Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
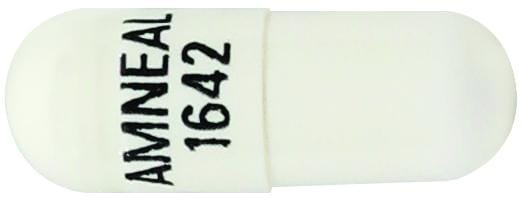
Capsule, Oral:
Esbriet: 267 mg
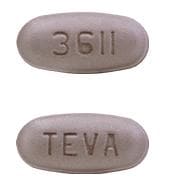
Tablet, Oral:
Esbriet: 267 mg, 801 mg
Pharmacology
Mechanism of Action
Precise mechanisms of action have not been fully elucidated; however, pirfenidone may exert antifibrotic properties by decreasing fibroblast proliferation and the production of fibrosis-associated proteins and cytokines; may decrease the formation and accumulation of extracellular matrix (ie, collagen) in response to transforming growth factor-beta and platelet derived growth factor. Pirfenidone is also believed to exert anti-inflammatory properties by decreasing the accumulation of inflammatory cells resulting from a variety of stimuli.
Pharmacokinetics/Pharmacodynamics
Distribution
~59 to 71 L
Metabolism
Hepatic primarily via CYP1A2 and to a lesser extent via CYP2C9, 2C19, 2D6, and 2E1; major metabolite (5-carboxy-pirfenidone) is inactive
Excretion
Urine (~80%; >99% as metabolite)
Time to Peak
Plasma: Median: 0.5 hours (fasting); 3 hours (with food)
Half-Life Elimination
~3 hours
Protein Binding
Mean: 58% (primarily to albumin)
Use in Specific Populations
Special Populations: Renal Function Impairment
Systemic exposure (AUC0 to ∞) increased ~1.4, 1.5, and 1.2-fold in mild, moderate, and severe renal impairment, respectively. The corresponding AUC0 to ∞ of 5-carboxy-pirfenidone increased 1.7, 3.4, and 5.6-fold. The renal clearance of 5-carboxy-pirfenidone decreased significantly in patients with moderate to severe impairment.
Special Populations: Hepatic Function Impairment
In patients with moderate impairment (Child Pugh class B), mean exposure, AUC0 to ∞ and Cmax increased ~1.6- and ~1.4-fold in moderate hepatic impairment, respectively.
Use: Labeled Indications
Idiopathic pulmonary fibrosis: Treatment of idiopathic pulmonary fibrosis (IPF)
Contraindications
There are no contraindications listed in the manufacturer’s labeling.
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to pirfenidone or any component of the formulation; history of angioedema with pirfenidone; concomitant use of fluvoxamine; severe hepatic impairment or end-stage liver disease; severe renal impairment (CrCl <30 mL/minute) or end-stage renal disease (ESRD) requiring dialysis.
Dosage and Administration
Dosing: Adult
Idiopathic pulmonary fibrosis (IPF): Oral:
Days 1 to 7: 267 mg 3 times daily (total dose: 801 mg/day)
Days 8 to 14: 534 mg 3 times daily (total dose: 1,602 mg/day)
Day 15 and thereafter: 801 mg 3 times daily (total dose: 2,403 mg/day). Maximum dose: 2,403 mg/day.
Reinitiation of therapy following interruption: If interruption <14 consecutive days, may reinitiate therapy at previous daily dose without retitration; if interruption ≥14 consecutive days, reinitiate therapy with the initial 2-week titration period up to recommended daily dose.
Dosage adjustment for concomitant therapy:
Strong CYP1A2 inhibitors (eg, fluvoxamine): Reduce pirfenidone to 267 mg 3 times daily (total dose: 801 mg/day).
Moderate CYP1A2 inhibitors (eg, ciprofloxacin): Reduce pirfenidone to 534 mg 3 times daily (total dose: 1,602 mg/day) when used concomitantly with ciprofloxacin 1,500 mg/day
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Gastrointestinal (eg, nausea, diarrhea, dyspepsia, vomiting): There are no specific dosage adjustments provided in the manufacturer’s labeling; however, consider temporary dosage reduction and/or therapy interruption to allow for resolution of symptoms.
Photosensitivity reaction or rash: There is no specific dosage adjustment provided in the manufacturer’s labeling; however, consider temporary dosage reduction and/or therapy interruption to allow for resolution of symptoms.
Administration
Oral: Administer with food at the same time each day.
Dietary Considerations
Take with food to decrease frequency of dizziness or nausea. Limit or avoid grapefruit juice.
Storage
Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F).
Pirfenidone Images
Drug Interactions
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Broccoli: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Cannabis: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Ciprofloxacin (Systemic): May increase the serum concentration of Pirfenidone. Management: With ciprofloxacin doses of 1,500 mg/day, the pirfenidone dose should be reduced to 1,602 mg per (534 mg three times a day). With lower daily doses of ciprofloxacin, use pirfenidone with caution. Consider therapy modification
CYP1A2 Inducers (Moderate): May decrease the serum concentration of Pirfenidone. Monitor therapy
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of Pirfenidone. Management: Avoid concomitant use of pirfenidone and moderate CYP1A2 inhibitors whenever possible. If combined, decrease the pirfenidone dose to 1,602 mg per day (534 mg three times daily) and monitor for increased pirfenidone toxicities. Exceptions: Ciprofloxacin (Systemic). Consider therapy modification
CYP1A2 Inhibitors (Strong): May increase the serum concentration of Pirfenidone. Management: Avoid concomitant use of pirfenidone and strong CYP1A2 inhibitors whenever possible. If combined, decrease the pirfenidone dose to 801 mg per day (267 mg three times daily) and monitor for increased pirfenidone toxicities. Consider therapy modification
Grapefruit Juice: May increase the serum concentration of Pirfenidone. Management: Consider advising patients to limit or avoid grapefruit juice consumption during treatment with pirfenidone. Canadian product labeling states that grapefruit juice should be avoided during pirfenidone treatment. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Tobacco (Smoked): May decrease the serum concentration of Pirfenidone. Avoid combination
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Fatigue (26%), headache (22%), dizziness (18%)
Dermatologic: Skin rash (30%)
Gastrointestinal: Nausea (36%), diarrhea (26%), abdominal pain (24%), dyspepsia (19%), anorexia (13%), vomiting (13%), gastroesophageal reflux disease (11%)
Respiratory: Upper respiratory tract infection (27%), sinusitis (11%)
1% to 10%:
Central nervous system: Insomnia (10%), noncardiac chest pain (5%)
Dermatologic: Skin photosensitivity (9%), pruritus (8%)
Endocrine & metabolic: Weight loss (10%)
Gastrointestinal: Decreased appetite (8%), dysgeusia (6%)
Hepatic: Increased serum transaminases (ALT and AST; ≥3 x ULN: 4%)
Neuromuscular & skeletal: Arthralgia (10%), asthenia (6%)
Postmarketing: Agranulocytosis, angioedema, hepatotoxicity
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: May cause dizziness and/or fatigue which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving). Incidence of dizziness may be reduced by administering with food. Dose reduction or discontinuation may be necessary if symptoms fail to improve or worsen.
- GI effects: Adverse effects including nausea/vomiting, diarrhea, dyspepsia, gastroesophageal reflux disease, and abdominal pain have been reported; incidence may be reduced by administering with food. The incidence of gastrointestinal events was highest early in the course of treatment (initial 3 months) and decreased over time. Consider dose reduction or discontinuation of therapy if lack of improvement or worsening of symptoms.
- Hepatic effects: Serious and nonserious cases of drug-induced liver injury (including severe liver injury with fatal outcome) have been reported. Elevations of ALT and AST were reversible with dose modification or discontinuation of therapy. Obtain LFTs (ALT, AST, bilirubin) prior to initiation of treatment, monthly during the first 6 months, then every 3 months thereafter, and as clinically indicated. Dosage modification or interruption of therapy may be necessary for elevated LFTs.
- Photosensitivity: Photosensitivity reactions and rash have been reported with the majority of reactions occurring during the initial 6 months of therapy (severe reactions are uncommon); instruct patients to avoid or minimize exposure to the sun and/or sun lamps, to apply sunscreen (SPF ≥50 against UVA and UVB), wear protective clothing/hats, and to avoid concurrent use of other photosensitizing drugs. Patients should promptly report symptoms, reaction, or rash; dose reduction or therapy interruption may be necessary. If appropriate, may reinitiate therapy with re-escalation of dose as tolerated.
- Weight loss: Weight loss/anorexia have been reported with use; monitor weight during therapy.
Disease-related concerns:
- Hepatic impairment: Use with caution in mild to moderate impairment (Child-Pugh class A and B); pirfenidone systemic exposure increased by 60% in moderate impairment. Use in severe impairment (Child-Pugh class C) is not recommended (has not been studied).
- Renal impairment: Use with caution in patients with renal impairment; consider dose reduction and/or discontinuation as necessary; use in patients with end stage renal disease requiring dialysis is not recommended.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Cigarette smokers: Clearance may be increased and systemic exposure decreased in cigarette smokers due to hepatic enzyme (ie, CYP1A2) induction. Patients should be instructed to quit smoking prior to initiation of therapy; cigarette smoking should be avoided during therapy.
Monitoring Parameters
Hepatic function (prior to initiation, monthly for first 6 months, then every 3 months thereafter and as clinically indicated); signs of photosensitivity; gastrointestinal events (eg, diarrhea, nausea, vomiting); weight loss.
Pregnancy
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat idiopathic pulmonary fibrosis.
Frequently reported side effects of this drug
- Dizziness
- Fatigue
- Heartburn
- Common cold symptoms
- Joint pain
- Lack of appetite
- Diarrhea
- Nausea
- Vomiting
- Change in taste
- Loss of strength and energy
- Trouble sleeping
- Headache
- Abdominal pain
- Weight loss
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Chest pain
- Severe diarrhea
- Severe nausea
- Vomiting
- Severe abdominal pain
- Sunburn
- Bleeding
- Bruising
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.