Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution Pen-injector, Subcutaneous [preservative free]:
Plegridy: 125 mcg/0.5 mL (0.5 mL) [contains mouse (murine) and/or hamster protein]
Plegridy Starter Pack: 63 mcg/0.5 mL & 94 mcg/0.5 mL (1 mL) [contains mouse (murine) and/or hamster protein]
Solution Prefilled Syringe, Subcutaneous:
Plegridy: 125 mcg/0.5 mL (0.5 mL) [contains mouse (murine) and/or hamster protein]
Plegridy Starter Pack: 63 mcg/0.5 mL & 94 mcg/0.5 mL (1 mL) [contains mouse (murine) and/or hamster protein]
Pharmacology
Mechanism of Action
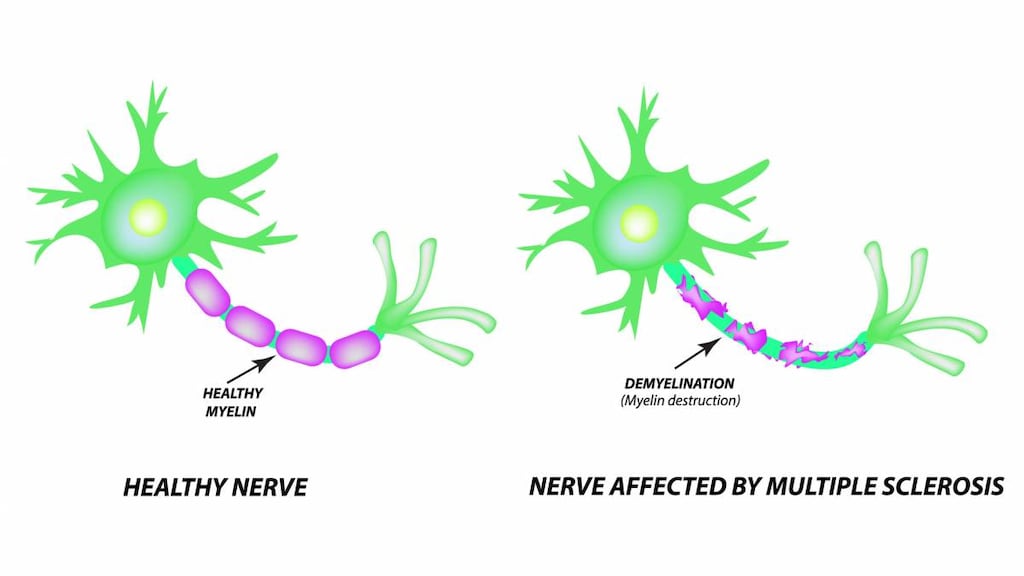
Interferon beta differs from the naturally occurring human protein by a single amino acid substitution and the lack of carbohydrate side chains; alters the expression and response to surface antigens and can enhance immune cell activities. Properties of interferon beta that modify biologic responses are mediated by cell surface receptor interactions; mechanism in the treatment of multiple sclerosis is unknown.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: 481 L
Metabolism
Not extensively metabolized in the liver
Excretion
Urine (major)
Time to Peak
1 to 1.5 days
Half-Life Elimination
~78 hours (multiple sclerosis patients)
Use in Specific Populations
Special Populations: Renal Function Impairment
Renal impairment can increase the Cmax and AUC for peginterferon beta-1a. The half-life was 53, 49, and 82 hours in patients with mild, moderate, and severe renal impairment, respectively.
Use: Labeled Indications
Multiple sclerosis, relapsing: Treatment of patients with relapsing forms of multiple sclerosis, including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease
Contraindications
Hypersensitivity to natural or recombinant interferon beta or peginterferon, or any component of the formulation
Documentation of allergenic cross-reactivity for interferons is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Pregnancy; current severe depression and/or suicidal ideation
Dosage and Administration
Dosing: Adult
Multiple sclerosis, relapsing: SubQ: Initial: 63 mcg on day 1; 94 mcg on day 15. Maintenance: 125 mcg every 14 days beginning on day 29. Note: Analgesics and/or antipyretics may help decrease flu-like symptoms during treatment.
Dosing: Geriatric
Refer to adult dosing.
Reconstitution
Allow prefilled syringe or pen to warm to room temperature (~30 minutes) prior to injection; do not use external heat sources (eg, hot water) to warm.
Administration
Subcutaneous: The first injection should be administered under the supervision of a health care professional.
Administer subcutaneously in the abdomen, back of the upper arm, or thigh; rotate injection sites; do not inject into area where skin is red, irritated, bruised or scarred.
Storage
Store in the closed original carton to protect from light, between 2°C and 8°C (36°F and 46°F). Do not freeze; discard if frozen.
If refrigeration is unavailable, may store between 2°C and 25°C (36°F and 77°F) for up to 30 days, protected from light. May remove from, and return to, a refrigerator if necessary. The total combined time out of refrigeration, within a temperature range of 2°C to 25°C (36°F to 77°F), should not exceed 30 days.
Drug Interactions
Cladribine: May enhance the adverse/toxic effect of Interferons (Beta). Specifically, the risk for lymphopenia may be increased. Avoid combination
Pegloticase: May diminish the therapeutic effect of PEGylated Drug Products. Monitor therapy
Pegvaliase: PEGylated Drug Products may enhance the adverse/toxic effect of Pegvaliase. Specifically, the risk of anaphylaxis or hypersensitivity reactions may be increased. Monitor therapy
Zidovudine: Interferons may enhance the adverse/toxic effect of Zidovudine. Interferons may decrease the metabolism of Zidovudine. Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Headache (44%), chills (17%)
Dermatologic: Injection site pruritus (13%)
Local: Injection site reaction (66%; severe: 3%), erythema at injection site (62%), pain at injection site (15%)
Neuromuscular & skeletal: Myalgia (19%), asthenia (13%), arthralgia (11%)
Respiratory: Flu-like symptoms (47%)
Miscellaneous: Fever (45%)
1% to 10%:
Central nervous system: Increased body temperature (6%), pain (5%), hyperthermia (4%)
Dermatologic: Pruritus (4%), rash at injection site (2%)
Endocrine & metabolic: Increased serum ALT (6%; >5 x ULN: 2%), increased gamma-glutamyl transferase (3%)
Gastrointestinal: Nausea (9%), vomiting (5%)
Hematologic and oncologic: Decreased white blood cell count (<3 x 109/L: 7%)
Hepatic: Increased serum AST (4%)
Immunologic: Antibody development (to PEG: 7%; neutralizing antibodies <1%)
Local: Hematoma at injection site (3%), swelling at injection site (3%), warm sensation at injection site (3%)
<1%, postmarketing, and/or case reports: Angioedema, hepatic disease, increased serum transaminases (combined with increased serum bilirubin), severe neutropenia, severe thrombocytopenia, thrombotic microangiopathy tissue necrosis at injection site, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Autoimmune disorders: Idiopathic thrombocytopenia, hyper- and hypothyroidism, and autoimmune hepatitis have been reported. Consider discontinuing treatment in patients who develop a new autoimmune disorder.
- Bone marrow suppression: May cause decreased peripheral blood cell counts in all cell lines, including rare instances of pancytopenia and severe thrombocytopenia. Monitor CBC with differential and platelets; monitor patients for infections, bleeding, and symptoms of anemia. Patients with preexisting myelosuppression may need more intensive monitoring.
- Hepatic effects: Severe hepatic injury, including hepatitis, autoimmune hepatitis, and severe hepatic failure (rare) have been reported; asymptomatic elevation of hepatic transaminases has also been reported and has recurred upon rechallenge. Monitor for signs and symptoms of hepatic injury.
- Hypersensitivity: Anaphylaxis and other serious allergic reactions (eg, angioedema, urticaria) may occur (rare); discontinue therapy if a serious allergic reaction occurs and institute appropriate supportive therapy.
- Injection site reactions: Injection site reactions (eg, injection site erythema, pain, pruritus, edema, necrosis) can occur with subcutaneous use. If necrosis occurs at a single site, avoid administration near the affected area; if multiple lesions occur, discontinue until healing occurs.
- Neuropsychiatric disorders: Depression, suicidal ideation and suicide have been reported; monitor for symptoms of depression and suicidal ideation; consider discontinuing treatment with development of depression or other severe psychiatric symptoms.
- Thrombotic microangiopathy: Thrombotic microangiopathy (TMA), including thrombotic thrombocytopenic purpura (TTP) or hemolytic uremic syndrome (HUS), has been reported (some fatal) with interferon beta products. Cases have been reported several weeks to years after initiating therapy. Monitor for new-onset hypertension, thrombocytopenia, renal impairment; discontinue use in patients who develop TMA and manage appropriately (Hunt 2014; Mahe 2013).
Disease-related concerns:
- Cardiovascular disease: Congestive heart failure (CHF), cardiomyopathy, and cardiomyopathy with CHF may occur in patients receiving interferon beta. Monitor patients with significant cardiac disease for worsening of their cardiac condition during initiation and continuation of therapy.
- Renal impairment: Use with caution in severe renal impairment; increased drug exposure may occur; monitor for adverse reactions.
- Seizures: May cause seizures; use with caution in patients with a seizure disorder.
Dosage form specific issues:
- Product variability: Due to differences in dosage, patients should not change brands of interferon.
Monitoring Parameters
CBC with differential and platelets, transaminase levels; signs and symptoms of hepatic injury, hypersensitivity, infections, bleeding, new onset autoimmune disorders, psychiatric disorders (including depression and/or suicidal ideation), new onset/worsening cardiovascular disease; adverse reactions in patients with severe renal impairment (CrCl <30 mL/minute); injection site reactions; signs/symptoms of thrombotic microangiopathy (eg, new-onset hypertension, thrombocytopenia, renal impairment).
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Information related to the use of peginterferon beta-1a in pregnancy is limited (MacDonald 2018).
In general, disease-modifying therapies for multiple sclerosis (MS) are stopped prior to a planned pregnancy, and not initiated during pregnancy, except in females at high risk of MS activity (AAN [Rae-Grant 2018]). Consider use of agents other than peginterferon beta-1a for females at high risk of disease reactivation who are planning a pregnancy. Delaying pregnancy is recommended for females with persistent high disease activity; when disease-modifying therapy is needed in these patients, other agents are preferred (ECTRIMS/EAN [Montalban 2018]).
A pregnancy registry has been established to monitor outcomes of females exposed to peginterferon beta-1a during pregnancy (866-810-1462 or https://www.plegridypregnancyregistry.com/).
Patient Education
What is this drug used for?
- It is used to treat MS (multiple sclerosis).
Frequently reported side effects of this drug
- Flu-like symptoms
- Nausea
- Vomiting
- Muscle pain
- Joint pain
- Injection site irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome like bruising or bleeding; loss of strength and energy; dark urine or yellow skin; pale skin; change in amount of urine passed; vision changes; change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance; or fever
- Depression like thoughts of suicide, anxiety, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Thyroid problems like change in weight without trying, anxiety, feeling restless, feeling very weak, hair thinning, depression, neck swelling, difficulty focusing, inability handling heat or cold, menstrual changes, tremors, or sweating
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out
- Seizures
- Sore throat
- Bruising
- Bleeding
- Severe loss of strength and energy
- Injection site skin breakdown, skin discoloration, swelling, or drainage of fluid
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.