, the AUC was increased 43% and 105%, respectively (compared with patients with normal hepatic function).
Use: Labeled Indications
Multiple myeloma: Treatment of multiple myeloma (in combination with bortezomib and dexamethasone) in patients who have received at least 2 prior regimens, including bortezomib and an immunomodulatory agent.
Contraindications
There are no contraindications listed in the manufacturer’s labeling.
Dosage and Administration
Dosing: Adult
Determine QTcF prior to the start of therapy and verify that QTcF <450 msec prior to panobinostat initiation. Baseline ANC should be at least 1,500/mm3 and platelets at least 100,000/mm3 prior to treatment. Panobinostat is associated with a moderate emetic potential; consider antiemetics to prevent nausea and vomiting.
Multiple myeloma: Adults: Oral: 20 mg once every other day for 3 doses each week during weeks 1 and 2 of a 21-day treatment cycle (eg, Monday, Wednesday, and Friday of weeks 1 and 2 only, rest during week 3) for up to 8 cycles (in combination with bortezomib and dexamethasone); treatment may continue (the same schedule for panobinostat; bortezomib and dexamethasone schedules are modified) for an additional 8 cycles in patients experiencing clinical benefit and acceptable toxicity (San-Miguel 2014). The total duration of therapy may be up to 16 cycles (48 weeks).
Missed doses: Missed doses may be taken up to 12 hours after the scheduled time. Do not repeat the dose if vomiting occurs; patients should take the next usual scheduled dose.
Dosage adjustment for concomitant therapy:
CYP2D6 substrates: Avoid coadministration with sensitive CYP2D6 substrates (eg, atomoxetine, desipramine, dextromethorphan, metoprolol, nebivolol, perphenazine, tolterodine, venlafaxine) or CYP2D6 substrates that have a narrow therapeutic index (eg, thioridazine, pimozide).
Strong CYP3A inducers: Avoid concomitant use with strong CYP3A inducers.
Strong CYP3A inhibitors: Reduce the starting panobinostat dose to 10 mg with strong CYP3A inhibitors (eg, boceprevir, clarithromycin, conivaptin, indinavir, itraconazole, ketoconazole, lopinavir/ritonavir, nefazodone, nelfinavir, posaconazole, ritonavir, saquinavir, telaprevir, telithromycin, voriconazole).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
If dose reductions are necessary, keep the same treatment schedule and reduce panobinostat dose in increments of 5 mg (from 20 mg to 15 mg, from 15 mg to 10 mg); if dose reduction below 10 mg 3 times a week is necessary, discontinue treatment.
Hematologic toxicity:
Thrombocytopenia:
Grade 3 (platelets <50,000/mm3): No dosage adjustments are necessary; monitor platelets weekly.
Grade 3 (platelets <50,000/mm3) with bleeding: Interrupt panobinostat treatment, monitor platelets weekly until platelets ≥50,000/mm3 and then restart panobinostat at a reduced dose. (Interrupt bortezomib until platelets ≥50,000/mm3; if only 1 dose omitted, restart bortezomib at the same dose; if ≥2 consecutive doses or doses within the same cycle are omitted, then restart bortezomib at a reduced dose.)
Grade 4 (platelets <25,000/mm3): Interrupt panobinostat treatment, monitor platelets weekly until platelets ≥50,000/mm3 and then restart panobinostat at a reduced dose. (Interrupt bortezomib until platelets ≥50,000/mm3; if only 1 dose omitted, restart bortezomib at the same dose; if ≥2 consecutive doses or doses within the same cycle are omitted, then restart bortezomib at a reduced dose.)
Severe thrombocytopenia: Consider platelet transfusions. Discontinue panobinostat if thrombocytopenia does not improve despite treatment modifications or if repeated platelet transfusions are required.
Neutropenia:
Grade 3 (ANC 750 to 1,000/mm3): No dosage adjustments are necessary.
Grade 3 (ANC 500 to 750/mm3 [2 or more occurrences]): Interrupt panobinostat treatment until ANC ≥1,000/mm3 and then restart at the same dose. (Bortezomib dosage adjustment is not necessary.)
Grade 3 (ANC <1,000/mm3) with neutropenic fever: Interrupt panobinostat treatment until neutropenic fever resolves and ANC ≥1,000/mm3 and then restart at a reduced dose. (Interrupt bortezomib until neutropenic fever resolves and ANC ≥1,000/mm3; if only 1 dose omitted, restart bortezomib at the same dose; if ≥2 consecutive doses or doses within the same cycle are omitted, then restart bortezomib at a reduced dose.)
Grade 4 (ANC <500/mm3): Interrupt panobinostat treatment until ANC ≥1,000/mm3 and then restart at a reduced dose. (Interrupt bortezomib until ANC ≥1,000/mm3; if only 1 dose omitted, restart bortezomib at the same dose; if ≥2 consecutive doses or doses within the same cycle are omitted, then restart bortezomib at a reduced dose.)
Neutropenia, grade 3 or 4: Consider growth factor support or dose modification; if neutropenia does not improve or if severe infection occurs despite dose modification or growth factor support, discontinue panobinostat.
Anemia: Grade 3 (hemoglobin <8 g/dL): Interrupt panobinostat until hemoglobin ≥10 g/dL and then restart at a reduced dose.
Nonhematologic toxicity:
Cardiovascular: QTcF increase to ≥480 msec: Interrupt panobinostat treatment; correct electrolyte abnormalities. If QT prolongation does not resolve then permanently discontinue panobinostat.
Diarrhea:
First sign of abdominal cramping, loose stools, or onset of diarrhea: Begin antidiarrheal medication (eg, loperamide).
Grade 2 (moderate diarrhea; 4 to 6 stools per day): Interrupt panobinostat until resolved and then restart at the same dose. (Consider interruption of bortezomib until resolved and then restart at the same dose.)
Grade 3 (severe diarrhea; ≥7 stools per day, IV fluids or hospitalization required): Interrupt panobinostat treatment until resolved and then restart at a reduced dose. (Interrupt bortezomib until resolved and then restart at a reduced dose.)
Grade 4 (life-threatening): Permanently discontinue panobinostat. (Permanently discontinue bortezomib.)
Infection: Consider interrupting or discontinuing panobinostat.
Nausea or vomiting (panobinostat is associated with nausea and vomiting; consider prophylactic antiemetics):
Severe nausea (grades 3/4): Interrupt panobinostat treatment until resolved and then restart at a reduced dose.
Severe/life-threatening vomiting (grades 3/4): Interrupt panobinostat treatment until resolved and then restart at a reduced dose.
Other toxicities:
Grade 3 or 4 toxicity or recurrent grade 2 toxicity: Withhold panobinostat treatment until recovery to grade 1 or less and then restart at a reduced dose.
Recurrent grade 3 or 4 toxicity: Withhold panobinostat treatment until recovery to grade 1 or less and then restart at a reduced dose.
Administration
Panobinostat is associated with a moderate emetic potential; consider antiemetics to prevent nausea and vomiting. Administer orally at approximately the same time on scheduled days. May administer with or without food. Swallow capsule whole with a cup of water. Do not open, crush, or chew the capsules. Avoid exposure to crushed and/or broken capsules. Avoid direct skin or mucous membrane contact with powder inside the capsules; if contact occurs, wash thoroughly.
Dietary Considerations
Avoid star fruit, pomegranate or pomegranate juice, and grapefruit or grapefruit juice.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Store blister pack in original carton. Protect from light.
Drug Interactions
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP2D6 Substrates (High risk with Inhibitors): Panobinostat may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Panobinostat. Avoid combination
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Panobinostat. Management: Reduce the panobinostat dose to 10 mg when it must be used with a strong CYP3A4 inhibitor. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dolasetron: May enhance the arrhythmogenic effect of Panobinostat. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Granisetron: May enhance the arrhythmogenic effect of Panobinostat. Monitor therapy
Grapefruit Juice: May increase the serum concentration of Panobinostat. Avoid combination
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Ondansetron: May enhance the arrhythmogenic effect of Panobinostat. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Perhexiline: CYP2D6 Inhibitors (Weak) may increase the serum concentration of Perhexiline. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Pomegranate: May increase the serum concentration of Panobinostat. Avoid combination
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Star Fruit: May increase the serum concentration of Panobinostat. Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Adverse Reactions
Frequency not always defined.
>10%:
Cardiovascular: Abnormal T waves on ECG (40%), peripheral edema (29%; grades 3/4: 2%), depression of ST segment on ECG (22%), cardiac arrhythmia (12%; grades 3/4: 3%)
Central nervous system: Fatigue (≤60%, grades 3/4: ≤25%), lethargy (≤60%; grades 3/4: ≤25%), malaise (≤60%; grades 3/4: ≤25%)
Endocrine & metabolic: Hypocalcemia (67%; grades 3/4: 5%), hypoalbuminemia (63%; grades 3/4: 2%), hypophosphatemia (63%; grades 3/4: 20%), hypokalemia (52%; grades 3/4: 18%), hyponatremia (49%; grades 3/4: 13%), hyperphosphatemia (29%; grades 3/4: 2%), hypermagnesemia (27%; grades 3/4: 5%), weight loss (12%; grades 3/4: 2%)
Gastrointestinal: Diarrhea (68%; grades 3/4: 25%), nausea (36%; grades 3/4: 6%), decreased appetite (28%; grades 3/4: 3%), vomiting (26%; grades 3/4: 7%)
Hematologic & oncologic: Thrombocytopenia (97%; grades 3/4: 67%), lymphocytopenia (82%; grades 3/4: 53%), leukopenia (81%; grades 3/4: 23%), neutropenia (75%; grades 3/4: 34%), anemia (62%; grades 3/4: 18%)
Hepatic: Hyperbilirubinemia (21%; grades 3/4: 1%)
Infection: Severe infection (31%; includes bacterial, fungal, and viral infections)
Neuromuscular & skeletal: Weakness (≤60%; grades ≥3: ≤25%)
Renal: Increased serum creatinine (41%; grades 3/4: 1%)
Miscellaneous: Fever (26%)
1% to 10%:
Cardiovascular: Hypertension (>2% to <10%), hypotension (>2% to <10%), orthostatic hypotension (>2% to <10%), palpitations (>2% to <10%), syncope (>2% to <10%), ischemic heart disease (4%), ECG changes, prolonged Q-T interval on ECG
Central nervous system: Chills (>2% to <10%), dizziness (>2% to <10%), headache (>2% to <10%), insomnia (>2% to <10%)
Dermatologic: Cheilitis (>2% to <10%), erythema (>2% to <10%), skin lesion (>2% to <10%), skin rash (>2% to <10%)
Endocrine & metabolic: Dehydration (>2% to <10%), fluid retention (>2% to <10%), hyperglycemia (>2% to <10%), hyperuricemia (>2% to <10%), hypomagnesemia (>2% to <10%), hypothyroidism (>2% to <10%)
Gastrointestinal: Abdominal distention (>2% to <10%), abdominal pain (>2% to <10%), colitis (>2% to <10%), dysgeusia (>2% to <10%), dyspepsia (>2% to <10%), flatulence (>2% to <10%), gastritis (>2% to <10%), gastrointestinal pain (>2% to <10%), xerostomia (>2% to <10%), gastrointestinal toxicity
Genitourinary: Urinary incontinence (>2% to <10%)
Hematologic & oncologic: Hemorrhage (grades 3/4: 4%)
Hepatic: Hepatitis B (>2% to <10%), increased serum alkaline phosphatase (>2% to <10%), increased serum transaminases, increased serum bilirubin
Infection: Sepsis (6%)
Neuromuscular & skeletal: Joint swelling (>2% to <10%), tremor (>2% to <10%)
Renal: Increased blood urea nitrogen (>2% to <10%), mean glomerular filtration rate decreased (>2% to <10%), renal failure (>2% to <10%)
Respiratory: Cough (>2% to <10%), dyspnea (>2% to <10%), rales (>2% to <10%), respiratory failure (>2% to <10%), wheezing (>2% to <10%)
Warnings/Precautions
Concerns related to adverse events:
- Bone marrow suppression: Severe thrombocytopenia, neutropenia and anemia have occurred. May require treatment interruption, dosage modification, discontinuation, transfusion or granulocyte colony-stimulating factor support. Monitor CBC with differential at baseline and during treatment. Patients >65 years may require more frequent monitoring.
- Cardiovascular events: [US Boxed Warning]: Severe and fatal cardiac ischemic events, severe arrhythmias, and ECG changes have occurred in patients receiving panobinostat. Arrhythmias may be exacerbated by electrolyte abnormalities. Obtain ECG and electrolytes at baseline and periodically during treatment as clinically indicated. ECG abnormalities including ST-segment depression and T-wave abnormalities have been observed. Monitor and correct electrolyte abnormalities as needed. Panobinostat may prolong the QT interval. Do not initiate treatment in patients with a QTcF >450 msec or with clinically significant baseline ST-segment or T-wave abnormalities. Interrupt treatment if QTcF increases to ≥480 msec; correct electrolyte abnormalities; if QT prolongation does not resolve, permanently discontinue panobinostat. Concomitant use with medications known to prolong the QT interval is not recommended. Do not initiate panobinostat treatment in patients with a history of recent MI or unstable angina.
- Gastrointestinal events: [US Boxed Warning]: Severe diarrhea occurred in one-fourth of panobinostat treated patients. Monitor for symptoms, institute antidiarrheal treatment, interrupt panobinostat, and then reduce dose or discontinue panobinostat. Any grade diarrhea was reported in over two-thirds of patients and may occur at any time. Monitor hydration status and serum electrolytes (including magnesium, potassium, and phosphate). Patients should have antidiarrheal medications available for use; begin antidiarrheal medications at the first sign of diarrhea, loose stools, or abdominal cramping. Interrupt panobinostat treatment for moderate diarrhea (4 to 6 stools per day). Panobinostat is associated with nausea and vomiting (moderate emetic potential); consider antiemetics to prevent nausea and vomiting. Some antiemetics known to prolong the QT interval (eg, dolasetron or ondansetron) may be used with frequent ECG monitoring.
- Hemorrhage: Serious and fatal hemorrhage has occurred, including grade 3 and 4 hemorrhage. All patients with hemorrhage also experienced thrombocytopenia at the time of hemorrhage.
- Hepatotoxicity: Hepatic dysfunction (transaminase and total bilirubin elevations) has been reported. Monitor liver function prior to and during treatment. If liver function tests are abnormal, consider dosage adjustments and monitor until liver function returns to normal or baseline. Initial dose should be reduced in patients with mild-to-moderate hepatic impairment; avoid use in patients with severe impairment.
- Infection: Localized and systemic infections (including pneumonia, bacterial infections, invasive fungal infections, and viral infections) have been observed; infections may be severe (or fatal). Do not initiate treatment in patients with active infections. Monitor for sings/symptoms of infections during treatment. If infection occurs, begin appropriate management and consider interrupting or discontinuing panobinostat.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
CBC with differential and platelets (prior to treatment initiation then weekly or more often if clinically indicated during treatment); serum electrolytes, including potassium and magnesium prior to treatment and during treatment (in the clinical trial, electrolytes were monitored prior to the start of each cycle, after the fifth panobinostat dose in week 2 through cycle 8 and then at the beginning of cycles 9 to 16); liver function tests at baseline and regularly during treatment; pregnancy test (in women of reproductive potential, rule out pregnancy prior to and intermittently during treatment); ECG (prior to treatment initiation and periodically as clinically indicated during treatment); hydration status; monitor for gastrointestinal toxicity (eg, diarrhea, nausea, vomiting), signs/symptoms of hemorrhage and/or infection.
Pregnancy
Pregnancy Considerations
Adverse events were observed in animal reproduction studies. Pregnancy should be ruled out prior to treatment. Women of reproductive potential should avoid pregnancy and use an effective contraceptive during therapy and for at least 3 months after the last panobinostat dose. Males should use condoms during therapy and for at least 6 months after the last dose of panobinostat.
Patient Education
What is this drug used for?
- It is used to treat multiple myeloma.
Frequently reported side effects of this drug
- Lack of appetite
- Weight loss
- Nausea
- Vomiting
- Loss of strength and energy
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Diarrhea
- Abdominal cramps
- Abnormal heartbeat
- Infection
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any bleeding that is very bad or that will not stop
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, very bad dizziness or passing out, fast heartbeat, more thirst, seizures, feeling very tired or weak, not hungry, unable to pass urine or change in the amount of urine produced, dry mouth, dry eyes, or nausea or vomiting
- Liver problems like dark urine, feeling tired, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or change in eyesight
- Skin discoloration
- Chest pain
- Slow heartbeat
- Fast heartbeat
- Dizziness
- Passing out
- Pale skin
- Severe headache
- Shortness of breath
- Swelling of arms or legs
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.