Boxed Warning
Bleeding risk:
Prasugrel can cause significant, sometimes fatal, bleeding. Do not use prasugrel in patients with active pathological bleeding or a history of transient ischemic attack (TIA) or stroke.
In patients ≥75 years, prasugrel is generally not recommended because of the increased risk of fatal and intracranial bleeding and uncertain benefit, except in high-risk situations (patients with diabetes or a history of myocardial infarction [MI]) in which its effect appears to be greater and its use may be considered.
Do not start prasugrel in patients likely to undergo urgent coronary artery bypass graft (CABG) surgery. When possible, discontinue prasugrel at least 7 days prior to any surgery.
Additional risk factors for bleeding include body weight <60 kg, propensity to bleed, and concomitant use of medications that increase the risk of bleeding (eg, warfarin, heparin, fibrinolytic therapy, long-term use of nonsteroidal anti-inflammatory drugs [NSAIDs]).
Suspect bleeding in any patient who is hypotensive and has recently undergone coronary angiography, percutaneous coronary intervention (PCI), CABG, or other surgical procedures in the setting of prasugrel.
If possible, manage bleeding without discontinuing prasugrel. Discontinuing prasugrel, particularly in the first few weeks after acute coronary syndrome (ACS), increases the risk of subsequent cardiovascular events.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
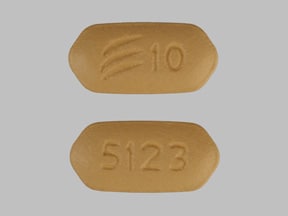
Tablet, Oral:
Effient: 5 mg, 10 mg
Generic: 5 mg, 10 mg
Pharmacology
Mechanism of Action
Prasugrel, an inhibitor of platelet activation and aggregation, is a prodrug that is metabolized to both active (R-138727) and inactive metabolites. The active metabolite irreversibly blocks the P2Y12 component of ADP receptors on the platelet, which prevents activation of the GPIIb/IIIa receptor complex, thereby reducing platelet activation and aggregation
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid; ≥79%
Distribution
Active metabolite: Vd: 44-68 L
Metabolism
Rapid intestinal and serum metabolism via esterase-mediated hydrolysis to a thiolactone intermediate (inactive), which is then converted, via CYP450-mediated (primarily CYP3A4 and CYP2B6) oxidation, to an active metabolite (R-138727) (Farid, 2007; Riley, 2008)
Excretion
Urine (~68% inactive metabolites); feces (27% inactive metabolites)
Onset of Action
Inhibition of platelet aggregation (IPA): Dose dependent: 60 mg loading dose: <30 minutes; median time to reach ≥20% IPA: 30 minutes (Brandt, 2007)
Peak effect: Time to maximal IPA: Dose-dependent: Note: Degree of IPA based on adenosine diphosphate (ADP) concentration used during light aggregometry: 60 mg loading dose: Occurs ~4 hours post administration; Mean IPA (ADP 5 micromol/L): ~84.1%; Mean IPA (ADP 20 micromole/L): ~78.8% (Brandt, 2007)
Time to Peak
Active metabolite: ~30 minutes; With high-fat/high-calorie meal: 1.5 hours
Duration of Action
Duration of effect: Platelet aggregation gradually returns to baseline values over 5-9 days after discontinuation; reflective of new platelet production
Half-Life Elimination
Half-life elimination: Active metabolite: ~7 hours (range: 2-15 hours)
Protein Binding
Active metabolite: ~98%
Use in Specific Populations
Special Populations: Renal Function Impairment
In patients with ESRD, both Cmax and AUC0-t last of the active metabolite were approximately half that in healthy patients and in patients with moderate renal impairment.
Special Populations: Elderly
The AUC of active metabolite was 19% higher in patients 75 years and older than in patients younger than 75 years.
Special Populations: Race
The AUC of active metabolite was approximately 19% higher in Chinese, Japanese, and Korean subjects than in white subjects.
Special Populations Note
Body weight: The AUC of the active metabolite is approximately 30% to 40% higher in subjects with a body weight of less than 60 kg compared to those weighing 60 kg or more.
Use: Labeled Indications
Acute coronary syndrome to be managed with percutaneous coronary intervention (PCI): To reduce the rate of thrombotic cardiovascular events (including stent thrombosis) in patients with acute coronary syndrome (ACS) who are to be managed with PCI for unstable angina (UA), non-ST-segment elevation MI (NSTEMI), or ST-elevation MI (STEMI).
Contraindications
Hypersensitivity (eg, anaphylaxis) to prasugrel or any component of the formulation; active pathological bleeding (eg, peptic ulcer, intracranial hemorrhage); prior transient ischemic attack or stroke.
Canadian labeling: Additional contraindications (not in US labeling): Severe hepatic impairment (Child-Pugh Class C).
Dosage and Administration
Dosing: Adult
Acute coronary syndrome (ACS): Oral:
Percutaneous coronary intervention (PCI) for ACS: Loading dose: 60 mg administered promptly (as soon as coronary anatomy is known) and no later than 1 hour after PCI; Maintenance dose: 10 mg once daily (in combination with aspirin) (ACCF/AHA [O’Gara, 2013]; AHA/ACC [Amsterdam 2014]; Levine 2011). For patients with STEMI, a loading dose may also be administered if PCI is performed >24 hours after treatment with a fibrin-specific thrombolytic (ie, alteplase, reteplase, tenecteplase) (ACCF/AHA [O’Gara, 2013]).
Maintenance dosing in low body weight (ie, <60 kg) individuals: Due to a higher incidence of bleeding in patients weighing <60 kg, a maintenance dose of 5 mg once daily may be considered. In aspirin-treated patients weighing <60 kg (mean: 56.4 ± 3.7 kg) with stable coronary artery disease, the use of prasugrel 5 mg once daily was shown to reduce platelet reactivity to a similar extent as prasugrel 10 mg administered once daily to patients >60 kg (mean: 84.7 ± 14.9 kg); clinical events were not evaluated (Erlinge 2012). In patients with ACS (medically managed) treated with aspirin, a 5 mg daily maintenance dose (after a 30 mg loading dose) in patients <60 kg did not demonstrate a significant difference in the composite primary end point of death from cardiovascular causes, MI, or stroke compared to patients >60 kg treated with a 10 mg maintenance dose; bleeding risk was not increased (Roe 2012).
Duration of prasugrel (in combination with aspirin) after stent placement: Premature interruption of therapy may result in stent thrombosis, MI, and death. According to the ACC/AHA Duration of Dual Antiplatelet Therapy (DAPT) guidelines, at least 12 months of a P2Y12 inhibitor (eg, prasugrel) is recommended for those with ACS receiving either stent type (bare metal [BMS] or drug eluting stent [DES]). The DAPT score may be useful in determining whether to prolong or extend DAPT in patients with stent placement (Yeh 2016). In addition, in patients with DES placement with a high risk of bleeding or significant overt bleeding on DAPT, it may be reasonable to discontinue prasugrel after 6 months of therapy instead (ACC/AHA [Levine 2016]).
Conversion from clopidogrel to prasugrel: Beginning 24 hours after the last clopidogrel dose (loading or maintenance), may initiate prasugrel 10 mg once daily or a 60 mg loading dose followed in 24 hours with 10 mg once daily (Angiolillo 2010; Payne 2008; Wiviott 2007).
Dosing: Geriatric
Refer to adult dosing. Patients ≥75 years: Use not recommended; may be considered in high-risk situations (eg, patients with diabetes or history of MI).
Administration
Administer without regard to meals. In an emergent primary PCI setting, crushing the tablets (using a commercially available syringe crusher) and mixing with 25 mL of water led to faster absorption and a quicker, more potent antiplatelet effect seen as early as 30 minutes (Rollini 2016). In addition, according to the manufacturer, tablets may be chewed and swallowed (bitter to taste) or crushed and mixed in food or liquid (eg, applesauce, juice, water) and immediately administered by mouth or gastric tube. Administration via an enteral tube that bypasses the acidic environment of the stomach may result in reduced bioavailability of prasugrel (data on file, Daiichi Sankyo-Lilly 2012).
Storage
Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Store and dispense in original container; do not remove desiccant.
Prasugrel Images
Drug Interactions
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Apixaban: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Consider therapy modification
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Cangrelor: May diminish the antiplatelet effect of Prasugrel. More specifically, while the use of Cangrelor is expected to increase total platelet inhibition in patients who have previously received Prasugrel, Cangrelor is expected to decrease binding of Prasugrel metabolites to P2Y12 receptors and thus reduce the extent of irreversible platelet inhibition. Management: Avoid administration of prasugrel until cangrelor is discontinued. Consider therapy modification
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Dabigatran Etexilate: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Dabigatran Etexilate. Specifically, the risk of bleeding may be increased. Antiplatelet Agents (P2Y12 Inhibitors) may increase the serum concentration of Dabigatran Etexilate. Specifically, clopidogrel may increase dabigatran serum concentrations. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Consider therapy modification
Dasatinib: May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Edoxaban: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider the anticipated risks and benefits of this combination. If combined, increased monitoring for bleeding is recommended. Consider therapy modification
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
FentaNYL: May diminish the antiplatelet effect of Antiplatelet Agents (P2Y12 Inhibitors). FentaNYL may decrease the serum concentration of Antiplatelet Agents (P2Y12 Inhibitors). Monitor therapy
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Heparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or agents with antiplatelet properties if coadministration is required. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Morphine (Systemic): May diminish the antiplatelet effect of Antiplatelet Agents (P2Y12 Inhibitors). Morphine (Systemic) may decrease the serum concentration of Antiplatelet Agents (P2Y12 Inhibitors). Management: Consider alternative anti-ischemic/analgesic therapies (eg, beta-blockers, nitroglycerin) in patients with acute coronary syndromes treated with a P2Y12 inhibitor when possible. The risks associated with other opioids are unknown. Consider therapy modification
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
RaNITIdine: May decrease serum concentrations of the active metabolite(s) of Prasugrel. Monitor therapy
RifAMPin: May diminish the antiplatelet effect of Prasugrel. Monitor therapy
Rivaroxaban: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Consider therapy modification
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Adverse Reactions
1% to 10%:
Cardiovascular: Hypertension (8%), hypotension (4%), atrial fibrillation (3%), bradycardia (3%), peripheral edema (3%)
Central nervous system: Headache (6%), dizziness (4%), fatigue (4%), noncardiac chest pain (3%)
Dermatologic: Skin rash (3%)
Endocrine & metabolic: Hypercholesterolemia (≤7%), hyperlipidemia (≤7%)
Gastrointestinal: Nausea (5%), diarrhea (2%), gastrointestinal hemorrhage (2%)
Hematologic & oncologic: Leukopenia (3%), anemia (2%), major hemorrhage (2%), minor hemorrhage (2%), major hemmorhage (life-threatening: 1%)
Neuromuscular & skeletal: Back pain (5%), limb pain (3%)
Respiratory: Epistaxis (6%), dyspnea (5%), cough (4%)
Miscellaneous: Fever (3%)
<1%, postmarketing, and/or case reports: Abnormal hepatic function tests, anaphylaxis, angioedema, hematoma, hemoptysis, hemorrhage (requiring inotropes or transfusion), hypersensitivity reaction, intracranial hemorrhage (symptomatic), re-operation due to bleeding, thrombocytopenia, thrombotic thrombocytopenic purpura
Warnings/Precautions
Concerns related to adverse effects:
- Bleeding: [US Boxed Warning]: May cause significant, sometimes fatal, bleeding. Do not use prasugrel in patients with active pathological bleeding or a history of TIA or stroke. Additional risk factors for bleeding include body weight <60 kg, propensity to bleed (eg, recent trauma, recent surgery, recent or recurrent GI bleeding, active peptic ulcer disease, severe hepatic impairment, or moderate to severe renal impairment), and concomitant use of medications that increase the risk of bleeding (eg, warfarin, heparin, fibrinolytic therapy, long-term use of NSAIDs). Suspect bleeding in any patient who is hypotensive and has recently undergone coronary angiography, PCI, CABG, or other surgical procedures in the setting of prasugrel. If possible, manage bleeding without discontinuing prasugrel. Discontinuing prasugrel, particularly in the first few weeks after ACS, increases the risk of subsequent cardiovascular events. Management of bleeding episodes includes the use of PRBCs and platelet transfusion.
- Hypersensitivity: Hypersensitivity, including angioedema, has been reported, including in patients with a previous history of thienopyridine hypersensitivity. Because of structural similarities, cross-reactivity is possible among the thienopyridines (clopidogrel, prasugrel, and ticlopidine); use with caution or avoid in patients with previous history of thienopyridine hypersensitivity. Use of prasugrel is contraindicated in patients with hypersensitivity (eg, anaphylaxis) to prasugrel.
- Thrombotic thrombocytopenic purpura (TTP): Cases of TTP (usually occurring within the first 2 weeks of therapy), resulting in some fatalities, have been reported with prasugrel; urgent plasmapheresis is required.
Disease-related concerns:
- GI disease: Use with caution in patients with recent or recurrent GI bleeding or active peptic ulcer disease (patients are generally at higher risk of bleeding).
- Hepatic impairment: Use with caution in patients with severe hepatic impairment (patients are generally at higher risk of bleeding).
- Renal impairment: Use with caution in patients with moderate to severe renal impairment (patients are generally at higher risk of bleeding).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: [US Boxed Warning]: In patients ≥75 years, use is generally not recommended due to increased risk of fatal and intracranial bleeding and uncertain benefit, except in high-risk situations (patients with diabetes or a history of MI) in which its effect appears to be greater and its use may be considered.
- Lower GI bleed patients: An individualized and multidisciplinary approach should be utilized to determine therapy discontinuation and management in patients with acute lower GI bleed (LGIB) who are on antiplatelet medications; risk of ongoing bleeding should be weighed with risk of thromboembolic events. In patients receiving dual antiplatelet therapy (aspirin plus P2Y12 receptor blocker [eg, clopidogrel, prasugrel, ticagrelor, ticlopidine]) or thienopyridine monotherapy, the thienopyridine should generally be resumed as soon as possible and at least within 7 days, taking into account control of bleeding and cardiovascular risk (aspirin should not be discontinued); however, dual antiplatelet therapy should not be discontinued in the 90 days post-acute coronary syndrome or 30 days post-coronary stenting (Strate 2016).
- Low-weight patients: In patients weighing <60 kg, risk of bleeding increased; consider lower maintenance dose.
- Surgical patients: [US Boxed Warning]: Do not initiate therapy in patients likely to undergo urgent CABG surgery; when possible, discontinue ≥7 days prior to any surgery; increased risk of bleeding. The American College of Chest Physicians (ACCP) recommends discontinuing prasugrel 5 days before surgery (Guyatt 2012). When urgent CABG is necessary, the ACCF/AHA suggests that it may be reasonable to perform surgery within 7 days of discontinuing prasugrel especially if the benefits of prompt revascularization outweigh the risks of bleeding (ACCF/AHA [Hillis 2011]; ACCF/AHA [O’Gara 2013]). Elective noncardiac surgery should not be performed in patients in whom dual antiplatelet therapy (DAPT) will need to be discontinued perioperatively within 30 days following bare metal stent (BMS) placement or within 12 months after drug-eluting stent (DES) placement. In patients undergoing urgent noncardiac surgery during the first 4 to 6 weeks after BMS or DES placement, continue DAPT. In patients with stents undergoing surgery that requires discontinuation of the P2Y12 inhibitor (eg, clopidogrel), continue aspirin and re-start the P2Y12 inhibitor as soon as possible after surgery (ACC/AHA [Fleisher 2014]).
Other warnings/precautions:
- Drug discontinuation: Discontinue therapy for active bleeding, elective surgery, stroke, or TIA; reinitiate therapy as soon as possible unless patient suffers stroke or TIA where subsequent use is contraindicated; if possible, manage bleeding without discontinuing therapy since premature discontinuation of treatment may cause increased risk for cardiac adverse events; lapses in treatment should be avoided.
Monitoring Parameters
Hemoglobin and hematocrit periodically.
Pregnancy
Pregnancy Considerations
Adverse events have not been observed in animal reproduction studies. Information related to use during pregnancy is limited (Tello-Montoliu 2013).
Patient Education
What is this drug used for?
- It is used to lower the chance of heart attack, the need for some heart treatments, or blockage of a stent after a stent is placed in the heart.
Frequently reported side effects of this drug
- Back pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Difficulty swallowing
- Chest pain
- Dizziness
- Passing out
- Severe headache
- Purple patches on skin or mouth
- Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome like bruising or bleeding; loss of strength and energy; dark urine or yellow skin; pale skin; change in amount of urine passed; vision changes; change in strength on one side is greater than the other, difficulty speaking or thinking, or change in balance; or fever.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.