Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
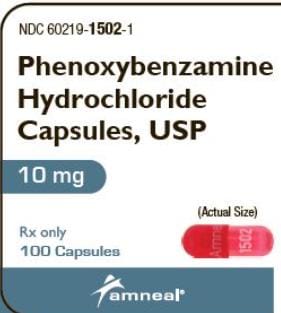
Capsule, Oral, as hydrochloride:
Dibenzyline: 10 mg [contains fd&c yellow #6 (sunset yellow)]
Generic: 10 mg
Pharmacology
Mechanism of Action
Produces long-lasting noncompetitive alpha-adrenergic blockade of postganglionic synapses in exocrine glands and smooth muscle; relaxes urethra and increases opening of the bladder
Pharmacokinetics/Pharmacodynamics
Distribution
Distributes to and may accumulate in adipose tissues
Excretion
Primarily in urine and bile
Onset of Action
Within 2 hours; Maximum effect: Within 4 to 6 hours
Duration of Action
IV: ≥3 to 4 days
Half-Life Elimination
IV: ~24 hours
Use: Labeled Indications
Pheochromocytoma: Treatment of sweating and hypertension associated with pheochromocytoma.
Use: Off Label
Hypertensive crisis caused by sympathomimetic amines; Micturition problems associated with neurogenic bladder, functional outlet obstruction, and partial prostate obstruction
Contraindications
Hypersensitivity to drug or any component of the formulation; conditions in which a fall in blood pressure may be undesirable.
Dosage and Administration
Dosing: Adult
Pheochromocytoma: Oral: Initial: 10 mg twice daily; may increase slowly every other day until optimal blood pressure response is achieved; usual dosage range: 20 to 40 mg 2 to 3 times daily. Doses up to 240 mg daily have been reported (Kinney 2000).
Micturition disorders (off-label use): Oral: 10 to 20 mg 1 to 2 times daily (Te 2002)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Pheochromocytoma, preoperative management: Limited data available: Children and Adolescents: Oral: Initial: 0.2 to 0.25 mg/kg/dose once or twice daily; maximum dose: 10 mg/dose; slowly titrate (eg, every 4 days) to effect; increments of 0.2 mg/kg/day have been reported; reported maintenance dose range: 0.4 to 3 mg/kg/day in divided doses every 6 to 8 hours; maximum single maintenance dose: 40 mg/dose; maximum daily dose: 4 mg/kg/day (Hack 1999; Kliegman 2007; Romero 2015; Sperling 2014)
Extemporaneously Prepared
A 2 mg/mL oral suspension may be made with capsules, propylene glycol 1%, and citric acid 0.15% in distilled water. Prepare the vehicle by dissolving 150 mg citric acid in a minimal amount of distilled water. Add 1 mL propylene glycol and mix well; add quantity of distilled water sufficient to make 100 mL (only a small portion of this vehicle will be used to make the final product). Grind the contents of two phenoxybenzamine 10 mg capsules in a mortar and reduce to a fine powder. Add a small portion of the vehicle and mix to a uniform paste; transfer to a graduated cylinder, rinse mortar with vehicle, and add quantity of prepared vehicle sufficient to make 10 mL. Transfer to an amber glass prescription bottle with tight-fitting cap; label "shake well" and "refrigerate". Stable for 7 days when stored in amber glass prescription bottles and refrigerated.
A stock solution of 10 mg/mL in propylene glycol was stable for 30 days refrigerated. When this stock solution was diluted 1:4 (v/v) with syrup (66.7% sucrose) to 2 mg/mL, the preparation was stable for 1 hour refrigerated. Note: Although the stock solution is stable for 30 days, it must be diluted before administration to decrease the amount of propylene glycol delivered to the patient.
Lim LY, Tan LL, Chan EW, et al, "Stability of Phenoxybenzamine Hydrochloride in Various Vehicles," Am J Health Syst Pharm, 1997, 54(18):2073-8.9377206
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Phenoxybenzamine Images
Drug Interactions
Alpha-/Beta-Agonists: Alpha1-Blockers may diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Similarly, Alpha-/Beta-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
Alpha1-Agonists: Alpha1-Blockers may diminish the vasoconstricting effect of Alpha1-Agonists. Similarly, Alpha1-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
Alpha1-Blockers: May enhance the antihypertensive effect of other Alpha1-Blockers. Avoid combination
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta-Blockers: May enhance the orthostatic hypotensive effect of Alpha1-Blockers. The risk associated with ophthalmic products is probably less than systemic products. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Calcium Channel Blockers: Alpha1-Blockers may enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Dapoxetine: May enhance the orthostatic hypotensive effect of Alpha1-Blockers. Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Alpha1-Blockers (Nonselective). Management: Ensure patient is stable on one agent prior to initiating the other, and always initiate combination using the lowest possible dose of the drug being added. When tadalafil is used for treatment of BPH, concurrent alpha 1-blockers are not recommended. Consider therapy modification
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Rilmenidine: Alpha1-Blockers may enhance the hypotensive effect of Rilmenidine. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Adverse Reactions
Frequency not defined.
Cardiovascular: Orthostatic hypotension, tachycardia
Central nervous system: Drowsiness, fatigue, inhibited ejaculation
Gastrointestinal: Gastrointestinal irritation
Ophthalmic: Miosis
Respiratory: Nasal congestion
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular effects: An exaggerated hypotensive response and tachycardia may occur when administered concurrently with compounds that stimulate both alpha- and beta-adrenergic receptors.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with marked cerebral or coronary atherosclerosis.
- Renal impairment: Use with caution in patients with renal impairment.
- Respiratory infection: May aggravate symptoms of respiratory infections.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity ("gasping syndrome") in neonates; the "gasping syndrome" consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC, 1982); some data suggest that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer's labeling.
Other warnings/precautions:
- Long-term use: Not recommended for long-term use due to case reports of cancer in humans; carefully weigh the risk and benefits before use.
Monitoring Parameters
Blood pressure, pulse, orthostatics
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adequate animal reproduction studies have not been conducted. It is not known whether phenoxybenzamine can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience fatigue, stuffy nose, nausea, or loss of strength and energy. Have patient report immediately to prescriber severe dizziness, passing out, fast heartbeat, sexual dysfunction, or small pupils (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.