Boxed Warning
Hepatotoxicity:
Severe and fatal hepatotoxicity has been observed in clinical trials. Monitor hepatic function and interrupt, reduce, or discontinue dosing as recommended.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Votrient: 200 mg
Pharmacology
Mechanism of Action
Tyrosine kinase (multikinase) inhibitor; limits tumor growth via inhibition of angiogenesis by inhibiting cell surface vascular endothelial growth factor receptors (VEGFR-1, VEGFR-2, VEGFR-3), platelet-derived growth factor receptors (PDGFR-alpha and -beta), fibroblast growth factor receptor (FGFR-1 and -3), cytokine receptor (cKIT), interleukin-2 receptor inducible T-cell kinase, lymphocyte-specific protein tyrosine kinase (Lck), and transmembrane glycoprotein receptor tyrosine kinase (c-Fms)
Pharmacokinetics/Pharmacodynamics
Metabolism
Hepatic; primarily via CYP3A4, minor metabolism via CYP1A2 and CYP2C8
Excretion
Feces (primarily); urine (<4%)
Time to Peak
Plasma: 2 to 4 hours
Half-Life Elimination
~31 hours
Protein Binding
>99%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Cmax and AUC were 43% and 29%, respectively, of that observed in patients with moderate hepatic impairment administered a 200 mg dose compared with patients with normal hepatic function who received an 800 mg dose.
Use: Labeled Indications
Renal cell carcinoma, advanced: Treatment of advanced renal cell carcinoma
Soft tissue sarcoma, advanced: Treatment of advanced soft tissue sarcoma (in patients who have received prior chemotherapy)
Limitations of use: The efficacy of pazopanib for the treatment of adipocytic soft tissue sarcoma or gastrointestinal stromal tumors (GIST) has not been demonstrated.
Use: Off Label
Desmoid tumors (progressive)b
Data from a multicenter, open-label, randomized phase 2 study support the use of pazopanib in the treatment of progressive desmoid tumors Toulmonde 2019.
Thyroid cancer (advanced, differentiated)b
Data from a phase II study supports the use of pazopanib in the treatment of advanced differentiated thyroid cancer Bible 2010, Bible 2014.
Contraindications
There are no contraindications listed in the manufacturer’s US labeling.
Canadian labeling: Hypersensitivity to pazopanib or any component of the formulation; use in pediatric patients <2 years of age (due to the antiangiogenic effects)
Dosage and Administration
Dosing: Adult
Desmoid tumors, progressive (off-label use): Oral: 800 mg once daily until disease progression or unacceptable toxicity for up to a maximum of 1 year (Toulmonde 2019).
Renal cell carcinoma, advanced: Oral: 800 mg once daily (Sternberg 2010).
Soft tissue sarcoma, advanced: Oral: 800 mg once daily (Van Der Graaf 2012).
Thyroid cancer, advanced differentiated (off-label use): Oral: 800 mg once daily until disease progression or unacceptable toxicity (Bible 2010; Bible 2014).
Missed doses: If a dose is missed, do not take if <12 hours until the next dose.
Concomitant CYP3A4 inhibitors/inducers:
CYP3A4 inhibitors: Avoid concomitant strong CYP3A4 inhibitors (may increase pazopanib concentrations). If pazopanib must be administered concomitantly with a potent enzyme inhibitor, reduce pazopanib to 400 mg once daily with careful monitoring; further dosage reductions may be needed if adverse events occur.
CYP3A4 inducers: Avoid concomitant strong CYP3A4 inducers (may decrease pazopanib concentrations); use of pazopanib is not recommended in situations where the chronic use of a strong CYP3A4 inducer is required.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Initial dosage reduction: Note: Prior to dose reduction, temporarily discontinue therapy if 24-hour urine protein ≥3 g or for other toxicities when clinically indicated.
RCC: Reduce to 400 mg once daily
STS: Reduce to 600 mg once daily
Further modification: RCC, STS: Adjust dose in 200 mg increments or decrements based on individual tolerance; maximum dose: 800 mg
Hypertension: Manage as appropriate with antihypertensive therapy and interrupt treatment or reduce dose as clinically warranted.
Hypertension (severe, persistent, and refractory to antihypertensives and dose reduction) or evidence of hypertensive crisis: Discontinue treatment.
Infection, serious: Consider treatment interruption or discontinuation.
Proteinuria (24-hour urine protein ≥3 g): Interrupt treatment and reduce the dose.
Proteinuria (recurrent 24-hour urine protein ≥3 g refractory to dose reduction): Discontinue treatment.
Pulmonary toxicity: Interstitial lung disease (ILD) or pneumonitis: Discontinue treatment.
Reversible posterior leukoencephalopathy syndrome (RPLS): Permanently discontinue.
Thrombotic microangiopathy (TMA): Permanently discontinue.
Wound dehiscence: Discontinue treatment.
Administration
Administer on an empty stomach, 1 hour before or 2 hours after a meal. Do not crush tablet (rate of absorption may be increased; may affect systemic exposure).
Dietary Considerations
Avoid grapefruit juice.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F).
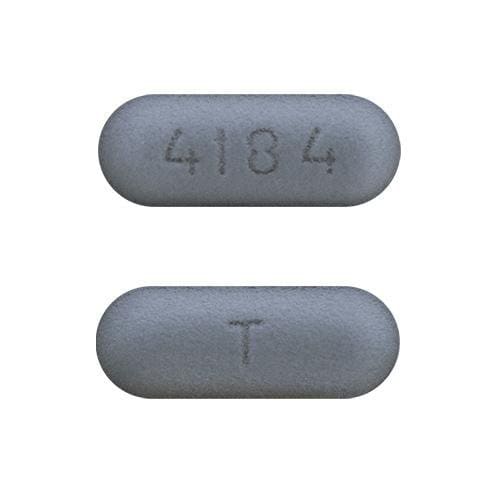
Pazopanib Images
Drug Interactions
Antacids: May decrease the serum concentration of PAZOPanib. Management: Avoid the use of antacids in combination with pazopanib whenever possible. Separate doses by several hours if antacid treatment is considered necessary. The impact of dose separation has not been investigated. Consider therapy modification
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
ARIPiprazole: CYP3A4 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCRP/ABCG2 Inhibitors: May increase the serum concentration of PAZOPanib. Avoid combination
Bisphosphonate Derivatives: Angiogenesis Inhibitors (Systemic) may enhance the adverse/toxic effect of Bisphosphonate Derivatives. Specifically, the risk for osteonecrosis of the jaw may be increased. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of PAZOPanib. Avoid combination
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of PAZOPanib. Management: Avoid concurrent use of pazopanib with strong inhibitors of CYP3A4 whenever possible. If it is not possible to avoid such a combination, reduce pazopanib adult dose to 400 mg. Further dose reductions may also be required. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dofetilide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Dofetilide. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Grapefruit Juice: May increase the serum concentration of PAZOPanib. Avoid combination
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Histamine H2 Receptor Antagonists: May decrease the serum concentration of PAZOPanib. Management: Avoid the use of histamine H2-antagonists in combination with pazopanib. Strategies to minimize the expected interaction between these agents (eg, dose separation) have not been investigated. Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Irinotecan Products: UGT1A1 Inhibitors may increase serum concentrations of the active metabolite(s) of Irinotecan Products. Specifically, concentrations of SN-38 may be increased. UGT1A1 Inhibitors may increase the serum concentration of Irinotecan Products. Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Lapatinib: May enhance the QTc-prolonging effect of PAZOPanib. Lapatinib may increase the serum concentration of PAZOPanib. Avoid combination
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lasmiditan: May increase the serum concentration of BCRP/ABCG2 Substrates. Avoid combination
Lemborexant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lemborexant. Management: The maximum recommended dosage of lemborexant is 5 mg, no more than once per night, when coadministered with weak CYP3A4 inhibitors. Consider therapy modification
Lomitapide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lomitapide. Management: Patients on lomitapide 5 mg/day may continue that dose. Patients taking lomitapide 10 mg/day or more should decrease the lomitapide dose by half. The lomitapide dose may then be titrated up to a max adult dose of 30 mg/day. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
NiMODipine: CYP3A4 Inhibitors (Weak) may increase the serum concentration of NiMODipine. Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of PAZOPanib. Avoid combination
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Pimozide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Pimozide. Avoid combination
Proton Pump Inhibitors: May decrease the serum concentration of PAZOPanib. Avoid combination
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Repaglinide: CYP2C8 Inhibitors (Weak) may increase the serum concentration of Repaglinide. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simvastatin: May enhance the adverse/toxic effect of PAZOPanib. Specifically, the risk for ALT/AST elevations may be increased. Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tafamidis: May increase the serum concentration of BCRP/ABCG2 Substrates. Monitor therapy
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Tolvaptan: May increase the serum concentration of BCRP/ABCG2 Substrates. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Triazolam: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Triazolam. Management: Consider triazolam dose reduction in patients receiving concomitant weak CYP3A4 inhibitors. Consider therapy modification
Ubrogepant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Ubrogepant. Management: In patients taking weak CYP3A4 inhibitors, the initial and second dose (if needed) of ubrogepant should be limited to 50 mg. Consider therapy modification
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Vinflunine: PAZOPanib may enhance the adverse/toxic effect of Vinflunine. Monitor therapy
Voxilaprevir: May increase the serum concentration of BCRP/ABCG2 Substrates. Avoid combination
Adverse Reactions
>10%:
Cardiovascular: Hypertension (40% to 42%; early in treatment), bradycardia (2% to 19%), peripheral edema (STS: 14%), cardiac insufficiency (11% to 13%)
Central nervous system: Fatigue (19%; STS: 65%), tumor pain (STS: 29%), headache (10%; STS: 23%), dizziness (11%)
Dermatologic: Hair discoloration (38% to 39%), exfoliative dermatitis (STS: 18%), alopecia (8% to 12%), dermatological disease (STS: 11%), hypopigmentation (STS, skin: 11%), palmar-plantar erythrodysesthesia (6% to 11%)
Endocrine & metabolic: Weight loss (9%, STS: 48%), increased serum glucose (41% to 45%), increased thyroid-stimulating hormone (TSH), decreased serum albumin (STS: 34%), decreased serum phosphate (34%), decreased serum sodium (31%), decreased serum magnesium (26%), decreased serum glucose (17%), increased serum potassium (STS: 16%)
Gastrointestinal: Diarrhea (52% to 59%), nausea (26%, STS: 56%), decreased appetite (STS: 40%), anorexia (22%), vomiting (21%, STS: 33%), dysgeusia (8%, STS: 28%), increased serum lipase (27%), gastrointestinal pain (STS: 23%), abdominal pain (11%), mucositis (STS: 12%), stomatitis (STS: 11%)
Hematologic & oncologic: Leukopenia (37% to 44%; STS, grade 3: 1%), lymphocytopenia (31%; grades 3/4: ≤4%; STS: 43%, grade 3: 10%), thrombocytopenia (32% to 36%; grades 3/4: ≤6%; grade 4: ≤1%), neutropenia (33% to 34%; grades 3/4 [in patients of East Asian descent]: 12%; grades 3/4 [in patients of non-East Asian descent]: ≤4%), hemorrhage (13% to 22%, including pulmonary, gastrointestinal, and genitourinary, grade 4: 1%, including intracranial, subarachnoid, and peritoneal)
Hepatic: Increased serum AST (51% to 53%), increased serum ALT (4% to 53%), increased serum bilirubin (29% to 36%), increased serum alkaline phosphatase (STS: 32%)
Neuromuscular & skeletal: Musculoskeletal pain (STS: 23%), myalgia (STS: 23%), weakness (14%)
Respiratory: Dyspnea (STS: 20%), cough (STS: 17%)
Miscellaneous: Tumor pain (29%)
1% to 10%:
Cardiovascular: Chest pain (5% to 10%; STS: grade 3: 2%), left ventricular systolic dysfunction (STS: 8%), venous thrombosis (STS: 5%), ischemia (≤2%), myocardial infarction (≤2%), prolonged Q-T interval on ECG (2%), facial edema (RCC: 1%), transient ischemic attacks (RCC: 1%)
Central nervous system: Insomnia (STS: 9%), voice disorder (4% to 8%), chills (STS: 5%)
Dermatologic: Skin rash (RCC: 8%), skin depigmentation (RCC: 3%), xeroderma (STS: 6%), nail disease (STS: 5%)
Endocrine & metabolic: Hypothyroidism (4% to 8%)
Gastrointestinal: Dyspepsia (5% to 7%), anal hemorrhage (STS: 2%), gastrointestinal fistula (≤1%), gastrointestinal perforation (≤1%)
Genitourinary: Proteinuria (1% to 9%), hematuria (RCC: 4%)
Hematologic & oncologic: Oral hemorrhage (STS: 3%), rectal hemorrhage (RCC: 1%)
Ophthalmic: Blurred vision (STS: 5%)
Respiratory: Epistaxis (2% to 8%), pneumothorax (≤3%), hemoptysis (RCC: 2%)
Frequency not defined:
Cardiovascular: Decreased left ventricular ejection fraction, hypertensive crisis
Central nervous system: Reversible posterior leukoencephalopathy syndrome
Hematologic & oncologic: Hemolytic-uremic syndrome, neutropenic infection, thrombotic thrombocytopenic purpura
Hepatic: Hepatotoxicity, severe hepatotoxicity
Infection: Serious infection
Neuromuscular & skeletal: Arthralgia (RCC), muscle spasm (RCC)
<1%, postmarketing, and/or case reports: Cardiac disease, cardiac failure, cerebral hemorrhage, cerebrovascular accident, interstitial pneumonitis, nephrotic syndrome, pancreatitis, polycythemia, retinal changes (tear), retinal detachment, torsades de pointes
Warnings/Precautions
Concerns related to adverse effects:
- Gastrointestinal perforation/fistula: Perforation and fistula (including fatal events) have been reported; monitor for symptoms of gastrointestinal perforation and fistula.
- Hand-foot skin reaction: Hand-foot skin reaction (HFSR) observed with tyrosine kinase inhibitors (TKIs) is distinct from hand-foot syndrome (palmar-plantar erythrodysesthesia) associated with traditional chemotherapy agents. HFSR due to TKIs is localized with defined hyperkeratotic lesions; symptoms include burning, dysesthesia, paresthesia, or tingling of the palms/soles, and generally occur within the first 2 to 4 weeks of treatment. Pressure and flexor areas may develop blisters (callus-like), dry/cracked skin, edema, erythema, desquamation, or hyperkeratosis. The incidence of HFSR is lower with pazopanib (compared to other tyrosine kinase inhibitors). Examine skin at baseline (remove calluses with pedicure prior to treatment) and with each visit; apply an emollient based moisturizer twice daily during treatment. If HFSR develops, consider changing moisturizer to a urea-based product; topical steroids may be utilized for the anti-inflammatory effect; avoid excessive friction or pressure to affected areas and avoid restrictive footwear. Temporary dose reduction or treatment interruption may be necessary (Appleby 2011).
- Heart failure: May cause new-onset or worsening of existing heart failure; baseline and periodic LVEF monitoring is recommended in patients at increased risk of heart failure (eg, prior anthracycline treatment). Concurrent hypertension may increase the risk for cardiac dysfunction. Monitor for signs/symptoms of heart failure.
- Hemorrhage: Hemorrhagic events (including fatal events) have been reported. In clinical studies, the most common events in renal cell carcinoma patients were hematuria, epistaxis, hemoptysis, and rectal hemorrhage. Epistaxis, mouth hemorrhage, and anal hemorrhage were most common in soft tissue sarcoma patients. Use is not recommended in patients with a history of hemoptysis, cerebral hemorrhage or clinically significant gastrointestinal hemorrhage within 6 months; these populations were excluded from clinical trials.
- Hepatotoxicity: [US Boxed Warning]: Severe and fatal hepatotoxicity (transaminase and bilirubin elevations) has been observed in studies. Monitor hepatic function and interrupt treatment, reduce dose, or discontinue as recommended. Liver function (ALT, AST, and bilirubin) tests should be monitored at baseline; at weeks 3, 5, 7, and 9; at months 3 and 4; and as clinically necessary, then periodically (after month 4). Transaminase elevations usually occur early in the treatment course. Use is not recommended in patients with preexisting severe hepatic impairment (bilirubin >3 times ULN with any ALT level); dosage reduction is recommended for preexisting moderate hepatic impairment (bilirubin >1.5 to 3 times ULN). Mild indirect (unconjugated) hyperbilirubinemia may occur in patients with Gilbert syndrome; for patients with known Gilbert syndrome (only a mild indirect bilirubin elevation) and ALT >3 times ULN, follow the dosage modification recommendations for isolated ALT elevations. Patients >65 years are at a higher risk for hepatotoxicity.
- Hypertension: May cause and/or worsen hypertension; hypertensive crisis has been observed. Blood pressure should be controlled prior to treatment initiation. Monitor frequently for hypertension; antihypertensive therapy should be used if needed. Hypertension usually occurs early in the treatment course. Dosage reduction may be necessary for hypertension that is persistent despite management with antihypertensive therapy; discontinue for hypertensive crisis, or for severe and persistent hypertension which is refractory to dose reduction and antihypertensive therapy.
- Infections: Serious, including fatal, infections have been reported; monitor for signs and symptoms of infection. Temporarily or permanently discontinue therapy for serious infections as clinically indicated.
- Ocular toxicity: Cases of retinal detachment or tear have been reported.
- Proteinuria: Has been reported with use. Obtain baseline and periodic urinalysis and 24-hour urine protein when clinically indicated. Dosage reduction may be necessary for significant proteinuria (≥3 g/24 hours); discontinue for recurrent proteinuria.
- Pulmonary toxicity: Interstitial lung disease (ILD)/pneumonitis has been reported with pazopanib; may be fatal. Monitor for pulmonary symptoms which could indicate ILD/pneumonitis; discontinue if ILD or pneumonitis develop.
- QTc prolongation: QTc prolongation, including torsade de pointes, has been observed; use caution in patients with a history of QTc prolongation, with medications known to prolong the QT interval, or with preexisting cardiac disease. Obtain baseline and periodic ECGs; correct electrolyte (potassium, calcium, and magnesium) abnormalities prior to and during treatment.
- Reversible posterior leukoencephalopathy syndrome (RPLS): Has been reported (rarely); may be fatal. Monitor for neurological changes or symptoms (blindness, confusion, headache, lethargy, seizure, visual or neurologic disturbances). Hypertension (mild to severe) may also be present. Permanently discontinue pazopanib in patients who develop RPLS.
- Thromboembolic events: Venous and arterial thromboembolism have been reported. DVT, pulmonary embolism, angina, transient ischemic attack, MI, and ischemic stroke were observed more frequently in the pazopanib group (versus placebo) in clinical trials. Fatalities were observed. Monitor for signs/symptoms of venous thrombotic events and pulmonary embolism. Use with caution in patients with a history of or an increased risk for these events. Use in patients with recent arteriothrombotic event (within 6 months) has not been studied and is not recommended.
- Thrombotic microangiopathy: Thrombotic microangiopathy (TMA), including thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS), has been observed in clinical studies. TMA has occurred with pazopanib monotherapy or when used in combination with bevacizumab or topotecan (off-label use); it typically occurs within 90 days of treatment initiation. Monitor for signs/symptoms and permanently discontinue in patients who develop TMA.
- Thyroid disorders: Hypothyroidism has been reported with use; monitor thyroid function tests.
- Wound healing complications: Vascular endothelial growth factor (VEGF) receptor inhibitors are associated with impaired wound healing. Discontinue treatment at least 7 days prior to scheduled surgery; treatment reinitiation should be guided by clinical judgment. Discontinue if wound dehiscence occurs.
Disease-related concerns:
- Renal impairment: Patients with mild-to-moderate renal impairment (CrCl ≥30 mL/minute) were included in trials. There are no pharmacokinetic data in patients with severe renal impairment undergoing dialysis (peritoneal and hemodialysis); however, renal impairment is not expected to significantly influence pazopanib pharmacokinetics or exposure.
Concurrent drug therapy issues:
- Chemotherapy: Increased toxicity and mortality has been observed in trials evaluating concurrent use of pazopanib with other chemotherapeutic agents (pemetrexed, lapatinib). Pazopanib is not approved for use in combination with other chemotherapy.
- Drug-drug/drug-food interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- East Asians: In an analysis of pooled clinical trials, grade 3 and 4 neutropenia, thrombocytopenia, and palmar-plantar erythrodysesthesia syndrome (hand-foot syndrome) were more frequently observed in patients of East Asian descent than in non-East Asian patients.
- Elderly: Patients >65 years of age may be at greater risk for transaminase elevations (ALT >3 time ULN). Patients ≥65 years of age experienced increased incidences of grade 3 or 4 fatigue, hypertension, decreased appetite, and transaminase elevations and are at increased risk for hepatotoxicity.
- Pediatric: Pazopanib is not approved for use in pediatric patients. Based on the mechanism of action, organ growth and maturation may be affected during early postnatal development. May potentially cause serious adverse effects on organ development, particularly in children <2 years of age.
- Pharmacogenomic variation: A pooled analysis of TA repeat polymorphism of UGT1A1 showed a statistically significant increase of hyperbilirubinemia in patients with the (TA)7/TA7 genotype (UGT1A1*28/*28), relative to the (TA)6/(TA)6 and (TA6/(TA)7 genotypes. In a large pooled analysis, grade 2 and 3 ALT elevations (ALT > 3 to <20 x ULN) were observed more frequently in patients carrying the HLA-B*57:01 allele versus non-carriers. Monitor liver function in all patients receiving pazopanib.
Monitoring Parameters
Monitor liver function tests (ALT, AST, bilirubin) at baseline; at weeks 3, 5, 7, and 9; at months 3 and 4; and as clinically necessary, then periodically after month 4 (monitor more frequently if clinically indicated); serum electrolytes (eg, calcium, magnesium, potassium); urinalysis (for proteinuria; baseline and periodic), 24-hour urine protein (if clinically indicated); thyroid function (TSH and T4 at baseline and TSH every 6 to 8 weeks during treatment [Appleby 2011]); verify pregnancy status (in women of reproductive potential) prior to therapy initiation; blood pressure; ECG (baseline and periodic); LVEF (if at risk for cardiac dysfunction; baseline and periodic); signs/symptoms of GI perforation or fistula, venous/arterial thrombotic events, pulmonary embolism, interstitial lung disease/pneumonitis, infection, heart failure, or neurological changes. Monitor adherence.
Pregnancy
Pregnancy Considerations
Based on its mechanism of action, pazopanib would be expected to cause fetal harm if administered to a pregnant woman. Verify pregnancy status in women of reproductive potential prior to initiating treatment. Women of reproductive potential should avoid becoming pregnant during treatment and use effective contraception during therapy and for at least 2 weeks after the last pazopanib dose. Male patients (including vasectomized patients) with pregnant partners or with female partners of reproductive potential should use condoms during treatment and for at least 2 weeks after the last pazopanib dose.
Patient Education
What is this drug used for?
- It is used to treat kidney cancer.
- It is used to treat soft tissue sarcoma.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Loss of strength and energy
- Nausea
- Vomiting
- Diarrhea
- Abdominal pain
- Lack of appetite
- Change in taste
- Mouth irritation
- Mouth sores
- Skin discoloration
- Hair discoloration
- Hair loss
- Muscle pain
- Bone pain
- Weight loss
- Trouble sleeping
- Nail changes
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Low thyroid level like constipation; difficulty handling heat or cold; memory problems; mood changes; or burning, numbness, or tingling feeling.
- Electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting.
- Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood.
- DVT like swelling, warmth, numbness, change in color, or pain in the extremities.
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes.
- Severe pulmonary disorder like lung or breathing problems like trouble breathing, shortness of breath, or a cough that is new or worse.
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out.
- Posterior reversible encephalopathy syndrome like confusion, not alert, vision changes, seizures, or severe headache.
- Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome like bruising or bleeding; loss of strength and energy; dark urine or yellow skin; pale skin; change in amount of urine passed; vision changes; change in strength on one side is greater than the other; difficulty speaking or thinking, or change in balance; or fever.
- Chest pain
- Fast heartbeat
- Passing out
- Severe headache
- Dizziness
- Vision changes
- Unable to pass urine
- Change in amount of urine passed
- Redness or irritation of palms or soles of feet
- Abdominal swelling
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.