Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet Extended Release, Oral:
Generic: 400 mg
Pharmacology
Mechanism of Action
Pentoxifylline increases blood flow to the affected microcirculation. Although the precise mechanism of action is not well-defined, blood viscosity is lowered, erythrocyte flexibility is increased, leukocyte deformability is increased, and neutrophil adhesion and activation are decreased. Overall, tissue oxygenation is significantly increased.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Metabolism
Hepatic to multiple metabolites; undergoes extensive first-pass effect; Pentoxifylline undergoes reduction to metabolite I (active), and oxidation to form metabolite V (active) (Ward 1987); Note: Plasma concentrations of M-1 and M-V are 5 and 8 times greater, respectively, than pentoxifylline
Excretion
Urine (0% as unchanged, 50% to 80% as M-V metabolite, 20% as other metabolites); feces (<4%)
Onset of Action
2 to 4 weeks with multiple doses
Time to Peak
Serum: 2 to 4 hours
Half-Life Elimination
Parent drug: 24 to 48 minutes; Metabolites: 60 to 96 minutes
Use in Specific Populations
Special Populations: Renal Function Impairment
In patients with mild to moderate renal impairment, AUC0-tss and Cmax of the active Metabolite V increased 2.4- and 2.1-fold, respectively. In patients with severe renal impairment, the AUC0-tss and Cmax of active Metabolite V increased 12.9- and 10.6-fold, respectively. Twice daily administration increased the exposure to metabolite V only slightly in both groups.
Special Populations: Hepatic Function Impairment
Following a single dose of pentoxifylline, the AUC increased 6.5-fold and the Cmax increased 7.5-fold in patients with mild to moderate hepatic impairment. The AUC and Cmax of active Metabolite I also increased 6.9- and 8.2-fold, respectively. Studies were not conducted in patients with severe hepatic failure.
Special Populations: Elderly
Pentoxifylline: Increased AUC and decreased elimination rate (60 to 68 years of age).
Use: Labeled Indications
Intermittent claudication: Treatment of intermittent claudication on the basis of chronic occlusive arterial disease of the limbs.
Limitations of use: May improve function and symptoms, but not intended to replace more definitive therapy. Note: The American College of Chest Physicians (ACCP) discourages the use of pentoxifylline for the treatment of intermittent claudication refractory to exercise therapy (and smoking cessation) (Guyatt, 2012).
Use: Off Label
Alcoholic hepatitis (severe)yes
Based on the American College of Gastroenterology for Alcoholic Liver Disease guideline, existing evidence does not support the use of pentoxifylline in the management of severe alcoholic hepatitis; however, certain patient subgroups, such as those with concomitant renal failure, may benefit. The American Association for the Study for Liver Disease Practice Guideline recommends that pentoxifylline be considered in patients with severe alcoholic hepatitis, especially if there are contraindications to steroid therapy.
Venous leg ulcers (with compression therapy)a
Based on a meta-analysis of trials evaluating the treatment of venous leg ulcers with compression therapy, the use of pentoxifylline was shown to be safe and effective Jull 2012.
Contraindications
Patients previously exhibiting intolerance to pentoxifylline, xanthines (eg, caffeine, theophylline), or any component of the formulation; recent cerebral and/or retinal hemorrhage
Canadian labeling: Additional contraindications (not in US labeling): Acute MI, severe coronary artery disease when myocardial stimulation might prove harmful, peptic ulcers (current or recent)
Dosage and Administration
Dosing: Adult
Alcoholic hepatitis (severe) (Maddrey Discriminant Function [MDF] score ≥32, especially when corticosteroids contraindicated) (off-label use): Oral: 400 mg 3 times daily for 4 weeks (AASLD [O’Shea 2010], ACG [Singal 2018]).
Intermittent claudication: Oral: 400 mg 3 times daily; maximal therapeutic benefit may take 2 to 4 weeks to develop; recommended to maintain therapy for at least 8 weeks. May reduce to 400 mg twice daily if GI or CNS side effects occur; discontinue if side effects persist.
Note: Use for the treatment of intermittent claudication refractory to exercise therapy (and smoking cessation) has been discouraged by The American College of Chest Physicians (ACCP) (Guyatt 2012).
Venous leg ulcer (off-label use): Oral: 400 mg 3 times daily (with compression therapy) (Jull 2012; Robson 2006).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Kawasaki disease; adjunctive: Limited data available, efficacy results variable (Nash 1996); AHA recommendations do not address pentoxifylline for the treatment of Kawasaki disease (AHA [McCrindle 2017]): Infants ≥2 months and Children: Oral: 20 mg/kg/day in 3 divided doses in combination with standard IV immunoglobulin and aspirin therapy; specific role in disease management undefined; data suggests use in patients with high serum concentrations of TNF may be appropriate (Best 2003; Furukawa 1994); the initial trial (n=22, mean age: 2 years, youngest: 6 months) reported a lower incidence of coronary artery lesions in patient receiving pentoxifylline compared to those who did not; all patients received aspirin and IV gamma globulin therapy (Furukawa 1994).
Extemporaneously Prepared
A 20 mg/mL oral suspension may be made using tablets. Crush ten 400 mg tablets and reduce to a fine powder. Add a small amount of purified water and mix to a uniform paste; mix while adding purified water to almost 200 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 200 mL. Label "shake well" and "refrigerate". Stable 91 days.
Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Administer with food. Swallow whole; do not chew, crush, or divide.
Dietary Considerations
May be taken with meals.
Storage
Store between 20°C to 25°C (68°F to 77°F); protect from light.
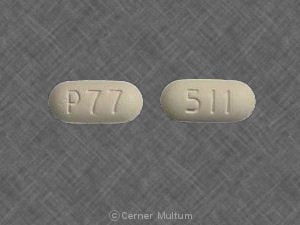
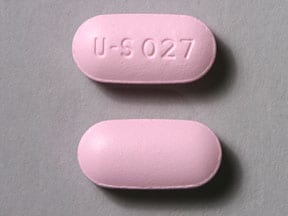
Pentoxifylline Images
Drug Interactions
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): Pentoxifylline may enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Blood Pressure Lowering Agents: Pentoxifylline may enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Cimetidine: May increase the serum concentration of Pentoxifylline. Monitor therapy
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of Pentoxifylline. Monitor therapy
CYP1A2 Inhibitors (Strong): May increase the serum concentration of Pentoxifylline. Monitor therapy
Heparin: Pentoxifylline may enhance the anticoagulant effect of Heparin. Monitor therapy
Heparins (Low Molecular Weight): Pentoxifylline may enhance the anticoagulant effect of Heparins (Low Molecular Weight). Monitor therapy
Ketorolac (Nasal): May enhance the adverse/toxic effect of Pentoxifylline. Specifically, the risk of bleeding may be increased. Avoid combination
Ketorolac (Systemic): May enhance the adverse/toxic effect of Pentoxifylline. Specifically, the risk of bleeding may be increased with this combination. Avoid combination
Theophylline Derivatives: Pentoxifylline may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Pentoxifylline may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
Concomitant administration increases theophylline levels
Adverse Reactions
1% to 10%: Gastrointestinal: Nausea (2%), vomiting (1%)
<1%, postmarketing, and/or case reports: Anaphylactic shock, anaphylactoid reaction, anaphylaxis, angioedema, angina pectoris, anorexia, anxiety, aplastic anemia, aseptic meningitis, bloating, blurred vision, cardiac arrhythmia, chest pain, cholecystitis, confusion, conjunctivitis, constipation, decreased serum fibrinogen, depression, dysgeusia, dyspnea, edema, epistaxis, eructation, flatulence, flu-like symptoms, hallucination, hepatitis, hypotension, increased liver enzymes, jaundice, laryngitis, leukemia, leukopenia, malaise, nail disease (brittle fingernails), nasal congestion, otalgia, pancytopenia, pruritus, purpura, scotoma, seizure, sialorrhea, skin rash, sore throat, tachycardia, thrombocytopenia, tremor, urticaria, weight changes, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylaxis/anaphylactoid reactions: Discontinue at first sign of anaphylaxis or anaphylactoid reaction.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with mild to moderate hepatic impairment; the bioavailability of pentoxifylline and metabolite I is increased. Has not been studied in patients with severe hepatic disease.
- Renal impairment: Use with caution in patients with renal impairment; bioavailability of active metabolite V may be increased.
Special populations:
- Elderly: Use with caution in the elderly due to the potential for cardiac, hepatic, or renal impairment.
Monitoring Parameters
Renal function; hemoglobin/hematocrit (especially in high risk patients)
Pregnancy
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies.
Pentoxifylline may be used to test sperm viability when evaluating nonfertile males (ASRM 2015). It has also been evaluated for the treatment of infertility due to endometriosis, but use for this purpose is not currently recommended (Lu 2012).
Patient Education
What is this drug used for?
- It is used to ease pain, numbness, and tingling in the legs.
- It is used to treat certain blood vessel problems.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Burping
- Bloating
- Dizziness
- Passing gas
- Headache
- Vomiting
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Chest pain
- Arrhythmia
- Severe dizziness
- Passing out
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.