Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Minipress: 1 mg, 2 mg, 5 mg
Generic: 1 mg, 2 mg, 5 mg
Pharmacology
Mechanism of Action
Competitively inhibits postsynaptic alpha-adrenergic receptors which results in vasodilation of veins and arterioles and a decrease in total peripheral resistance and blood pressure
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: 0.5 L/kg
Metabolism
Extensively hepatic via demethylation and conjugation
Excretion
Feces; urine (6% to 10% as unchanged drug)
Onset of Action
Antihypertensive: Within 2 hours; Peak effect: 2 to 4 hours
Time to Peak
Plasma: ~3 hours
Duration of Action
10 to 24 hours
Half-Life Elimination
2 to 3 hours, prolonged with CHF
Protein Binding
Highly bound (97%)
Use: Labeled Indications
Hypertension: Management of hypertension. Note: Alpha blockers are not recommended as first line therapy (ACC/AHA [Whelton 2017]).
Use: Off Label
Posttraumatic stress disorder related nightmares and sleep disruptionbyes
Data from a meta-analysis of six randomized-controlled trials, supports the use of prazosin in reducing trauma nightmares and improving overall posttraumatic stress disorder (PTSD) symptoms including hyperarousal, total sleep time, and sleep quality in both veteran combat related and civilian noncombat related chronic PTSD Singh 2016.
Based on the American Psychiatric Association practice guidelines for the treatment of acute stress disorder and posttraumatic stress disorder and American Academy of Sleep Medicine position paper for the treatment of nightmare disorders in adults, prazosin appears effective for the management of trauma-related nightmares and sleep disruption associated with PTSD. Similarly, based on the World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the treatment of anxiety, obsessive-compulsive and post-traumatic stress disorder, prazosin may reduce nightmares and be an alternative therapy for treatment-resistant cases. In contrast, the Veterans Affairs/Department of Defense clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder suggests against the use of prazosin for global symptoms of PTSD and does not make a recommendation for or against use for nightmares associated with PTSD, based on inconsistent and insufficient clinical trials evidence, respectively. The guidelines do not recommend for or against continuation of prazosin in patients who find benefit and recommend that decisions to stop or continue therapy be individualized.
Raynaud phenomenonc
Data from a limited number of patients in four double-blind, placebo-controlled trials and an open-label dose response trial suggest that prazosin may be beneficial for the treatment of Raynaud phenomenon Nielson 1983, Russell 1985, Surwit 1984, Wollersheim 1988, Wollersheim 1986.
Contraindications
Known sensitivity to quinazolines, prazosin, or any component of the formulation
Dosage and Administration
Dosing: Adult
Hypertension (alternative agent): Oral: Initial: 1 mg 2 or 3 times daily, titrate as needed based on patient response up to a dose of 20 mg daily in 2 or 3 divided doses (ACC/AHA [Whelton 2017]). Some patients may benefit from up to 40 mg/day in divided doses.
Concomitant diuretics or other antihypertensives: When adding a diuretic or other antihypertensive, decrease prazosin dose to 1 or 2 mg 3 times daily and retitrate.
PTSD-related nightmares and sleep disruption (off-label use): Oral: Initial: 1 mg at bedtime; after 2 to 3 days increase dose to 2 mg at bedtime, then adjust dosage based on response and tolerability in 1 to 5 mg increments every 7 days up to a maximum of 15 mg/day. Titration as rapid as every 2 to 3 days has been evaluated (Singh 2016). Usual dose range: 3 to 15 mg at bedtime (APA [Benedek 2009]). Civilian patients, especially females, may require lower doses (Taylor 2008).
Raynaud phenomenon (off-label use): Oral: Initial: 0.5 to 1 mg once daily (at bedtime) or 0.5 mg twice daily; gradually adjust dose based on response and tolerability up 12 mg/day in 2 to 3 divided doses (Nielson 1983; Russell 1985; Wollersheim 1988)
Dosing: Geriatric
Avoid use for hypertension treatment (Beers Criteria [AGS 2019]). Refer to adult dosing for other indications.
Dosing: Pediatric
Hypertension: Limited data available: Note: Not recommended first-line therapy; reserve for patients not responsive to therapeutic trials of 2 or more preferred agents (eg, ACE inhibitor, ARB, calcium channel blocker, or thiazide diuretic) (AAP [Flynn 2017]). Children and Adolescents: Oral: Initial: 0.05 to 0.1 mg/kg/day in divided doses every 8 hours; may titrate up to 0.5 mg/kg/day in divided doses 3 times daily; maximum daily dose: 20 mg/day (NHBPEP 2004; NHLBI 2011)
Scorpion envenomation: Limited data available:
Weight-directed: Infants ≥4 months, Children, and Adolescents: Oral: 0.03 mg/kg/dose; second dose has been administered at 3 or 6 hours after initial dose; subsequent doses every 3 to 6 hours; therapy has been continued for 48 hours or until extremities are warm and dry (Bosnak 2009; Gupta 2010; Pandi 2014)
Fixed dosing: Infants >6 months, Children, and Adolescents: Oral: 0.25 mg every 3 hours until extremities are warm and dry (Bawaskar 2010)
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from moisture and light.
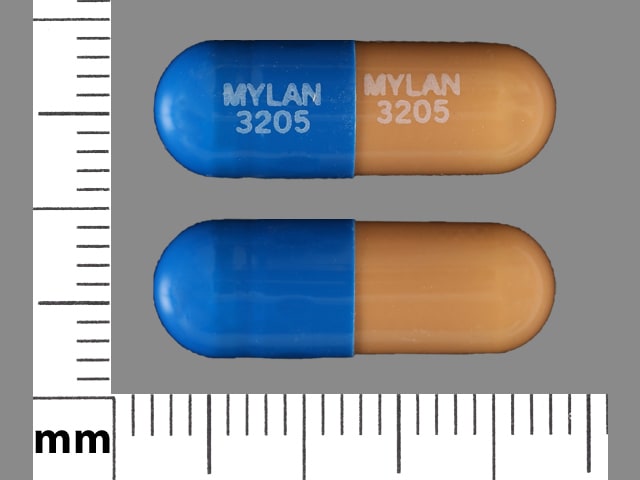
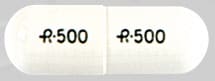
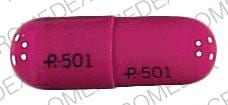
Prazosin Images
Drug Interactions
Alpha-/Beta-Agonists: Alpha1-Blockers may diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Similarly, Alpha-/Beta-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
Alpha1-Agonists: Alpha1-Blockers may diminish the vasoconstricting effect of Alpha1-Agonists. Similarly, Alpha1-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
Alpha1-Blockers: May enhance the antihypertensive effect of other Alpha1-Blockers. Avoid combination
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta-Blockers: May enhance the orthostatic hypotensive effect of Alpha1-Blockers. The risk associated with ophthalmic products is probably less than systemic products. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Calcium Channel Blockers: Alpha1-Blockers may enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Dapoxetine: May enhance the orthostatic hypotensive effect of Alpha1-Blockers. Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Alpha1-Blockers (Nonselective). Management: Ensure patient is stable on one agent prior to initiating the other, and always initiate combination using the lowest possible dose of the drug being added. When tadalafil is used for treatment of BPH, concurrent alpha 1-blockers are not recommended. Consider therapy modification
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Rilmenidine: Alpha1-Blockers may enhance the hypotensive effect of Rilmenidine. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
Increased urinary VMA 17%, norepinephrine metabolite 42%; therefore, false positives may occur in screening for pheochromocytoma. If elevated VMA is found, discontinue prazosin and retest after one month.
Adverse Reactions
>4%:
Cardiovascular: Palpitations (5%)
Central nervous system: Dizziness (10%), drowsiness (8%), headache (8%), fatigue (7%)
Gastrointestinal: Nausea (5%)
Neuromuscular & skeletal: Weakness (7%)
1% to 4%:
Cardiovascular: Edema, orthostatic hypotension, syncope
Central nervous system: Depression, nervousness, vertigo
Dermatologic: Skin rash
Gastrointestinal: Constipation, diarrhea, vomiting, xerostomia
Genitourinary: Urinary frequency
Ophthalmic: Blurred vision, injected sclera
Respiratory: Dyspnea, epistaxis, nasal congestion
<1%, postmarketing, and/or case reports: Abdominal distress, abnormal hepatic function tests, alopecia, angina pectoris, arthralgia, bradycardia, cataplexy, cataract (both development of cataract and disappearance have been reported), diaphoresis, eye pain, fever, flushing, gynecomastia, hallucination, hypersensitivity reaction, impotence, insomnia, leukopenia, lichen planus, malaise, myocardial infarction, narcolepsy (worsened), pain, pancreatitis, paresthesia, positive ANA titer, priapism, pruritus, retinal pigment changes (mottled), retinopathy (serous), systemic lupus erythematosus, tachycardia, tinnitus, urinary incontinence, urticaria, vasculitis
Warnings/Precautions
Concerns related to adverse effects:
- Angina: Discontinue if symptoms of angina occur or worsen.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Floppy iris syndrome: Intraoperative floppy iris syndrome has been observed in cataract surgery patients who were on or were previously treated with alpha1-blockers; modification to surgical technique may be necessary. There appears to be no benefit in discontinuing alpha1-blockers prior to surgery.
- Orthostatic hypotension/syncope: May cause significant orthostatic hypotension and syncope with sudden loss of consciousness, especially within 30 to 90 minutes of the first dose; anticipate a similar effect if therapy is interrupted for a few days, if dosage is rapidly increased, or if another antihypertensive drug (particularly vasodilators or a beta-blocker) or a phosphodiesterase 5 (PDE 5) inhibitor (eg, sildenafil, tadalafil, vardenafil) is introduced. Severe tachycardia (120 to 160 beats/minute) has occasionally been reported prior to a syncopal episode. Patients should be cautioned about alcohol use and performing hazardous tasks when starting new therapy or adjusting dosage upward.
- Priapism: Priapism and prolonged erections have been reported; seek immediate medical assistance for erections lasting longer than 4 hours.
Disease-related concerns:
- Heart failure: In a scientific statement from the American Heart Association, prazosin has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: moderate) (AHA [Page 2016]).
- Prostate cancer: Should rule out prostatic carcinoma before beginning therapy.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
Blood pressure, standing and sitting/supine
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year ASCVD risk ≥10%: Target blood pressure <130/80 mm Hg is recommended
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable
Pregnancy
Pregnancy Considerations
Prazosin crosses the placenta and its pharmacokinetics may be slightly altered during pregnancy (Bourget 1995; Rubin 1983); bioavailability was increased, time to peak serum concentration, and elimination rates were longer in women during the third trimester (Rubin 1983). Limited use in pregnant women has not demonstrated any fetal abnormalities or adverse effects (maternal treatment started after the first trimester) (Dommisse 1983; Lubbe 1981).
Chronic maternal hypertension may increase the risk of birth defects, low birth weight, preterm delivery, stillbirth, and neonatal death. Actual fetal/neonatal risks may be related to duration and severity of maternal hypertension. Untreated hypertension may also increase the risks of adverse maternal outcomes, including gestational diabetes, myocardial infarction, preeclampsia, stroke, and delivery complications (ACOG 203 2019).
Agents other than prazosin are more commonly used to treat hypertension in pregnancy (ACOG 203 2019; ESC [Regitz-Zagrosek 2018]); use of prazosin should be considered in consult with subspecialists (ACOG 203 2019). Females with preexisting hypertension may continue their medication during pregnancy unless contraindications exist (ESC [Regitz-Zagrosek 2018]). Although rare, use of prazosin for the treatment of hypertension due to a pheochromocytoma during pregnancy has been described (Mazza 2014).
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Fatigue
- Loss of strength and energy
- Headache
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Blurred vision
- Fast heartbeat
- Arrhythmia
- Depression
- Shortness of breath
- Erection that lasts more than 4 hours
- Swelling of arms or legs
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.