Boxed Warning
Experienced physician (injection):
Physicians should completely familiarize themselves with the complete contents of this monograph before prescribing phenylephrine injection.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Liquid, Oral, as hydrochloride:
Little Colds Decongestant: 2.5 mg/mL (30 mL) [alcohol free, dye free, saccharin free; contains sodium benzoate; grape flavor]
Solution, Injection, as hydrochloride:
Generic: 10 mg/mL (5 mL [DSC], 10 mL [DSC])
Solution, Intravenous, as hydrochloride:
Vazculep: 10 mg/mL (1 mL, 5 mL, 10 mL) [contains sodium metabisulfite]
Generic: 10 mg/mL (1 mL, 5 mL [DSC], 10 mL [DSC])
Solution, Intravenous, as hydrochloride [preservative free]:
Biorphen: 0.5 mg/5 mL (5 mL) [sulfate free]
Generic: 10 mg/mL (1 mL, 5 mL, 10 mL)
Solution, Oral, as hydrochloride:
Sudafed PE Childrens: 2.5 mg/5 mL (118 mL) [alcohol free, sugar free; contains edetate disodium, fd&c red #40, sodium benzoate; berry flavor]
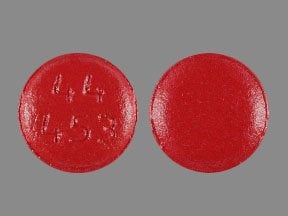
Tablet, Oral, as hydrochloride:
Medi-Phenyl: 5 mg [DSC] [pseudoephedrine free; contains fd&c red #40, fd&c yellow #6 (sunset yellow)]
Nasal Decongestant: 10 mg [contains fd&c blue #2 (indigotine), fd&c red #40, fd&c yellow #6 aluminum lake]
Non-Pseudo Sinus Decongestant: 10 mg [contains fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Sudafed PE Sinus Congestion: 10 mg [contains fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Sudogest PE: 10 mg [contains fd&c red #40]
Sudogest PE: 10 mg [gluten free; contains fd&c red #40 aluminum lake]
Pharmacology
Mechanism of Action
Potent, direct-acting alpha-adrenergic agonist with virtually no beta-adrenergic activity; produces systemic arterial vasoconstriction. Such increases in systemic vascular resistance may result in dose-dependent increases in systolic and diastolic blood pressure and reductions in heart rate and cardiac output (most noticeable in patients with preexisting cardiac dysfunction).
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Erratic and incomplete (Kanfer 1993)
Distribution
Vd: Initial: 26 to 61 L; Vdss: 184 to 543 L (mean: 340 L) (Hengstmann 1982)
Metabolism
Hepatic via oxidative deamination (Oral: 24%; IV: 50%); Undergoes sulfation (Oral [mostly within gut wall]: 46%; IV: 8%) and some glucuronidation; forms inactive metabolites (Kanfer 1993)
Excretion
Urine (mostly as inactive metabolites)
Onset of Action
Blood pressure increase/vasoconstriction: IM, SubQ: 10 to 15 minutes; IV: Immediate
Nasal decongestant: Oral: 15 to 30 minutes (Kollar 2007)
Time to Peak
Oral: 0.75 to 2 hours (Kanfer 1993)
Duration of Action
Blood pressure increase/vasoconstriction: IM: 1 to 2 hours; IV: ~15 to 20 minutes; SubQ: 50 minutes
Nasal decongestant: Oral: ≤4 hours (Kollar 2007)
Half-Life Elimination
Alpha phase: ~ 5 minutes; Terminal phase: 2 to 3 hours (Hengstmann 1982; Kanfer 1993)
Use: Labeled Indications
Hypotension/shock: Treatment of hypotension, vascular failure in shock. Note: Not recommended for routine use in the treatment of septic shock; use should be limited until more evidence demonstrating positive clinical outcomes becomes available (Rhodes 2017).
Guideline recommendations:
Cardiogenic shock: The 2017 American Heart Association (AHA) scientific statement for the Contemporary Management of Cardiogenic Shock recommends phenylephrine, if needed, be considered for initial vasoactive management of cardiogenic shock due to aortic stenosis, mitral stenosis, or dynamic left ventricular outflow tract (LVOT) obstruction (AHA [van Diepen 2017]).
Hypotension during anesthesia: As a vasoconstrictor in regional analgesia
Nasal congestion: As a decongestant [OTC]
Use: Off Label
Hypotension in patients with obstructive hypertrophic cardiomyopathycyes
Phenylephrine is a pure alpha1 agonist that will increase systemic vascular resistance without increasing heart rate or contractility. This is advantageous in patients with obstructive hypertrophic cardiomyopathy and hypotension since increases in both heart rate and contractility may cause the obstruction to worsen, leading to a decrease in cardiac output. Other vasopressors like dopamine, epinephrine, and norepinephrine may increase contractility and/or heart rate Hensley 2015, Nishimura 2004.
Based on the American College of Cardiology Foundation/American Heart Association Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy, the use of phenylephrine is recommended for patients with obstructive hypertrophic cardiomyopathy who develop acute hypotension unresponsive to fluid administration.
Priapism (ischemic)byes
Data from an open-label nonrandomized study supports the use of phenylephrine in the treatment of ischemic priapism Dittrich 1991. Higher doses have been employed with continuous cardiovascular monitoring for patients who have not responded to usual dosing; however, this dosing cannot be recommended as routine Munarriz 2006. Additional trials may be necessary to further define the role of phenylephrine in this condition.
Based on the American Urological Association guidelines for the management of priapism, due to the low risk of cardiovascular side effects intracavernous injection of phenylephrine is recommended for ischemic priapism that persists following aspiration/irrigation.
Contraindications
There are no contraindications listed in the manufacturer's labeling.
OTC labeling (Oral): When used for self-medication: Use with or within 14 days of monoamine oxidase inhibitor therapy
Dosage and Administration
Dosing: Adult
Hypotension/shock: Note: The Society of Critical Care Medicine (SCCM) does not recommend phenylephrine for septic shock except in the following circumstances: When norepinephrine (preferred first-line agent) is associated with serious arrhythmias, when cardiac output is known to be high and blood pressure persistently low, or when the combination of inotrope/vasopressor and low-dose vasopressin failed to achieve target mean arterial pressure and phenylephrine is used as salvage therapy (Rhodes 2017). Vasopressors should be used if patient is hypotensive during or after fluid resuscitation to maintain goal mean arterial pressure (MAP) ≥65 mm Hg (AHA [Peberdy 2010]; Levy 2018). Titrate to lowest effective dose. Institutional protocols may vary with weight-based or non-weight dose regimens.
Septic/vasodilatory shock: IV infusion: 0.5 to 6 mcg/kg/minute; titrate to desired MAP. Dosing ranges between 0.4 to 9.1 mcg/kg/minute have been reported when treating septic shock (Flancbaum 1997; Gregory 1991; Hollenberg 2004).
Post cardiac arrest (off-label dose): Note: For vasoactive management of severe hypotension ([eg, systolic blood pressure <70 mm Hg] and low total peripheral resistance) during/after cardiac arrest.
IV infusion: Initial dose: 0.5 to 2 mcg/kg/minute; titrate to effect (AHA [Peberdy 2010]).
Cardiogenic shock (off-label dose): Note: For initial vasoactive management of cardiogenic shock due to aortic stenosis, mitral stenosis, or dynamic left ventricular outflow tract obstruction.
IV infusion: 0.1 to 10 mcg/kg/minute (AHA [van Diepen 2017]).
Hypotension during anesthesia:
IV bolus: Initial: 40 to 100 mcg/dose; may repeat every 1 to 2 minutes as needed (total dose should not exceed 200 mcg) or 50 to 100 mcg (usual range: 50 to 250 mcg); titrate to achieve blood pressure goal.
IV infusion: Initial dose: 10 to 35 mcg/minute (not to exceed 200 mcg/minute) or 0.5 to 1.4 mcg/kg/minute; titrate to blood pressure goal.
Nasal congestion: Oral: OTC labeling: 10 mg every 4 hours as needed for ≤7 days (maximum: 60 mg/24 hours).
Priapism (ischemic) (off-label use): Intracavernous (off-label route): 100 to 500 mcg every 3 to 5 minutes (using a concentration of 100 to 500 mcg/mL) over the course of ~1 hour; lower concentrations in smaller volumes should be used in patients with severe cardiovascular disease (AUA [Montague 2003]).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosing presented in both mg (oral) and mcg (parenteral); use caution when ordering and dispensing.
Nasal congestion: Oral:
Children 4 to 5 years: 2.5 mg every 4 hours; maximum daily dose: 15 mg in 24 hours
Children 6 to 11 years: 5 mg every 4 hours; maximum daily dose: 30 mg in 24 hours
Children ≥12 years and Adolescents: 10 mg every 4 hours; maximum daily dose: 60 mg in 24 hours
Hypotension, low cardiac output: Infants, Children, and Adolescents:
IM, SubQ: 100 mcg/kg/dose every 1 to 2 hours as needed; maximum dose: 5000 mcg
IV bolus: 5 to 20 mcg/kg/dose every 10 to 15 minutes as needed (AAP, 1998; Shaddy, 1989); initial dose should not exceed 500 mcg; maximum dose: 1000 mcg
Continuous IV infusion: Usual initial dose: 0.1 to 0.5 mcg/kg/minute; titrate to desired response (Di Gennaro, 2010; Stewart, 2002; Wessel, 2001); in cases of shock or intraoperative hypotension, doses up to 2 mcg/kg/minute have been reported (Di Gennaro, 2010; Kliegman, 2011; Shaddy, 1989; Stewart, 2002) and for management of infundibular spasm (Tet Spell), even higher doses up to 5 mcg/kg/minute may be required (AAP, 1998; Shaddy, 1989)
Hypotension during spinal anesthesia: IM, SubQ: Infants, Children, and Adolescents: 44 to 88 mcg/kg/dose; maximum dose: 500 mcg
Reconstitution
Solution for injection:
IV infusion: May dilute 10 mg in 500 mL NS or D5W. May also dilute 50 mg in 500 mL NS, 100 mg in 500 mL NS, or 1,250 mg in 500 mL NS (Gupta 2004; Weber 1970).
IV bolus injection: Dilute 10 mg (1 mL of 10 mg/mL) in 99 mL of D5W or NS. A ready-to-use formulation requiring no further dilution is also available.
Intracavernous injection (off-label route): Dilute with NS to a concentration of 0.1 to 0.5 mg/mL; lower concentrations should be used for patients with severe cardiovascular disease (AUA [Montague 2003])
Administration
IV:
Hypotension/shock: May be administered via continuous infusion (after diluting). When administering as a continuous infusion, central line administration is preferred. IV infusions require an infusion pump.
Hypotension during anesthesia: Administer as an IV bolus over 20 to 30 seconds.
Vesicant; ensure proper needle or catheter placement prior to and during infusion; avoid extravasation.
Extravasation management: If extravasation occurs, stop infusion immediately and disconnect (leave cannula/needle in place); gently aspirate extravasated solution (do NOT flush the line); remove needle/cannula; elevate extremity. Initiate phentolamine (or alternative antidote). Apply dry warm compresses (Hurst 2004; Reynolds 2014).
Phentolamine: Dilute 5 to 10 mg in 10 to 20 mL NS and administer into extravasation site as soon as possible after extravasation; may readminister if patient remains symptomatic (Reynolds 2014).
Alternative to phentolamine: Nitroglycerin topical 2% ointment (based on limited data): Apply a 1-inch strip to the site of ischemia; may repeat every 8 hours as necessary (Reynolds 2014).
Dietary Considerations
Some products may contain phenylalanine and/or sodium.
Storage
Vials: Store intact vials at 20°C to 25°C (68°F to 77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Protect from light.
IV infusion: Concentrations of 0.1 and 0.2 mg/mL in NS are stable for at least 14 days at room temperature of 25°C (77°F) (Gupta 2004). Dilution of 2.5 mg/mL in NS retained potency for at least 24 hours at 22°C (Weber 1970). The manufacturer's labeling for 10 mg/mL products state to store diluted solutions for ≤4 hours at room temperature or ≤24 hours refrigerated.
Stability in syringes: Concentration of 0.1 mg/mL in NS (polypropylene syringes) is stable for at least 30 days at -20°C (-4°F), 3°C to 5°C (37°F to 41°F), or 23°C to 25°C (73.4°F to 77°F) (Kiser 2007). Vazculep: Do not hold diluted solutions for longer than 4 hours at room temperature or 24 hours refrigerated.
Oral: Store at 15°C to 25°C (59°F to 77°F). Protect from light.
Phenylephrine (Systemic) Images
Drug Interactions
Acetaminophen: May increase the serum concentration of Phenylephrine (Systemic). Monitor therapy
Alpha1-Blockers: May diminish the vasoconstricting effect of Alpha1-Agonists. Similarly, Alpha1-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Benzylpenicilloyl Polylysine: Alpha1-Agonists may diminish the diagnostic effect of Benzylpenicilloyl Polylysine. Management: Consider use of a histamine skin test as a positive control to assess a patient's ability to mount a wheal and flare response. Consider therapy modification
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Chloroprocaine: May enhance the hypertensive effect of Phenylephrine (Systemic). Monitor therapy
CloZAPine: May diminish the therapeutic effect of Phenylephrine (Systemic). Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
Doxofylline: Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. Monitor therapy
Ergot Derivatives: May enhance the hypertensive effect of Alpha1-Agonists. Ergot Derivatives may enhance the vasoconstricting effect of Alpha1-Agonists. Exceptions: Ergoloid Mesylates; Nicergoline. Avoid combination
FentaNYL: Alpha1-Agonists may decrease the serum concentration of FentaNYL. Specifically, fentanyl nasal spray serum concentrations may decrease and onset of effect may be delayed. Monitor therapy
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Hyaluronidase: May enhance the vasoconstricting effect of Phenylephrine (Systemic). Management: Avoid the use of hyaluronidase to enhance dispersion or absorption of phenylephrine. Use of hyaluronidase for other purposes in patients receiving phenylephrine may be considered as clinically indicated. Avoid combination
Iobenguane Radiopharmaceutical Products: Alpha1-Agonists may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Ioflupane I 123: Phenylephrine (Systemic) may diminish the diagnostic effect of Ioflupane I 123. Monitor therapy
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the hypertensive effect of Alpha1-Agonists. While linezolid is expected to interact via this mechanism, management recommendations differ from other monoamine oxidase inhibitors. Refer to linezolid specific monographs for details. Exceptions: Linezolid. Avoid combination
Propacetamol: May increase the serum concentration of Phenylephrine (Systemic). Management: Monitor patients closely for increased side effects of phenylephrine if propacetamol is used concomitantly. Patients with underlying blood pressure issues or arrhythmias may need closer monitoring and may warrant consideration of alternative therapies. Monitor therapy
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Tricyclic Antidepressants: May enhance the therapeutic effect of Alpha1-Agonists. Tricyclic Antidepressants may diminish the therapeutic effect of Alpha1-Agonists. Monitor therapy
Adverse Reactions
Frequency not defined.
Injection:
Cardiovascular: Cardiac arrhythmia (rare), exacerbation of angina, hypertension, hypertensive crisis, ischemia, localized blanching, low cardiac output, peripheral vasoconstriction (severe), reflex bradycardia, visceral vasoconstriction (severe), worsening of heart failure
Central nervous system: Anxiety, dizziness, excitability, headache, insomnia, nervousness, paresthesia, precordial pain (or discomfort), restlessness
Dermatologic: Pallor, piloerection, pruritus
Endocrine & metabolic: Metabolic acidosis
Gastrointestinal: Epigastric pain, gastric irritation, nausea, vomiting
Genitourinary: Decreased renal blood flow, decreased urine output
Hypersensitivity: Hypersensitivity reaction (including skin rash, urticaria, leukopenia, agranulocytosis, thrombocytopenia)
Neuromuscular & skeletal: Neck pain, tremor, weakness
Ophthalmic: Blurred vision
Respiratory: Dyspnea, respiratory distress
Oral: Central nervous system: Anxiety, dizziness, excitability, headache, insomnia, nervousness, restlessness
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular effects: Intravenous use of phenylephrine may cause severe bradycardia (likely baroreflex mediated) and reduced cardiac output due to an increase in cardiac afterload especially in patients with preexisting cardiac dysfunction (Goertz 1993; Yamazaki 1982). May also precipitate angina in patients with severe coronary artery disease and increase pulmonary arterial pressure. Use with caution in patients with preexisting bradycardia, partial heart block, myocardial disease, or severe coronary artery disease. Avoid or use with extreme caution in patients with heart failure or cardiogenic shock; increased systemic vascular resistance may significantly reduce cardiac output. Avoid use in patients with hypertension (contraindicated in severe hypertension); monitor blood pressure closely and adjust infusion rate. May also cause excessive peripheral and visceral vasoconstriction and ischemia to vital organs, particularly in patients with extensive peripheral vascular disease.
- Extravasation: IV administration: Vesicant; ensure proper needle or catheter placement prior to and during infusion. Avoid extravasation.
Disease-related concerns:
- Acidosis: Acidosis may reduce the efficacy of phenylephrine; correct acidosis prior to or during use of phenylephrine.
- Autonomic dysfunction: Patients with autonomic dysfunction (eg, spinal cord injury) may exhibit an exaggerated increase in blood pressure response to phenylephrine.
Concurrent drug therapy issues:
- Monoamine oxidase inhibitors: Use with extreme caution in patients taking monoamine oxidase inhibitors; hypertension may result from concurrent use.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
- Oral: When used for self-medication (OTC), use with caution in patients with asthma, bowel obstruction/narrowing, hyperthyroidism, diabetes mellitus, cardiovascular disease, ischemic heart disease, hypertension, increased intraocular pressure, prostatic hyperplasia, or in the elderly. Notify health care provider if symptoms do not improve within 7 days or are accompanied by fever. Discontinue and contact health care provider if nervousness, dizziness, or sleeplessness occur.
- Sulfites: Some products contain sulfites which may cause allergic reactions in susceptible individuals.
Other warnings/precautions:
- Appropriate use: When used intravenously in patients who are hypotensive, assure adequate circulatory volume to minimize need for vasoconstrictors.
Monitoring Parameters
Blood pressure (or mean arterial pressure), heart rate; cardiac output (as appropriate), intravascular volume status, pulmonary capillary wedge pressure (as appropriate); monitor infusion site closely
Consult individual institutional policies and procedures.
Pregnancy
Pregnancy Considerations
Phenylephrine crosses the placenta at term.
Maternal use of phenylephrine during the first trimester of pregnancy is not strongly associated with an increased risk of fetal malformations; maternal dose and duration of therapy were not reported in available publications. Phenylephrine is available over-the-counter for the symptomatic relief of nasal congestion. Decongestants are not the preferred agents for the treatment of rhinitis during pregnancy. Oral phenylephrine should be avoided during the first trimester of pregnancy; short-term use (<3 days) of intranasal phenylephrine may be beneficial to some patients although its safety during pregnancy has not been studied. Phenylephrine injection is used at delivery for the prevention and/or treatment of maternal hypotension associated with spinal anesthesia in women undergoing cesarean section. Phenylephrine may be associated with a more favorable fetal acid base status than ephedrine; however, overall fetal outcomes appear to be similar. Nausea or vomiting may be less with phenylephrine than ephedrine but is also dependent upon blood pressure control. Phenylephrine may be preferred in the absence of maternal bradycardia.
Patient Education
What is this drug used for?
All oral products:
- It is used to treat nose stuffiness.
Injection:
- It is used to treat low blood pressure.
Frequently reported side effects of this drug
- Trouble sleeping
- Agitation
- Nausea
- Vomiting
- Sweating a lot
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Chest pain
- Fast heartbeat
- Passing out
- Abnormal heartbeat
- Severe dizziness
- Severe headache
- Vision changes
- Severe anxiety
- Tremors
- Blurred vision
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Slow heartbeat
- Burning or numbness of hands or feet
- Severe injection site pain, burning, edema, or irritation
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.