Boxed Warning
Suicidal thoughts and behaviors:
Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric and young adult patients in short-term studies. Closely monitor all antidepressant-treated patients for clinical worsening and for emergence of suicidal thoughts and behaviors. Paroxetine is not approved for use in pediatric patients.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral, as mesylate [strength expressed as base]:
Brisdelle: 7.5 mg [contains fd&c red #40, fd&c yellow #6 (sunset yellow)]
Generic: 7.5 mg
Suspension, Oral, as hydrochloride [strength expressed as base]:
Paxil: 10 mg/5 mL (250 mL) [contains fd&c yellow #6 aluminum lake, methylparaben, propylene glycol, propylparaben, saccharin sodium; orange flavor]
Tablet, Oral, as hydrochloride [strength expressed as base]:
Paxil: 10 mg [scored]
Paxil: 10 mg [scored; contains fd&c blue #2 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Paxil: 20 mg [scored]
Paxil: 20 mg [scored; contains fd&c blue #2 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Paxil: 30 mg
Paxil: 30 mg [contains fd&c blue #2 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Paxil: 40 mg
Paxil: 40 mg [contains fd&c blue #2 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Generic: 10 mg, 20 mg, 30 mg, 40 mg
Tablet, Oral, as mesylate [strength expressed as base]:
Pexeva: 10 mg, 20 mg
Pexeva: 20 mg [DSC] [scored]
Pexeva: 30 mg, 40 mg
Tablet Extended Release 24 Hour, Oral, as hydrochloride [strength expressed as base]:
Paxil CR: 12.5 mg [contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Paxil CR: 25 mg
Paxil CR: 37.5 mg [contains fd&c blue #2 aluminum lake]
Generic: 12.5 mg, 25 mg, 37.5 mg
Pharmacology
Mechanism of Action
Paroxetine is a selective serotonin reuptake inhibitor, chemically unrelated to tricyclic, tetracyclic, or other antidepressants; presumably, the inhibition of serotonin reuptake from brain synapse stimulated serotonin activity in the brain
Pharmacokinetics/Pharmacodynamics
Absorption
Completely absorbed following oral administration
Distribution
Vd: 8.7 L/kg (3 to 28 L/kg)
Metabolism
Extensively hepatic via CYP2D6 enzymes; primary metabolites are formed via oxidation and methylation of parent drug, with subsequent glucuronide/sulfate conjugation; nonlinear pharmacokinetics (via 2D6 saturation) may be seen with higher doses and longer duration of therapy. Metabolites exhibit ~2% potency of parent compound. Cmin concentrations are 70% to 80% greater in the elderly compared to nonelderly patients; clearance is also decreased.
Excretion
Urine (64%, 2% as unchanged drug); feces (36% primarily via bile, <1% as unchanged drug)
Onset of Action
Depression: The onset of action is within a week, however, individual response varies greatly and full response may not be seen until 8-12 weeks after initiation of treatment; antiobsessional and antipanic effects: Up to several weeks
Time to Peak
Capsules: Median: 6 hours (range: 3 to 8 hours)
Tablets, oral suspension: Immediate release: Mean: 5.2 to 8.1 hours
Tablets: Controlled release: 6 to 10 hours
Half-Life Elimination
Paxil: 21 hours; Paxil CR: 15 to 20 hours; Pexeva: 33.2 hours
Protein Binding
93% to 95%
Use in Specific Populations
Special Populations: Renal Function Impairment
Mean plasma concentrations increased approximately 4 times, with CrCl <30 mL/minute. Plasma concentrations increased 2-fold with CrCl 30 to 60 mL/minute.
Special Populations: Hepatic Function Impairment
2-fold increase in plasma concentrations; reduce the dose in patients with severe hepatic impairment; no dosage adjustment is necessary with Brisdelle.
Special Populations: Elderly
Minimum concentrations were 70% to 80% greater than in younger patients. Reduce initial dosage; no dosage adjustment is necessary with Brisdelle.
Use: Labeled Indications
Generalized anxiety disorder (immediate release): Treatment of generalized anxiety disorder.
Major depressive disorder (unipolar) (immediate and extended release): Treatment of unipolar major depressive disorder.
Obsessive-compulsive disorder (immediate release): Treatment of obsessions and compulsions in patients with obsessive-compulsive disorder.
Panic disorder (immediate and extended release): Treatment of panic disorder, with or without agoraphobia.
Posttraumatic stress disorder (immediate release): Treatment of posttraumatic stress disorder.
Premenstrual dysphoric disorder (extended release): Treatment of premenstrual dysphoric disorder.
Social anxiety disorder (immediate and extended release): Treatment of social anxiety disorder, also known as social phobia.
Vasomotor symptoms of menopause (immediate release; 7.5 mg capsule): Treatment of moderate to severe vasomotor symptoms associated with menopause.
Use: Off Label
Body dysmorphic disorderyes
Based on the National Institute for Health and Care Excellence (NICE) guidelines for the treatment of obsessive-compulsive disorder and body dysmorphic disorder, selective serotonin reuptake inhibitors given as monotherapy or in combination with cognitive behavior therapy are recommended in the management of body dysmorphic disorder in adults with moderate or severe functional impairment, respectively.
Premature ejaculationbyes
Data from a meta-analysis of 35 clinical trials involving the use of serotonergic antidepressants, 9 of which were double-blind or open-label clinical trials using paroxetine, support the use of daily paroxetine in the treatment of premature ejaculation Waldinger 2004. Two single-blind trials also support on-demand dosing regimens Abu El-Hamd 2018, McMahon 1999.
According to the
Contraindications
Hypersensitivity (eg, anaphylaxis, angioedema, Stevens-Johnson syndrome) to paroxetine or any component of the formulation; concurrent use with or within 14 days of monoamine oxidase inhibitors (including linezolid or methylene blue IV); concomitant use with pimozide or thioridazine; pregnancy (Brisdelle only).
Dosage and Administration
Dosing: Adult
Note: Dose: In patients sensitive to side effects, some experts suggest a lower starting dose of 5 to 10 mg once daily (immediate release [IR]) or 12.5 mg once daily (extended release [ER]) and gradual titration in increments of no more than 10 mg (immediate release) or 12.5 mg (extended release), particularly in patients with anxiety who are generally more sensitive to overstimulation effects (eg, anxiety, insomnia) with antidepressants (Hirsch 2019c; Siris 2019; Stein 2019b; WFSBP [Bandelow 2012]). Dosage forms: Paroxetine is available as IR and ER formulations; both formulations are dosed once daily but are not interchangeable on a mg to mg basis. Where dosing for the ER formulation is not provided for an indication, may convert between formulations using equivalence shown in Dosing conversions section below.
Body dysmorphic disorder (off-label use): Dosing recommendations based on expert opinion: Immediate release: Oral: Initial: 20 mg once daily; may increase dose gradually based on response and tolerability in increments of 20 mg/day at intervals of every 2 to 3 weeks to a usual dose of 60 mg/day; doses up to 100 mg/day may be necessary in some patients for optimal response, typically under specialist care. Note: An adequate trial for assessment of effect in body dysmorphic disorder is 12 to 16 weeks, including maximum tolerated doses for at least 3 to 4 of those weeks (Phillips 2019).
Generalized anxiety disorder: Immediate release: Oral: Initial: 10 mg once daily; may increase dose based on response and tolerability in increments of 10 mg/day at intervals ≥1 week up to 50 mg/day (Pollack 2001; WFSBP [Bandelow 2012]).
Major depressive disorder (unipolar):
Immediate release: Oral: Initial: 20 mg once daily; may increase dose based on response and tolerability in increments of 10 to 20 mg/day at intervals ≥1 week to a maximum of 50 mg/day (Hirsch 2019b).
Extended release: Oral: Initial: 25 mg once daily; may increase dose based on response and tolerability in increments of 12.5 mg/day at intervals ≥1 week to a maximum of 62.5 mg/day.
Obsessive-compulsive disorder: Immediate release: Oral: Initial: 20 mg once daily; may increase dose based on response and tolerability in increments of 10 mg/day at intervals ≥1 week up to a recommended dose of 40 to 60 mg/day; maximum dose: 60 mg/day (APA [Koran 2007]). Note: An adequate trial for assessment of effect in obsessive-compulsive disorder is considered ≥6 weeks at the maximum tolerated dose (Issari 2016).
Panic disorder:
Immediate release: Oral: Initial: 10 mg once daily for 3 to 7 days; may increase dose based on response and tolerability in increments of 10 mg/day at intervals ≥1 week up to a usual dose of 20 to 40 mg/day (APA [Stein 2009]); maximum dose: 60 mg/day.
Extended release: Oral: Initial: 12.5 mg once daily; may increase dose based on response and tolerability in increments of 12.5 mg/day at intervals ≥1 week up to a maximum of 75 mg/day.
Posttraumatic stress disorder: Immediate release: Oral: Initial: 20 mg once daily; may increase dose based on response and tolerability in increments of 10 to 20 mg/day at intervals ≥1 week up to 60 mg/day (Marshall 2007; Stein 2019a).
Premature ejaculation (off-label use): Immediate release: Oral: Initial: 10 mg once daily; may increase dose based on response and tolerability in increments of 10 mg/day at intervals ≥1 week to a usual dosage of 20 mg/day (Waldinger 2001). Some patients may require up to 40 mg/day for optimal response (ISSM [Althof 2014]; Waldinger 1997); some experts suggest 3- to 4-week titration intervals (Khera 2019).
Premenstrual dysphoric disorder: Note: Some experts prefer selective serotonin reuptake inhibitors (SSRIs) other than paroxetine for this use (Casper 2019).
Continuous daily dosing regimen:
Immediate release (off-label): Oral: Initial: 10 mg once daily; increase to usual effective dose of 20 mg once daily over the first month; in a subsequent menstrual cycle, a further increase to 40 mg/day may be necessary in some patients for optimal response (Casper 2019).
Extended release: Oral: Initial: 12.5 mg once daily; increase to usual effective dose of 25 mg once daily over the first month; in a subsequent menstrual cycle, a further increase to 50 mg/day (based on equivalent IR dose) may be necessary in some patients for optimal response (Casper 2019).
Intermittent regimens:
Luteal phase dosing regimen:
Immediate release (off-label): Oral: Initial: 10 mg once daily during the luteal phase of menstrual cycle only (ie, beginning therapy 14 days before anticipated onset of menstruation and continued to the onset of menses); over the first month, may increase to usual effective dose of 20 mg once daily during the luteal phase; in a subsequent menstrual cycle, a further increase to 30 mg/day during the luteal phase may be necessary in some patients for optimal response (Casper 2019).
Extended release: Oral: Initial: 12.5 mg once daily during the luteal phase of menstrual cycle only (ie, beginning therapy 14 days before anticipated onset of menstruation and continued to the onset of menses); over the first month, may increase to usual effective dose of 25 mg once daily during the luteal phase; in a subsequent menstrual cycle, a further increase to 37.5 mg/day (based on equivalent IR dose) during the luteal phase may be necessary in some patients for optimal response (Casper 2019).
Symptom-onset dosing regimen (off-label): Immediate release: Oral: Initial: 10 mg once daily from the day of symptom onset until a few days after the start of menses; over the first month, may increase dose based on response and tolerability up to 20 mg/day; in a subsequent menstrual cycle, a further increase to 30 mg/day may be necessary in some patients for optimal response (Casper 2019).
Social anxiety disorder:
Immediate release: Oral: Initial: 10 mg once daily; may increase dose based on response and tolerability in increments of 10 mg/day at intervals ≥1 week to a maximum of 60 mg/day (Baldwin 1999; Liebowitz 2002; Mancini 1996; Stein 1998).
Extended release: Oral: Initial: 12.5 mg once daily; may increase dose based on response and tolerability in increments of 12.5 mg/day at intervals ≥1 week up to a maximum of 37.5 mg/day (manufacturer's labeling). Note: Doses up to 75 mg/day (based on equivalent IR dose) may be necessary in some patients for optimal response (Liebowitz 2002).
Vasomotor symptoms of menopause (alternative agent): Note: Nonhormonal alternative in patients unable or unwilling to take estrogen (AACE [Goodman 2011]).
Immediate release:
Capsule: Oral: 7.5 mg once daily at bedtime.
Tablet (off-label): Oral: 10 to 20 mg once daily at bedtime (Stearns 2005; Slaton 2015).
Extended release (off-label): Oral: 12.5 to 25 mg once daily at bedtime (Stearns 2003; Slaton 2015).
Dosing conversions: Immediate release 10 mg is equivalent to extended release 12.5 mg (DeVane 2003).
Discontinuation of therapy: When discontinuing antidepressant treatment that has lasted for >3 weeks, gradually taper the dose (eg, over 2 to 4 weeks) to minimize withdrawal symptoms and detect reemerging symptoms (APA 2010; WFSBP [Bauer 2015]). Reasons for a slower titration (eg, over 4 weeks) include use of a drug with a half-life <24 hours (eg, paroxetine, venlafaxine), prior history of antidepressant withdrawal symptoms, or high doses of antidepressants (APA 2010; Hirsch 2019a). If intolerable withdrawal symptoms occur, resume the previously prescribed dose and/or decrease dose at a more gradual rate (Shelton 2001). Select patients (eg, those with a history of discontinuation syndrome) on long-term treatment (>6 months) may benefit from tapering over >3 months (WFSBP [Bauer 2015]). Evidence supporting ideal taper rates is limited (Shelton 2001; WFSBP [Bauer 2015]).
Switching antidepressants: Evidence for ideal antidepressant switching strategies is limited; strategies include cross-titration (gradually discontinuing the first antidepressant while at the same time gradually increasing the new antidepressant) and direct switch (abruptly discontinuing the first antidepressant and then starting the new antidepressant at an equivalent dose or lower dose and increasing it gradually). Cross-titration (eg, over 1 to 4 weeks depending upon sensitivity to discontinuation symptoms and adverse effects) is standard for most switches, but is contraindicated when switching to or from an MAOI. A direct switch may be an appropriate approach when switching to another agent in the same or similar class (eg, when switching between two SSRIs), when the antidepressant to be discontinued has been used for <1 week, or when the discontinuation is for adverse effects. When choosing the switch strategy, consider the risk of discontinuation symptoms, potential for drug interactions, other antidepressant properties (eg, half-life, adverse effects, pharmacodynamics), and the degree of symptom control desired (Hirsch 2019b; Ogle 2013; WFSBP [Bauer 2013]).
Switching to or from an MAOI:
Allow 14 days to elapse between discontinuing an MAOI and initiation of paroxetine.
Allow 14 days to elapse between discontinuing paroxetine and initiation of an MAOI.
Dosing: Geriatric
Major depressive disorder (unipolar), obsessive-compulsive disorder, panic disorder, social anxiety disorder:
Immediate release: Oral: Initial: 10 mg/day; may increase dose based on response and tolerability in increments of 10 mg/day at intervals ≥1 week to a maximum of 40 mg/day.
Extended release: Oral: Initial: 12.5 mg/day; may increase dose based on response and tolerability in increments of 12.5 mg/day at intervals ≥1 week to a maximum of 37.5 mg/day (social anxiety disorder) or 50 mg/day (major depressive disorder, panic disorder).
Note: An adequate trial for assessment of effect in obsessive-compulsive disorder is considered to be ≥6 weeks at the maximum tolerated dose (Issari 2016).
Dosing conversions: Refer to adult dosing.
Discontinuation of therapy: Refer to adult dosing.
Switching antidepressants: Refer to adult dosing.
Dosing: Pediatric
Note: Immediate-release paroxetine is available in two salts, hydrochloride (eg, Paxil) and mesylate (eg, Brisdelle, Pexeva); use extra precaution to ensure product selection. Paroxetine is available as immediate-release and extended-release formulations; both formulations are dosed once daily but are not interchangeable on a mg to mg basis; based on adult bioavailability data, immediate-release 10 mg is equivalent to extended-release 12.5 mg (DeVane 2003).
Obsessive-compulsive disorder (OCD): Limited data available: Children and Adolescents 7 to 17 years: Oral: Immediate release (hydrochloride salt): Initial: 10 mg once daily; titrate every 7 to 14 days in 10 mg/day increments; maximum daily dose: 60 mg/day. Dosing based on two trials. The first was a 12-week open-label trial of paroxetine in 20 outpatients 8 to 17 years of age that demonstrated the potential clinical usefulness in pediatric OCD (Rosenberg 1999). The second trial demonstrated efficacy of paroxetine in a 10-week, randomized, double-blind, placebo-controlled trial conducted in 207 pediatric patients (aged 7 to 17 years) with OCD; the overall mean dose was 20.3 mg/day for children and 26.8 mg/day for adolescents (Geller 2004).
Social anxiety disorder: Limited data available: Children and Adolescents 8 to 17 years: Oral: Immediate release (hydrochloride salt): Initial: 10 mg once daily; titrate at intervals of at least 7 days in 10 mg/day increments; maximum daily dose: 50 mg/day. Dosing based on a 16-week multicenter, randomized, double-blind, placebo-controlled trial that reported the efficacy of paroxetine in pediatric patients (aged 8 to 17 years) with social anxiety disorder; 163 patients were randomized to receive paroxetine; the overall mean dose was 21.7 mg/day for children and 26.1 mg/day for adolescents (Wagner 2004).
Discontinuation of OCD therapy: Consider planning discontinuation of therapy during lower-stress times, recognizing non-illness-related factors could cause stress or anxiety and be misattributed to OCD treatment discontinuation (Hathaway 2018). To discontinue therapy, gradually taper the dose to minimize the incidence of discontinuation syndromes (withdrawal) and allow for the detection of reemerging disease state symptoms (eg, relapse). Evidence supporting ideal taper rates after illness remission is sparse, particularly in pediatric patients; however, a general consensus is to taper over several weeks to months and to resume the previous OCD therapy if symptoms worsen; a plan for continued psychotherapy during serotonergic medication discontinuation is recommended (Boisseau 2018; Fenske 2015). A unified taper protocol has been reported in adults with OCD in which serotonin reuptake inhibitor monotherapy was tapered over 12 weeks with biweekly psychiatrist visits (Boisseau 2018). For the treatment of depression, experts suggest tapering therapy over at least several weeks with consideration to the half-life of the antidepressant; agents with a shorter half-life may need to be tapered more conservatively and if intolerable discontinuation symptoms occur following a dose reduction, consider resuming the previously prescribed dose and/or decrease dose at a more gradual rate; similar principles may also be applicable to OCD therapy discontinuation (APA 2010; Bauer 2002; Fenske 2009; Haddad 2001; NCCMH 2010; Schatzberg 2006; Shelton 2001; Warner 2006).
Monoamine oxidase (MAO) inhibitor recommendations:
Switching to or from an MAO inhibitor intended to treat psychiatric disorders:
Allow 14 days to elapse between discontinuing an MAO inhibitor intended to treat psychiatric disorders and initiation of paroxetine.
Allow 14 days to elapse between discontinuing paroxetine and initiation of an MAO inhibitor intended to treat psychiatric disorders.
Administration
Oral: May be administered without regard to meals. Administer preferably in the morning; when used for vasomotor symptoms of menopause, administer at bedtime. Do not crush, break, or chew ER or IR film-coated tablets.
Storage
Capsules: Store between 20°C and 25°C (68°F and 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F). Protect from light and humidity.
Tablets: Store between 20°C and 25°C (68°F and 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F).
Suspension: Store at or below 25°C (77°F).
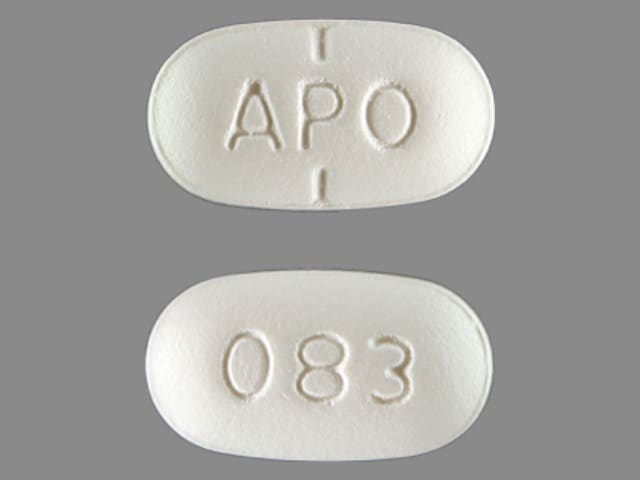
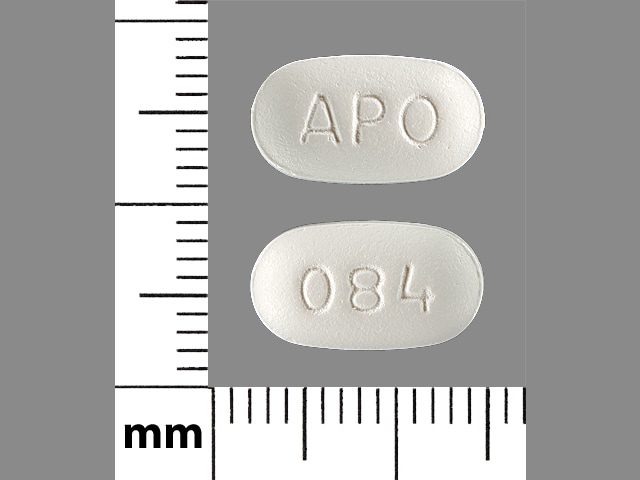
PARoxetine Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ajmaline: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Ajmaline. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Management: Patients receiving selective serotonin reuptake inhibitors should be advised to avoid alcohol. Monitor for increased psychomotor impairment in patients who consume alcohol during treatment with selective serotonin reuptake inhibitors. Consider therapy modification
Almotriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Alosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Amphetamines: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors). This could result in serotonin syndrome. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may increase the serum concentration of Amphetamines. Management: Monitor for increased amphetamine toxicities, including signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability) when these agents are combined. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Antiemetics (5HT3 Antagonists): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Alosetron; Ondansetron; Ramosetron. Monitor therapy
Antipsychotic Agents: Serotonergic Agents (High Risk) may enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, serotonergic agents may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotic Agents may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Monitor therapy
Apixaban: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Monitor therapy
Aprepitant: PARoxetine may decrease the serum concentration of Aprepitant. Aprepitant may decrease the serum concentration of PARoxetine. Monitor therapy
ARIPiprazole: PARoxetine may enhance the adverse/toxic effect of ARIPiprazole. Specifically, the risk of neuroleptic malignant syndrome may be increased. ARIPiprazole may enhance the serotonergic effect of PARoxetine. This could result in serotonin syndrome. PARoxetine may increase the serum concentration of ARIPiprazole. Management: Aripiprazole dose adjustment is recommended, except when used adjunctively for depression. Consult full interaction monograph or aripiprazole prescribing information for complete details. Consider therapy modification
ARIPiprazole Lauroxil: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of ARIPiprazole Lauroxil. Management: Please refer to the full interaction monograph for details concerning the recommended dose adjustments. Consider therapy modification
Asenapine: May increase the serum concentration of PARoxetine. Management: Decrease the paroxetine dose by half when used concomitantly with asenapine. Monitor patients receiving this combination closely for signs and symptoms of increased paroxetine toxicity. Consider therapy modification
Aspirin: Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Aspirin. Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
AtoMOXetine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of AtoMOXetine. Management: Initiate atomoxetine at a reduced dose (adult doses -- patients up to 70kg: 0.5mg/kg/day; patients 70kg or more: 40mg/day) in patients receiving a strong CYP2D6 inhibitor. Consider therapy modification
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Benzhydrocodone: CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Benzhydrocodone. Monitor therapy
Beta-Blockers: Selective Serotonin Reuptake Inhibitors may increase the serum concentration of Beta-Blockers. Exceptions: Acebutolol; Atenolol; Betaxolol (Ophthalmic); Betaxolol (Systemic); Bisoprolol; Carteolol (Ophthalmic); Esmolol; Labetalol; Levobunolol; Metipranolol; Nadolol; Sotalol. Monitor therapy
Blood Glucose Lowering Agents: Selective Serotonin Reuptake Inhibitors may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Brexanolone: Selective Serotonin Reuptake Inhibitors may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brexpiprazole: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Brexpiprazole. Management: Reduce brexpiprazole dose to 50% of usual with a strong CYP2D6 inhibitor, reduce to 25% of usual if used with both a strong CYP2D6 inhibitor and a CYP3A4 inhibitor; these recommendations do not apply if treating major depressive disorder. Consider therapy modification
Bromopride: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Avoid combination
BuPROPion: May enhance the adverse/toxic effect of PARoxetine. Specifically, the risk for seizures and serotonin syndrome may be increased. Monitor therapy
BusPIRone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Cimetidine: May increase the serum concentration of PARoxetine. Monitor therapy
Citalopram: May enhance the antiplatelet effect of Selective Serotonin Reuptake Inhibitors. Citalopram may enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, mental status changes) when these agents are combined. In addition, monitor for signs and symptoms of bleeding. Monitor therapy
Clarithromycin: May enhance the adverse/toxic effect of PARoxetine. Clarithromycin may enhance the QTc-prolonging effect of PARoxetine. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CloZAPine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of CloZAPine. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Codeine: CYP2D6 Inhibitors (Strong) may diminish the therapeutic effect of Codeine. These CYP2D6 inhibitors may prevent the metabolic conversion of codeine to its active metabolite morphine. Consider therapy modification
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Cyclobenzaprine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
CYP2D6 Substrates (High risk with Inhibitors): CYP2D6 Inhibitors (Strong) may decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Exceptions: Ajmaline; Dapoxetine; Indoramin; Metoprolol; Tamoxifen; Timolol (Ophthalmic); Tropisetron. Consider therapy modification
Cyproheptadine: May diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Dabigatran Etexilate: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Dabigatran Etexilate. Agents with Antiplatelet Properties may increase the serum concentration of Dabigatran Etexilate. This mechanism applies specifically to clopidogrel. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Monitor therapy
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Dapoxetine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Do not use serotonergic agents (high risk) with dapoxetine or within 7 days of serotonergic agent discontinuation. Do not use dapoxetine within 14 days of monoamine oxidase inhibitor use. Dapoxetine labeling lists this combination as contraindicated. Avoid combination
Darunavir: May decrease the serum concentration of PARoxetine. Monitor therapy
Dasatinib: May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Desmopressin: Selective Serotonin Reuptake Inhibitors may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Deutetrabenazine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Deutetrabenazine. Management: The total daily dose of deutetrabenazine should not exceed 36 mg, and the maximum single dose of deutetrabenazine should not exceed 18 mg with concurrent use of a strong CYP2D6 inhibitor. Consider therapy modification
Dexmethylphenidate-Methylphenidate: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Dextromethorphan: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors). This could result in serotonin syndrome. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may increase the serum concentration of Dextromethorphan. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes). Consider therapy modification
DOXOrubicin (Conventional): CYP2D6 Inhibitors (Strong) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to strong CYP2D6 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
DULoxetine: May enhance the antiplatelet effect of Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors). DULoxetine may enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors). This could result in serotonin syndrome. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may increase the serum concentration of DULoxetine. Management: Monitor for increased duloxetine effects/toxicities and signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperthermia, tremor, mental status changes) when these agents are combined. In addition, monitor for signs and symptoms of bleeding. Monitor therapy
Edoxaban: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Monitor therapy
Eletriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Eliglustat: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Eliglustat. Management: Reduce the eliglustat dose to 84 mg daily. Avoid use of eliglustat in combination with a strong CYP2D6 inhibitor and a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Ergot Derivatives: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Nicergoline. Monitor therapy
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Fesoterodine: CYP2D6 Inhibitors may increase serum concentrations of the active metabolite(s) of Fesoterodine. Monitor therapy
FLUoxetine: May enhance the antiplatelet effect of PARoxetine. FLUoxetine may enhance the serotonergic effect of PARoxetine. This could result in serotonin syndrome. FLUoxetine may increase the serum concentration of PARoxetine. PARoxetine may increase the serum concentration of FLUoxetine. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, mental status changes), bleeding, and increased SSRI toxicities when these agents are combined. Monitor therapy
Fosamprenavir: May decrease the serum concentration of PARoxetine. The active metabolite amprenavir is likely responsible for this effect. Monitor therapy
Fosaprepitant: PARoxetine may decrease serum concentrations of the active metabolite(s) of Fosaprepitant. Fosaprepitant may decrease the serum concentration of PARoxetine. Monitor therapy
Galantamine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Galantamine. Monitor therapy
Gilteritinib: May diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Management: Avoid use of this combination if possible. If the combination cannot be avoided, monitor closely for evidence of reduced response to the selective serotonin reuptake inhibitor. Consider therapy modification
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Heparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or agents with antiplatelet properties if coadministration is required. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
HYDROcodone: CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of HYDROcodone. Specifically, concentrations of hydromorphone may be decreased. Monitor therapy
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Iloperidone: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Iloperidone. Specifically, concentrations of the metabolite P88 may be increased. CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Iloperidone. Specifically, concentrations of the metabolite P95 may be decreased. CYP2D6 Inhibitors (Strong) may increase the serum concentration of Iloperidone. Management: Reduce iloperidone dose by half when administered with a strong CYP2D6 inhibitor. Consider therapy modification
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Indoramin: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Indoramin. Monitor therapy
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Ioflupane I 123: Selective Serotonin Reuptake Inhibitors may diminish the diagnostic effect of Ioflupane I 123. Monitor therapy
Lasmiditan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Linezolid: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Avoid combination
Lofexidine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Lofexidine. Monitor therapy
Lorcaserin: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Mequitazine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Mequitazine. Avoid combination
Metaxalone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Methylene Blue: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Methylene Blue. This could result in serotonin syndrome. Avoid combination
Metoclopramide: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Management: Seek alternatives to this combination when possible. Monitor patients receiving metoclopramide with selective serotonin reuptake inhibitors for signs of extrapyramidal symptoms, neuroleptic malignant syndrome, and serotonin syndrome. Consider therapy modification
Metoclopramide: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Metoclopramide. Management: Reduce metoclopramide dose to 5 mg 4 times daily (30 minutes before each meal and at bedtime) and limit the maximum daily dose to 20 mg if combined with strong CYP2D6 inhibitors. Consider therapy modification
Metoprolol: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Metoprolol. Monitor therapy
MetyroSINE: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Monoamine Oxidase Inhibitors (Antidepressant): Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Monoamine Oxidase Inhibitors (Antidepressant). This could result in serotonin syndrome. Avoid combination
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Nebivolol: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Nebivolol. Monitor therapy
Nefazodone: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Nicergoline: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Nicergoline. Specifically, concentrations of the MMDL metabolite may be increased. CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Nicergoline. Specifically, concentrations of the MDL metabolite may be decreased. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective) may diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (Nonselective): Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Management: Consider alternatives to NSAIDs. Monitor for evidence of bleeding and diminished antidepressant effects. It is unclear whether COX-2-selective NSAIDs reduce risk. Exceptions: Diclofenac (Topical); Ibuprofen (Topical); Piroxicam (Topical). Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (Topical): May enhance the antiplatelet effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Ondansetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Opioid Agonists: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: FentaNYL; Meperidine; TraMADol. Monitor therapy
Oxitriptan: Serotonergic Agents (High Risk) may enhance the serotonergic effect of Oxitriptan. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Perhexiline: CYP2D6 Inhibitors may increase the serum concentration of Perhexiline. Management: Consider alternatives to this combination if possible. If combined, monitor for increased perhexiline serum concentrations and toxicities (eg, hypoglycemia, neuropathy, liver dysfunction). Perhexiline dose reductions will likely be required. Consider therapy modification
Pimozide: Selective Serotonin Reuptake Inhibitors may enhance the adverse/toxic effect of Pimozide. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs as appropriate. Avoid combination
Pimozide: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Pimozide. Avoid combination
Pitolisant: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Pitolisant. Management: Reduce the pitolisant dose by 50% if a strong CYP2D6 inhibitor is initiated. For patients receiving strong CYP2D6 inhibitors, initiate pitolisant at 8.9 mg once daily and increase after 7 days to a maximum of 17.8 mg once daily. Consider therapy modification
Pravastatin: May enhance the adverse/toxic effect of PARoxetine. Specifically, blood glucose elevations may occur with the combination. Monitor therapy
Primaquine: CYP2D6 Inhibitors (Strong) may diminish the therapeutic effect of Primaquine. Management: Monitor for signs and symptoms of possible treatment failure with primaquine in patients who are taking strong CYP2D6 inhibitors. If efficacy of primaquine is compromised, may consider adjusting therapies. Consider therapy modification
Propafenone: PARoxetine may increase the serum concentration of Propafenone. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ramosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Rasagiline: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Rasagiline. This could result in serotonin syndrome. Avoid combination
Rivaroxaban: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Rivaroxaban. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Monitor therapy
Safinamide: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Use the lowest effective dose of SSRIs in patients treated with safinamide and monitor for signs and symptoms of serotonin syndrome/serotonin toxicity. Consider therapy modification
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the antiplatelet effect of other Selective Serotonin Reuptake Inhibitors. Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of other Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, mental status changes) when these agents are combined. In addition, monitor for signs and symptoms of bleeding. Exceptions: Citalopram; Dapoxetine; Vortioxetine. Monitor therapy
Selegiline: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Selegiline. This could result in serotonin syndrome. Avoid combination
Serotonergic Agents (High Risk, Miscellaneous): May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Serotonergic Non-Opioid CNS Depressants: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Serotonergic Non-Opioid CNS Depressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Serotonergic Opioids (High Risk): May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) if these agents are combined. Exceptions: TraMADol. Monitor therapy
Serotonin 5-HT1D Receptor Agonists (Triptans): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Almotriptan; Eletriptan. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Serotonin/Norepinephrine Reuptake Inhibitors. Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Serotonin/Norepinephrine Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, mental status changes) when these agents are combined. In addition, monitor for signs and symptoms of bleeding. Exceptions: DULoxetine. Monitor therapy
St John's Wort: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. St John's Wort may decrease the serum concentration of Serotonergic Agents (High Risk). Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Syrian Rue: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Tamoxifen: CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Tamoxifen. Specifically, strong CYP2D6 inhibitors may decrease the metabolic formation of highly potent active metabolites. Avoid combination
Tamsulosin: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Tamsulosin. Monitor therapy
Tetrabenazine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Tetrabenazine. Specifically, concentrations of the active alpha- and beta-dihydrotetrabenazine metabolites may be increased. Management: Tetrabenazine adult dose should be reduced by 50% when starting a strong CYP2D6 inhibitor. Maximum tetrabenazine adult dose is 50 mg/day when used with a strong CYP2D6 inhibitor. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Selective Serotonin Reuptake Inhibitors may enhance the hyponatremic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thioridazine: CYP2D6 Inhibitors may increase the serum concentration of Thioridazine. Avoid combination
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Thyroid Products: Selective Serotonin Reuptake Inhibitors may diminish the therapeutic effect of Thyroid Products. Thyroid product dose requirements may be increased. Monitor therapy
Timolol (Ophthalmic): CYP2D6 Inhibitors (Strong) may increase the serum concentration of Timolol (Ophthalmic). Monitor therapy
TraMADol: Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may enhance the adverse/toxic effect of TraMADol. Specifically, the risk for serotonin syndrome/serotonin toxicity and seizures may be increased. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may diminish the therapeutic effect of TraMADol. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes), seizures, and decreased tramadol efficacy when these agents are combined. Monitor therapy
Tricyclic Antidepressants: PARoxetine may enhance the serotonergic effect of Tricyclic Antidepressants. PARoxetine may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA concentrations/effects if these agents are combined. Consider therapy modification
Tropisetron: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Tropisetron. Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Valbenazine: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Valbenazine. Monitor therapy
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Selective Serotonin Reuptake Inhibitors may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Vortioxetine: Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may enhance the antiplatelet effect of Vortioxetine. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may enhance the serotonergic effect of Vortioxetine. This could result in serotonin syndrome. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may increase the serum concentration of Vortioxetine. Management: Consider alternatives to this drug combination. If combined, reduce the vortioxetine dose by half and monitor for signs and symptoms of bleeding and serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, autonomic instability). Consider therapy modification
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Adverse Reactions
Frequency varies by dose and indication. Adverse reactions reported as a composite of all indications.
>10%:
Central nervous system: Drowsiness (15% to 24%), insomnia (11% to 24%), headache (6% to 18%), dizziness (6% to 14%)
Dermatologic: Diaphoresis (5% to 14%)
Endocrine & metabolic: Decreased libido (3% to 15%)
Gastrointestinal: Nausea (19% to 26%), xerostomia (9% to 18%), constipation (5% to 16%), diarrhea (9% to 12%)
Genitourinary: Ejaculatory disorder (13% to 28%)
Neuromuscular & skeletal: Weakness (12% to 22%), tremor (4% to 11%)
1% to 10%:
Cardiovascular: Vasodilation (2% to 4%), chest pain (3%), palpitations (2% to 3%), hypertension (≥1%), tachycardia (≥1%)
Central nervous system: Nervousness (4% to 9%), anxiety (5%), fatigue (5%), agitation (3% to 5%), paresthesia (4%), abnormal dreams (3% to 4%), lack of concentration (3% to 4%), yawning (2% to 4%), depersonalization (≤3%), myoclonus (2% to 3%), amnesia (2%), chills (2%), emotional lability (≥1%), vertigo (≥1%), confusion (1%), myasthenia (1%)
Dermatologic: Skin rash (2% to 3%), pruritus (≥1%)
Endocrine & metabolic: Weight gain (≥1%)
Gastrointestinal: Decreased appetite (5% to 9%), dyspepsia (2% to 5%), flatulence (4%), abdominal pain (4%), nausea and vomiting (4%), increased appetite (2% to 4%), vomiting (2% to 3%), dysgeusia (2%)
Genitourinary: Male genital disease (10%), female genital tract disease (2% to 9%), impotence (2% to 9%), orgasm disturbance (2% to 9%), dysmenorrhea (5%), urinary frequency (2% to 3%), urinary tract infection (2%)
Infection: Infection (5% to 6%)
Neuromuscular & skeletal: Myalgia (2% to 4%), back pain (3%), myopathy (2%), arthralgia (≥1%)
Ophthalmic: Blurred vision (4%), visual disturbance (2% to 4%)
Otic: Tinnitus (≥1%)
Respiratory: Dyspnea (≤7%), pharyngitis (4%), sinusitis (≤4%), rhinitis (3%)
<1%, postmarketing, and/or case reports: Abnormal erythrocytes, abnormal hepatic function tests, acute renal failure, adrenergic syndrome, aggressive behavior, agranulocytosis, akathisia, akinesia, anaphylactoid reaction, anaphylaxis, anemia (various), angina pectoris, angioedema, angle-closure glaucoma, aphasia, aphthous stomatitis, aplastic anemia, asthma, atrial fibrillation, behavioral problems (various), bloody diarrhea, bone marrow aplasia, bradycardia, bronchitis, bulimia nervosa, bundle branch block, cardiac failure, cataract, cellulitis, cerebral ischemia, cerebrovascular accident, change in platelet count, cholelithiasis, colitis, deafness, dehydration, delirium, depression, diabetes mellitus, disorientation, drug dependence, dyskinesia, dysphagia, dyspnea, dystonia, ecchymoses, eclampsia, emphysema, erythema, esophageal achalasia, exfoliative dermatitis, extrapyramidal reaction, fecal impaction, fungal dermatitis, gastroenteritis, goiter, Guillain-Barre syndrome, hallucination, hematemesis, hematologic disease, hematoma, hemoptysis, hemorrhage (eye, gingival, rectal, retinal, vaginal), hemorrhagic pancreatitis, hepatic failure, hepatic necrosis, hepatitis, hepatotoxicity, homicidal ideation, hyperbilirubinemia, hypercholesteremia, hypergammaglobulinemia, hyperglycemia, hyperhidrosis, hypersensitivity reaction, hyperthyroidism, hypoglycemia, hyponatremia, hypotension, hypothyroidism, immune thrombocytopenia, increased blood urea nitrogen, increased creatine phosphokinase, increased lactate dehydrogenase, increased serum alkaline phosphatase, intestinal obstruction, ischemic heart disease, jaundice, ketosis, low cardiac output, lymphadenopathy, malaise, meningitis, migraine, mydriasis, myelitis, myocardial infarction, neuroleptic malignant syndrome (Stevens, 2008), neuropathy, nodal arrhythmia, osteoarthritis, osteoporosis, pancreatitis, pancytopenia, peptic ulcer, peritonitis, phlebitis, pneumonia, prolonged bleeding time, pulmonary edema, pulmonary embolism, pulmonary fibrosis, pulmonary hypertension, restlessness, seizure, sepsis, serotonin syndrome, status epilepticus, Stevens-Johnson syndrome, suicidal ideation, suicidal tendencies, syncope, tetany, thrombophlebitis, thrombosis, tongue edema, torsades de pointes, toxic epidermal necrolysis, uncontrolled diabetes mellitus, vasculitis, ventricular arrhythmia, ventricular fibrillation, ventricular tachycardia, withdrawal syndrome (including increased dreaming/nightmares, muscle cramps/spasms/twitching, headache, nervousness/anxiety, fatigue/tiredness, restless feeling in legs, and trouble sleeping/insomnia)
Warnings/Precautions
Major psychiatric warnings:
- Suicidal thoughts/behavior: [US Boxed Warning]: Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric and young adult patients in short-term studies. Closely monitor all antidepressant-treated patients for clinical worsening and for emergence of suicidal thoughts and behaviors. Short-term studies did not show an increased risk in patients >24 years of age and showed a decreased risk in patients ≥65 years of age. Closely monitor patients for clinical worsening, suicidality, or unusual changes in behavior, particularly during the initial 1 to 2 months of therapy or during periods of dosage adjustments (increases or decreases); the patient's family or caregiver should be instructed to closely observe the patient and communicate condition with health care provider. A medication guide concerning the use of antidepressants should be dispensed with each prescription. Paroxetine is not FDA approved for use in children.
- The possibility of a suicide attempt is inherent in major depression and may persist until remission occurs. Worsening depression and severe abrupt suicidality that are not part of the presenting symptoms may require discontinuation or modification of drug therapy. Use caution in high-risk patients during initiation of therapy.
- Prescriptions should be written for the smallest quantity consistent with good patient care. The patient's family or caregiver should be alerted to monitor patients for the emergence of suicidality and associated behaviors such as anxiety, agitation, panic attacks, insomnia, irritability, hostility, impulsivity, akathisia, hypomania, and mania; patients should be instructed to notify their healthcare provider if any of these symptoms or worsening depression or psychosis occur.
Concerns related to adverse effects:
- Akathisia: Inability to remain still due to feelings of agitation or restlessness has been observed with paroxetine and other selective serotonin reuptake inhibitors (SSRIs). Usually occurs within the first few weeks of therapy.
- Anticholinergic effects: Has low potential for sedation and anticholinergic effects relative to cyclic antidepressants; however, among the SSRI class these effects are relatively higher.
- Bleeding risk: May impair platelet aggregation resulting in increased risk of bleeding events, particularly if used concomitantly with aspirin, nonsteroidal anti-inflammatory drugs, warfarin or other anticoagulants. Bleeding related to SSRI use has been reported to range from relatively minor bruising and epistaxis to life-threatening hemorrhage.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Fractures: Bone fractures have been associated with antidepressant treatment. Consider the possibility of a fragility fracture if an antidepressant-treated patient presents with unexplained bone pain, point tenderness, swelling, or bruising (Rabenda 2013; Rizzoli, 2012).
- Ocular effects: May cause mild pupillary dilation, which can lead to an episode of narrow-angle glaucoma in susceptible individuals. Consider evaluating patients who have not had an iridectomy for narrow-angle glaucoma risk factors.
- Serotonin syndrome: Potentially life-threatening serotonin syndrome (SS) has occurred with serotonergic agents (eg, SSRIs, serotonin-norepinephrine reuptake inhibitors [SNRIs]), particularly when used in combination with other serotonergic agents (eg, triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, buspirone, St John's wort, tryptophan) or agents that impair metabolism of serotonin (eg, monoamine oxidase [MAO] inhibitors intended to treat psychiatric disorders, other MAO inhibitors [ie, linezolid and intravenous methylene blue]). Monitor patients closely for signs of SS such as mental status changes (eg, agitation, hallucinations, delirium, coma); autonomic instability (eg, tachycardia, labile blood pressure, diaphoresis); neuromuscular changes (eg, tremor, rigidity, myoclonus); GI symptoms (eg, nausea, vomiting, diarrhea); and/or seizures. Discontinue treatment (and any concomitant serotonergic agent) immediately if signs/symptoms arise.
- Sexual dysfunction: May cause or exacerbate sexual dysfunction.
- Syndrome of inappropriate antidiuretic hormone secretion and hyponatremia: SSRIs and SNRIs have been associated with the development of syndrome of inappropriate antidiuretic hormone secretion (SIADH); hyponatremia has been reported rarely (including severe cases with serum sodium <110 mmol/L), predominately in the elderly. Volume depletion and/or concurrent use of diuretics likely increases risk.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with cardiovascular disease; paroxetine has not been systemically evaluated in patients with a recent history of myocardial infarction or unstable heart disease.
- Hepatic impairment: Use with caution in patients with hepatic impairment; clearance is decreased and plasma concentrations are increased; a lower dosage may be needed.
- Mania/hypomania: May worsen psychosis in some patients or precipitate a shift to mania or hypomania in patients with bipolar disorder. Monotherapy in patients with bipolar disorder should be avoided. Patients presenting with depressive symptoms should be screened for bipolar disorder. Paroxetine is not FDA approved for the treatment of bipolar depression.
- Renal impairment: Use with caution in patients with renal impairment; clearance is decreased and plasma concentrations are increased; a lower dosage may be needed.
- Seizure disorder: Use with caution in patients with a previous seizure disorder or condition predisposing to seizures such as brain damage or alcoholism.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Brisdelle: Brisdelle contains a lower dose than what is required for the treatment of psychiatric conditions. Patients who require paroxetine for the treatment of psychiatric conditions should discontinue Brisdelle and begin treatment with a paroxetine-containing medication which provides an adequate dosage.
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley, 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Other warnings/precautions:
- Discontinuation syndrome: Abrupt discontinuation or interruption of antidepressant therapy has been associated with a discontinuation syndrome. Symptoms arising may vary with antidepressant however commonly include nausea, vomiting, diarrhea, headaches, lightheadedness, dizziness, diminished appetite, sweating, chills, tremors, paresthesias, fatigue, somnolence, and sleep disturbances (eg, vivid dreams, insomnia). Less common symptoms include electric shock-like sensations, cardiac arrhythmias (more common with tricyclic antidepressants), myalgias, parkinsonism, arthralgias, and balance difficulties. Psychological symptoms may also emerge such as agitation, anxiety, akathisia, panic attacks, irritability, aggressiveness, worsening of mood, dysphoria, mood lability, hyperactivity, mania/hypomania, depersonalization, decreased concentration, slowed thinking, confusion, and memory or concentration difficulties. Greater risks for developing a discontinuation syndrome have been associated with antidepressants with shorter half-lives, longer durations of treatment, and abrupt discontinuation. For antidepressants of short or intermediate half-lives, symptoms may emerge within 2 to 5 days after treatment discontinuation and last 7 to 14 days (APA 2010; Fava 2006; Haddad 2001; Shelton 2001; Warner 2006).
- Electroconvulsive therapy: May increase the risks associated with electroconvulsive therapy; consider discontinuing, when possible, prior to ECT treatment.
Monitoring Parameters
Liver and renal function tests (baseline; as clinically indicated); serum sodium in at-risk populations (as clinically indicated); CBC (as clinically indicated); evaluate for suicidal ideation (baseline and with dose changes).
Pregnancy
Pregnancy Risk Factor
D/X (product specific)
Pregnancy Considerations
Paroxetine crosses the placenta (Hendrick 2003). An increased risk of teratogenic effects, including cardiovascular defects, may be associated with maternal use of paroxetine or other SSRIs; however, available information is conflicting. Nonteratogenic effects in the newborn following SSRI/SNRI exposure late in the third trimester include respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypo- or hypertonia, hyper-reflexia, jitteriness, irritability, constant crying, and tremor. Symptoms may be due to the toxicity of the SSRIs/SNRIs or a discontinuation syndrome and may be consistent with serotonin syndrome associated with SSRI treatment. Persistent pulmonary hypertension of the newborn (PPHN) has also been reported with SSRI exposure. The long-term effects of in utero SSRI exposure on infant development and behavior are not known.
Due to pregnancy-induced physiologic changes, some pharmacokinetic parameters of paroxetine may be altered. The maternal CYP2D6 genotype also influences paroxetine plasma concentrations during pregnancy (Hostetter 2000; Ververs 2009).
The manufacturer suggests discontinuing paroxetine or switching to another antidepressant unless the benefits of therapy justify continuing treatment during pregnancy; consider other treatment options for women who are planning to become pregnant. The ACOG recommends that therapy with SSRIs or SNRIs during pregnancy be individualized; treatment of depression during pregnancy should incorporate the clinical expertise of the mental health clinician, obstetrician, primary health care provider, and pediatrician. The ACOG also recommends that therapy with paroxetine be avoided during pregnancy if possible and that fetuses exposed in early pregnancy be assessed with a fetal echocardiography (ACOG 2008). Other guidelines note that treatment with paroxetine should not be initiated in pregnant women (Bauer 2013). According to the American Psychiatric Association (APA), the risks of medication treatment should be weighed against other treatment options and untreated depression. The use of paroxetine is not recommended as first line therapy during pregnancy. For women who discontinue antidepressant medications during pregnancy and who may be at high risk for postpartum depression, the medications can be restarted following delivery (APA 2010). Treatment algorithms have been developed by the ACOG and the APA for the management of depression in women prior to conception and during pregnancy (Yonkers 2009).
Menopausal vasomotor symptoms do not occur during pregnancy; therefore, the use of paroxetine for the treatment of menopausal vasomotor symptoms is contraindicated in pregnant women.
Pregnant women exposed to antidepressants during pregnancy are encouraged to enroll in the National Pregnancy Registry for Antidepressants (NPRAD). Women 18 to 45 years of age or their health care providers may contact the registry by calling 844-405-6185. Enrollment should be done as early in pregnancy as possible.
Patient Education
What is this drug used for?
- It is used to treat low mood (depression).
- It is used to treat obsessive-compulsive problems.
- It is used to treat panic attacks.
- It is used to treat anxiety.
- It is used to treat post-traumatic stress.
- It is used to treat mood problems caused by monthly periods.
- It is used to treat hot flashes caused by menopause.
- It may be given for other reasons.
Frequently reported side effects of this drug
- Fatigue
- Anxiety
- Headache
- Nausea
- Vomiting
- Constipation
- Abdominal pain
- Passing gas
- Back pain
- Anxiety
- Diarrhea
- Passing gas
- Dry mouth
- Back pain
- Trouble sleeping
- Loss of strength and energy
- Tremors
- Lack of appetite
- Yawning
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, severe diarrhea
- Low sodium like headache, trouble focusing, trouble with memory, confusion, weakness, seizures, or change in balance
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
- Seizures
- Restlessness
- Vision changes
- Eye pain
- Severe eye irritation
- Confusion
- Change in balance
- Agitation
- Twitching
- Sweating
- Stiff muscles
- Abnormal heartbeat
- Sensing things that seem real but are not
- Severe dizziness
- Passing out
- Bone pain
- Excessive weight loss
- Burning or numbness feeling
- Sexual dysfunction
- Erection that lasts more than 4 hours
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.