Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Zemplar: 1 mcg, 2 mcg [contains alcohol, usp]
Generic: 1 mcg, 2 mcg, 4 mcg
Solution, Intravenous:
Zemplar: 2 mcg/mL (1 mL); 5 mcg/mL (1 mL, 2 mL) [contains alcohol, usp, propylene glycol]
Generic: 2 mcg/mL (1 mL); 5 mcg/mL (1 mL, 2 mL)
Pharmacology
Mechanism of Action
Decreased renal conversion of vitamin D to its primary active metabolite (1,25-hydroxyvitamin D) in chronic renal failure leads to reduced activation of vitamin D receptor (VDR), which subsequently removes inhibitory suppression of parathyroid hormone (PTH) release; increased serum PTH (secondary hyperparathyroidism) reduces calcium excretion and enhances bone resorption. Paricalcitol is a synthetic vitamin D analog which binds to and activates the VDR in kidney, parathyroid gland, intestine and bone, thus reducing PTH levels and improving calcium and phosphate homeostasis.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd:
Healthy subjects: Oral: 34 L; IV: 24 L
Stage 3 and 4 CKD: Oral: 44 to 46 L
Stage 5 CKD: Oral: 38 to 49 L; IV: 31 to 35 L
Metabolism
Hydroxylation and glucuronidation via hepatic and nonhepatic enzymes, including CYP24, CYP3A4, UGT1A4; forms metabolites (at least one active)
Excretion
Healthy subjects: Feces (oral: 70%; IV: 63%); urine (oral: 18%, IV: 19%); 51% to 59% as metabolites
Time to Peak
Plasma: 3 hours: Delayed by food
Half-Life Elimination
Healthy subjects: Oral: 4 to 6 hours; IV: 5 to 7 hours
Stage 3 and 4 CKD: Oral: 17 to 20 hours
Stage 5 CKD (on HD or PD): Oral: 14 to 18 hours; IV: 14 to 15 hours
Protein Binding
>99%
Use in Specific Populations
Special Populations: Renal Function Impairment
Compared with healthy subjects, chronic kidney disease subjects on dialysis showed a decreased clearance and increased half-life.
Use: Labeled Indications
IV: Prevention and treatment of secondary hyperparathyroidism in adults and pediatric patients 5 years and older with chronic kidney disease (CKD) on dialysis
Oral: Prevention and treatment in adults and pediatric patients 10 years and older with secondary hyperparathyroidism associated with stage 3 and 4 CKD and stage 5 CKD patients on hemodialysis or peritoneal dialysis
Contraindications
Hypersensitivity to paricalcitol or any component of the formulation; vitamin D toxicity; hypercalcemia
Documentation of allergenic cross-reactivity for vitamin D analogues is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Note: KDIGO guidelines do not recommend routine use of vitamin D analogs in patients not on dialysis with chronic kidney disease (CKD) stages G3 to G5; it may be reasonable to reserve use for patients with CKD stages G4 or G5 and with severe and progressive hyperparathyroidism. Caution is advised to avoid hypercalcemia or elevated phosphate levels (KDIGO 2017).
Secondary hyperparathyroidism in patients with chronic kidney disease on dialysis:
IV: Initial: 0.04 to 0.1 mcg/kg (2.8 to 7 mcg) given no more frequently than every other day at any time during dialysis; adjust dose based on serum intact PTH (iPTH), as follows:
iPTH above target and increased: Increase by 2 to 4 mcg every 2 to 4 weeks; maximum dose: 0.24 mcg/kg/day
iPTH above target and decreased by <30%: Increase by 2 to 4 mcg every 2 to 4 weeks; maximum dose: 0.24 mcg/kg/day
iPTH above target and decreased by 30% to 60%: Maintain paricalcitol dose
iPTH above target and decreased by >60%: Decrease paricalcitol dose based on clinical judgement
iPTH at target and stable: Maintain paricalcitol dose
Note: Dose suspension may be necessary due to persistent and abnormally low iPTH or serum calcium persistently above normal; restart therapy at a reduced dose after iPTH and/or serum calcium has normalized.
Oral: Initial dose is calculated, in mcg, based on baseline iPTH level divided by 80 and administered 3 times weekly, no more frequently than every other day. Note: To reduce the risk of hypercalcemia initiate only after baseline serum calcium has been adjusted to ≤9.5 mg/dL.
Dose titration:
Titration dose (mcg) = Most recent iPTH level (pg/mL) divided by 80
Note: In situations where monitoring of iPTH, calcium, and phosphorus occurs less frequently than once per week, a more modest initial and dose titration rate may be warranted:
Modest titration dose (mcg) = Most recent iPTH level (pg/mL) divided by 100
Dosage adjustment for elevated serum calcium: Decrease dose by 2 to 4 mcg.
Secondary hyperparathyroidism associated with stage 3 and 4 CKD: Adults: Oral: Initial dose based on baseline serum iPTH:
iPTH ≤500 pg/mL: 1 mcg once daily or 2 mcg 3 times/week
iPTH >500 pg/mL: 2 mcg once daily or 4 mcg 3 times/week
Dosage adjustment based on iPTH level relative to baseline, adjust dose at 2- to 4-week intervals:
iPTH same or increased: Increase paricalcitol dose by 1 mcg once daily or 2 mcg 3 times/week
iPTH decreased by <30%: Increase paricalcitol dose by 1 mcg once daily or 2 mcg 3 times/week
iPTH decreased by ≥30% and ≤60%: Maintain paricalcitol dose
iPTH decreased by >60%: Decrease paricalcitol dose by 1 mcg once daily* or 2 mcg 3 times/week
iPTH <60 pg/mL: Decrease paricalcitol dose by 1 mcg once daily* or 2 mcg 3 times/week
*If patient is taking 1 mcg once daily and further dose reduction is needed, decrease to 1 mcg 3 times/week. If further dose reduction is required, withhold therapy as needed and restart at a lower dosing frequency.
Dosing: Geriatric
Refer to adult dosing. Use with caution and initiate at the lower end of the dosage range.
Dosing: Pediatric
Note: KDIGO guidelines suggest that in children vitamin D analogs may be considered to maintain serum calcium levels in an age-appropriate normal range, which differs from recommendation in adult patients (KDIGO 2017).
Secondary hyperparathyroidism associated with stage 5 chronic renal failure (CKD):
Oral:
Children ≥10 years and Adolescents ≤16 years:
Initial dose: Calculate based on intact parathyroid hormone (iPTH) serum levels using the following equation. Round the calculated dose down to the nearest whole number and administer calculated dose 3 times/week and no more frequently than every other day.
Initial dose (mcg) = baseline iPTH (pg/ml) divided by 120.
Titration: Every 4 weeks, may increase dose by 1 mcg/dose (eg, increase from 1 mcg 3 times/week to 2 mcg 3 times/week) to maintain iPTH within target range. Based on response and clinical markers (iPTH, serum Ca, and P), each administered dose may be decreased 2 mcg/dose at any time. If dosage reduction is required while receiving 1 or 2 mcg 3 times/week, discontinue therapy and resume when appropriate.
Adolescents ≥17 years: Note: To reduce the risk of hypercalcemia, initiate only after baseline serum calcium has been adjusted to ≤9.5 mg/dL. In patients where laboratory markers are monitored less frequently than once weekly, more modest dosing should be used.
Initial dose: Calculate based on iPTH serum levels using the following equation and administer calculated dose 3 times/week and no more frequently than every other day.
Initial dose (mcg) = baseline iPTH (pg/mL) divided by 80.
Titration: Adjust mcg dose based on at least weekly labs (iPTH, Ca, and P); administer calculated dose 3 times/week and not more often than every other day.
iPTH level (pg/mL) based: Dose (mcg) = Most recent iPTH level (pg/mL) divided by 80.
Elevated serum calcium: Decrease dose by 2 to 4 mcg.
For modest dosing adjustments: In situations where monitoring of iPTH, calcium, and phosphorus occurs less frequently than once per week, a more modest initial and dose titration rate may be warranted. Calculate based on iPTH serum levels using the following equation and administer calculated dose 3 times/week and no more frequently than every other day.
Modest dose (mcg) = Most recent iPTH level (pg/mL) divided by 100.
Parenteral: Children ≥5 years and Adolescents: IV through HD access (not directly into vein):
Initial: Dose based on baseline serum iPTH; administer 3 times weekly at any time during dialysis session, and no more frequently than every other day:
iPTH <500 pg/mL: 0.04 mcg/kg/dose.
iPTH ≥500 pg/mL: 0.08 mcg/kg/dose.
Dosing adjustment: Prior to any paricalcitol dosing adjustments, ensure serum Ca is within normal limits. The dose of paricalcitol should be adjusted based on iPTH levels relative to baseline and targets as follows:
Above target and iPTH level decreased by <30%: Increase paricalcitol dose by 0.04 mcg/kg/dose every 2 to 4 weeks.
iPTH level ≥150 pg/mL and decreased by ≥30% to ≤60%: Maintain current paricalcitol dose.
iPTH level <150 pg/mL or decreased by >60%: Decrease weekly paricalcitol dose by 0.04 mcg/kg or by 50% if decreased dose is zero.
Secondary hyperparathyroidism associated with stage 3 and 4 chronic renal failure (CKD):
Children ≥10 years and Adolescents ≤16 years: Oral: Initial: 1 mcg 3 times/week no more frequently than every other day; may titrate every 4 weeks; increase dose by 1 mcg (eg, increase from 1 mcg 3 times/week to 2 mcg 3 times/week) to maintain iPTH within target range. Based on response and clinical markers (iPTH, serum Ca, and P), each administered dose may be decreased by 1 mcg at any time. If dosage reduction is required while receiving 1 mcg 3 times/week, discontinue therapy, resuming when appropriate.
Adolescents ≥17 years: Note: If using 3 times/week dosing, doses should not be administered more frequently than every other day:
Initial: Dose based on baseline serum iPTH: Oral:
iPTH ≤500 pg/mL: 1 mcg once daily or 2 mcg 3 times/week.
iPTH >500 pg/mL: 2 mcg once daily or 4 mcg 3 times/week.
Titration and dosage adjustment: May adjust at 2- to 4-week intervals based on iPTH level relative to baseline:
iPTH same or increased: Increase paricalcitol dose by 1 mcg once daily or 2 mcg 3 times/week.
iPTH decreased by <30%: Increase paricalcitol dose by 1 mcg once daily or 2 mcg 3 times/week.
iPTH decreased by ≥30% and ≤60%: Maintain paricalcitol dose.
iPTH decreased by >60%: Decrease paricalcitol dose by 1 mcg/day or 2 mcg 3 times/week (see Note).
iPTH <60 pg/mL: Decrease paricalcitol dose by 1 mcg/day or 2 mcg 3 times/week (see Note).
Note: If patient is taking the lowest dose (1 mcg) on the daily regimen and an additional dose reduction is necessary, then regimen should be changed to 1 mcg 3 times weekly. If further reduction is required, withhold drug as needed and restart at a lower dose.
Administration
Oral: Administer with or without food. With the 3 times/week dosing schedule, doses should not be given more frequently than every other day.
IV: Administer as a bolus dose at any time during dialysis. May be administered through a hemodialysis vascular access port or intravenously if an access port is unavailable. Doses should not be administered more often than every other day.
Dietary Considerations
Some products may contain coconut or palm kernel oil.
Storage
Store at 25°C (77°F); excursions permitted between 15°C to 30°C (59°F to 86°F).
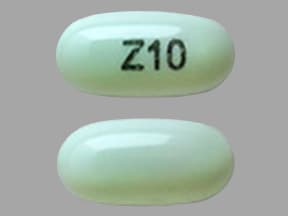
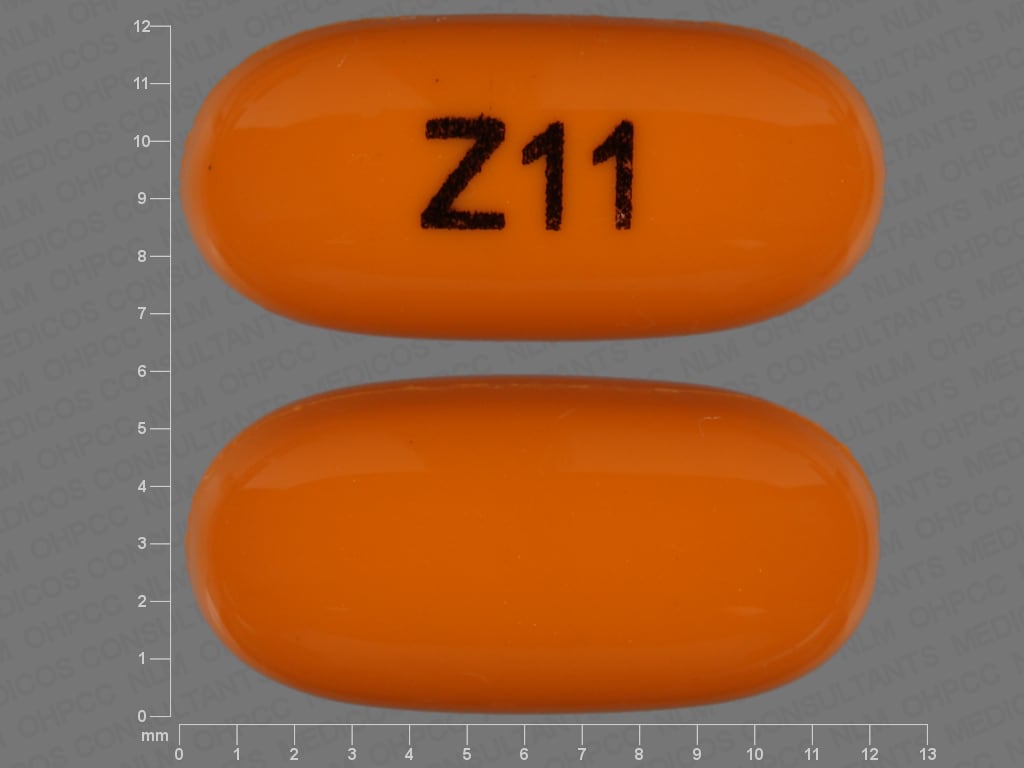
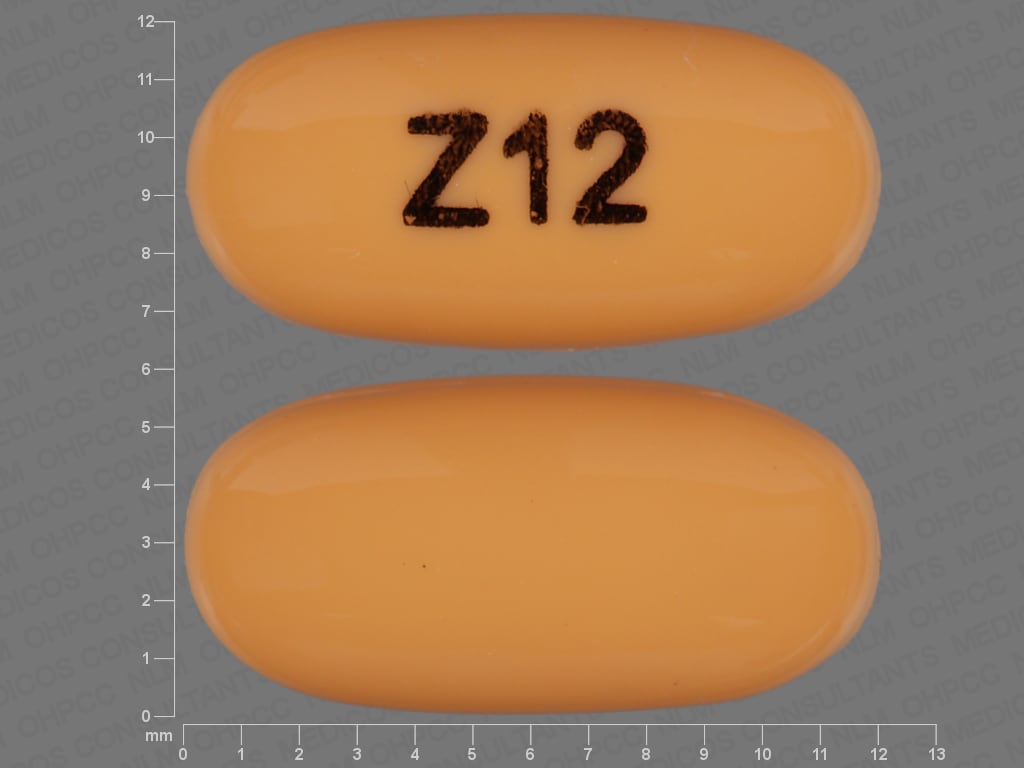
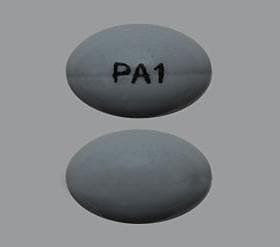
Paricalcitol Images
Drug Interactions
Aluminum Hydroxide: Vitamin D Analogs may increase the serum concentration of Aluminum Hydroxide. Specifically, the absorption of aluminum may be increased, leading to increased serum aluminum concentrations. Avoid combination
Bile Acid Sequestrants: May decrease the serum concentration of Vitamin D Analogs. More specifically, bile acid sequestrants may impair absorption of Vitamin D Analogs. Management: Avoid concomitant administration of vitamin D analogs and bile acid sequestrants (eg, cholestyramine). Separate administration of these agents by several hours to minimize the potential risk of interaction. Monitor plasma calcium concentrations. Consider therapy modification
Burosumab: Vitamin D Analogs may enhance the adverse/toxic effect of Burosumab. Avoid combination
Calcium Salts: May enhance the adverse/toxic effect of Vitamin D Analogs. Monitor therapy
Cardiac Glycosides: Vitamin D Analogs may enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Paricalcitol. Monitor therapy
Danazol: May enhance the hypercalcemic effect of Vitamin D Analogs. Monitor therapy
Digoxin: Paricalcitol may enhance the adverse/toxic effect of Digoxin. Monitor therapy
Erdafitinib: Serum Phosphate Level-Altering Agents may diminish the therapeutic effect of Erdafitinib. Management: Avoid coadministration of serum phosphate level-altering agents with erdafitinib before initial dose increase period based on serum phosphate levels (Days 14 to 21). Consider therapy modification
Mineral Oil: May decrease the serum concentration of Vitamin D Analogs. More specifically, mineral oil may interfere with the absorption of Vitamin D Analogs. Management: Avoid concomitant, oral administration of mineral oil and vitamin D analogs. Consider separating the administration of these agents by several hours to minimize the risk of interaction. Monitor plasma calcium concentrations. Consider therapy modification
Multivitamins/Fluoride (with ADE): May enhance the adverse/toxic effect of Vitamin D Analogs. Avoid combination
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the adverse/toxic effect of Vitamin D Analogs. Avoid combination
Orlistat: May decrease the serum concentration of Paricalcitol. Management: Monitor clinical response to paricalcitol closely when used with orlistat. When this combination must be used, consider administering paricalcitol at least 1 hour before or 4 to 6 hours after the administration of orlistat Consider therapy modification
Sucralfate: Vitamin D Analogs may increase the serum concentration of Sucralfate. Specifically, the absorption of aluminum from sucralfate may be increased, leading to an increase in the serum aluminum concentration. Avoid combination
Thiazide and Thiazide-Like Diuretics: May enhance the hypercalcemic effect of Vitamin D Analogs. Monitor therapy
Vitamin D Analogs: May enhance the adverse/toxic effect of other Vitamin D Analogs. Avoid combination
Test Interactions
In predialysis patients, paricalcitol may increase serum creatinine and therefore decrease the estimated GFR (eGFR).
Adverse Reactions
As reported in adults, unless otherwise noted.
>10%:
Gastrointestinal: Nausea (children, adolescents, and adults: 5% to 13%), diarrhea (7% to 12%)
Infection: Infection (bacterial, fungal, viral: 3% to 15%)
Respiratory: Rhinitis (children and adolescents: 17%)
1% to 10%:
Cardiovascular: Hypertension (7%), edema (6% to 7%), hypotension (5%), palpitations (3%), chest pain (3%), peripheral edema (3%), syncope (3%), atrial flutter (<2%), cardiac arrhythmia (<2%), cerebrovascular accident (<2%), chest discomfort (<2%), ischemic bowel disease (<2%)
Central nervous system: Dizziness (5% to 7%), chills (5%), insomnia (5%), vertigo (5%), headache (3% to 5%), anxiety (3%), depression (3%), fatigue (3%), malaise (3%), abnormal gait (<2%), agitation (<2%), confusion (<2%), delirium (<2%), hypoesthesia (<2%), myoclonus (<2%), nervousness (<2%), paresthesia (<2%), restlessness (<2%)
Dermatologic: Skin rash (4% to 6%), dermal ulcer (3%), ecchymoses (3%), acne vulgaris (<2%), alopecia (<2%), burning sensation of skin (<2%), extravasation reactions (<2%), night sweats (<2%), pruritus (<2%), urticaria (<2%)
Endocrine & metabolic: Hypervolemia (5%), dehydration (3%), hypoglycemia (3%), hirsutism (<2%), hypercalcemia (<2%), hyperkalemia (<2%), hyperparathyroidism (<2%), hyperphosphatemia (<2%), hypocalcemia (<2%), hypoparathyroidism (<2%), increased thirst (<2%), weight loss (<2%)
Gastrointestinal: Vomiting (5% to 8%), gastrointestinal hemorrhage (5%), peritonitis (5%), constipation (4% to 5%), abdominal pain (4%), dyspepsia (3%), xerostomia (3%), decreased appetite (<2%), dysgeusia (<2%), dysphagia (<2%), gastritis (<2%), gastroesophageal reflux disease (<2%)
Genitourinary: Urinary urgency (children and adolescents: 6%), chronic renal failure (3%), uremia (3%), urinary tract infection (3%), erectile dysfunction (<2%), mastalgia (<2%), vaginal infection (<2%)
Hematologic & oncologic: Anemia (<2%), lymphadenopathy (<2%), malignant neoplasm of breast (<2%), prolonged bleeding time (<2%), rectal hemorrhage (<2%)
Hepatic: Abnormal hepatic function tests (<2%), increased serum AST (<2%)
Hypersensitivity: Hypersensitivity reaction (6%)
Infection: Influenza (5%), sepsis (5%)
Local: Pain at injection site (<2%)
Neuromuscular & skeletal: Arthralgia (5%), arthritis (5%), weakness (3% to 5%), back pain (3% to 4%), leg cramps (3%), muscle spasm (3%), joint stiffness (<2%), muscle twitching (<2%), myalgia (<2%)
Ophthalmic: Conjunctivitis (children and adolescents: 6%; adults: <2%), glaucoma (<2%), ocular hyperemia (<2%)
Otic: Otalgia (<2%)
Respiratory: Nasopharyngitis (8%), asthma (children and adolescents: 6%), pneumonia (5%), oropharyngeal pain (4%), bronchitis (3%), cough (3%), sinusitis (3%), dyspnea (<2%), orthopnea (<2%), pulmonary edema (<2%), upper respiratory tract infection (<2%), wheezing (<2%)
Miscellaneous: Fever (3% to 5%), laboratory test abnormality (<2%), swelling (<2%)
<1%, postmarketing, and/or case reports: Angioedema (including laryngeal edema), increased serum creatinine
Warnings/Precautions
Concerns related to adverse effects:
- Excessive vitamin D: Excessive vitamin D administration may lead to over suppression of PTH, progressive or acute hypercalcemia, hypercalciuria, hyperphosphatemia and adynamic bone disease.
- Hypercalcemia: Progressive and/or acute hypercalcemia may increase risk of cardiac arrhythmias and seizures; chronic hypercalcemia may lead to generalized vascular and other soft-tissue calcification, exacerbate nephrolithiasis, and has been associated with increased mortality in adults with chronic kidney disease (CKD) (KDIGO 2017). High intake of calcium and phosphate with vitamin D (and its derivatives) may increase risk of hypercalciuria and hyperphosphatemia. Risk of hypercalcemia may be increased by concomitant use of calcium-containing supplements, other vitamin D compounds, and/or medications that increase serum calcium (eg, thiazide diuretics). Monitor serum calcium frequently in high risk patients.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information
Monitoring Parameters
Signs and symptoms of vitamin D intoxication and hypercalcemia.
Serum calcium and phosphorus:
IV: Serum calcium twice weekly during initial phase, then at least monthly once dose established
Oral: Serum calcium and phosphorus at baseline, at least every 2 weeks for initial 3 months or following dose adjustment, then monthly for 3 months, then every 3 months
Serum or plasma intact PTH (iPTH):
IV: Every 2 to 4 weeks during initial phase or after dose adjustment
Oral: Baseline, at least every 2 weeks for 3 months or following dose adjustment, then monthly for 3 months, then every 3 months
KDIGO guidelines (2017):
Serum calcium, phosphorus, and parathyroid hormone (PTH): Frequency of measurement may be dependent upon the presence and magnitude of abnormalities, the rate of progression of chronic kidney disease (CKD), and the use of treatments for chronic kidney disease-mineral and bone disorder (CKD-MBD) (KDIGO 2017):
CKD stage G3a to G3b: Serum calcium and phosphate: Every 6 to 12 months; PTH: Frequency based on baseline level and progression of CKD
CKD stage G4: Serum calcium and phosphate: Every 3 to 6 months; PTH: Every 6 to 12 months
CKD stage G5 and G5D: Serum calcium and phosphate: Every 1 to 3 months; PTH: Every 3 to 6 months
Pregnancy
Pregnancy Considerations
Adverse events have been observed in some animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat high parathyroid hormone levels in certain patients.
Frequently reported side effects of this drug
- Diarrhea
- Nausea
- Vomiting
- Nose irritation
- Throat irritation
- Joint pain
- Eye redness
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High calcium like weakness, confusion, fatigue, headache, nausea and vomiting, constipation, or bone pain.
- Severe headache
- Severe dizziness
- Passing out
- Vision changes
- Abnormal heartbeat
- Seizures
- Passing a lot of urine
- Weight loss
- Vomiting blood
- Chills
- Lack of appetite
- Increased thirst
- Black, tarry, or bloody stools
- Swelling
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.