Boxed Warning
Mortality:
In the National Heart, Lung, and Blood Institute's Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multicenter, randomized, double-blind study in patients with asymptomatic non–life-threatening ventricular arrhythmias who had a myocardial infarction (MI) more than 6 days but less than 2 years previously, an increased rate of death or reversed cardiac arrest rate (7.7%) was seen in patients treated with encainide or flecainide (class IC antiarrhythmics) compared with that seen in patients assigned to placebo (3%). The average duration of treatment with encainide or flecainide in this study was 10 months.
The applicability of the CAST results to other populations (eg, those without recent MI) or other antiarrhythmic drugs is uncertain, but at present, it is prudent to consider any IC antiarrhythmic to have a significant risk in patients with structural heart disease. Given the lack of any evidence that these drugs improve survival, generally avoid antiarrhythmic agents in patients with non–life-threatening ventricular arrhythmias, even if the patients are experiencing unpleasant, but not life-threatening, symptoms or signs.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule Extended Release 12 Hour, Oral, as hydrochloride:
Rythmol SR: 225 mg, 325 mg, 425 mg [contains soybean lecithin]
Generic: 225 mg, 325 mg, 425 mg
Tablet, Oral, as hydrochloride:
Rythmol: 150 mg [DSC], 225 mg [DSC]
Generic: 150 mg, 225 mg, 300 mg
Pharmacology
Mechanism of Action
Propafenone is a class 1c antiarrhythmic agent which possesses local anesthetic properties, blocks the fast inward sodium current, and slows the rate of increase of the action potential. Prolongs conduction and refractoriness in all areas of the myocardium, with a slightly more pronounced effect on intraventricular conduction; it prolongs effective refractory period, reduces spontaneous automaticity and exhibits some beta-blockade activity.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Distribution
Vd: Adults: 252 L
Metabolism
Hepatic via CYP2D6, CYP3A4 and CYP1A2 to two active metabolites (5-hydroxypropafenone and N-depropylpropafenone) then ultimately to glucuronide or sulfate conjugates. Two genetically determined metabolism groups exist (extensive and poor metabolizers); 10% of Caucasians are poor metabolizers. Exhibits nonlinear pharmacokinetics; when dose is increased from 300-900 mg/day, serum concentrations increase tenfold; this nonlinearity is thought to be due to saturable first-pass effect.
Excretion
Urine (<1% unchanged; remainder as glucuronide or sulfate conjugates); feces
Time to Peak
Serum: IR: 3.5 hours; ER: 3-8 hours
Half-Life Elimination
Extensive metabolizers: 2-10 hours; Poor metabolizers: 10-32 hours
Protein Binding
95% to alpha1-acid glycoprotein
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Cl is reduced and elimination half-life is increased.
Use: Labeled Indications
Treatment of life-threatening ventricular arrhythmias; to prolong the time to recurrence of paroxysmal atrial fibrillation/flutter (PAF) or paroxysmal supraventricular tachycardia (PSVT) in patients with disabling symptoms without structural heart disease
Guideline recommendations: Due to safety risks, propafenone should be reserved for use in patients without structural or ischemic heart disease who are not candidates for, or prefer not to undergo catheter ablation and in whom other therapies have failed or are contraindicated (ACC/AHA/HRS [Page 2015]; AHA/ACC/HRS [Al-Khatib 2017]).
Extended-release capsule: Prolong the time to recurrence of symptomatic atrial fibrillation in patients without structural heart disease
Use: Off Label
Paroxysmal atrial fibrillation (pharmacological cardioversion)byes
Data from an open-label clinical trial investigating the feasibility and safety of a pill-in-the-pocket approach to treating paroxysmal atrial fibrillation supports the use of immediate release propafenone to reduce emergency room visits and hospitalizations of patients with recurrent atrial fibrillation (AF) Alboni 2004. Additional data may be necessary to further define the role of propafenone as a pill-in-the-pocket approach to pharmacologic cardioversion in the outpatient setting.
According to the 2014 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for the management of AF, propafenone may be used to convert atrial fibrillation/flutter to sinus rhythm. Immediate release propafenone (“pill-in-the-pocket”) in addition to a beta blocker or nondihydropyridine calcium channel blocker may also be used to terminate AF outside of the hospital when it is demonstrated to be safe in a monitored setting for selected patients.
Ventricular premature beatsyes
Based on the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death, propafenone is effective for suppressing premature ventricular contractions in patients without structural heart disease. Clinical experts recommend beta blockers as first line pharmacologic therapy due to a safer side effect profile Manolis 2018.
Contraindications
Hypersensitivity to propafenone or any component of the formulation; sinoatrial, atrioventricular, and intraventricular disorders of impulse generation or conduction (except in patients with a functioning artificial pacemaker); known Brugada syndrome; bradycardia; cardiogenic shock; heart failure; marked hypotension; bronchospastic disorders or severe obstructive pulmonary disease; marked electrolyte imbalance
Canadian labeling: Additional contraindications (not in US labeling): MI within past 3 months; severe hepatic impairment; myasthenia gravis; concurrent use with ritonavir
Dosage and Administration
Dosing: Adult
Note: Patients who exhibit significant widening of QRS complex or second- or third-degree AV block may need dose reduction.
Atrial fibrillation (to prevent recurrence): Oral:
Extended-release capsule: Initial: 225 mg every 12 hours; dosage increase may be made at a minimum of 5-day intervals; may increase to 325 mg every 12 hours; if further increase is necessary, may increase to 425 mg every 12 hours
Immediate-release tablet: Initial: 150 mg every 8 hours; dosage increase may be made at minimum of 3- to 4-day intervals, may increase to 225 mg every 8 hours; if further increase is necessary, may increase to 300 mg every 8 hours
Paroxysmal supraventricular tachycardia (to prevent recurrence): Oral:
Immediate-release tablet: Initial: 150 mg every 8 hours; dosage increase may be made at minimum of 3- to 4-day intervals, may increase to 225 mg every 8 hours; if further increase is necessary, may increase to 300 mg every 8 hours
Alternate recommendations:
Immediate-release tablet: Initial: 150 mg every 8 hours; maximum maintenance dose: 300 mg every 8 hours (ACC/AHA/HRS [Page 2015]).
Extended-release capsule: Initial: 225 mg every 12 hours; maximum maintenance dose: 425 mg every 12 hours (ACC/AHA/HRS [Page 2015]).
Paroxysmal atrial fibrillation, pharmacologic cardioversion (off-label use): Oral: Note: May be used on an outpatient basis (“Pill-in-the-pocket”). An initial inpatient cardioversion trial should have been successful before sending patient home on this approach. Patient must be taking an AV nodal-blocking agent (eg, beta-blocker, nondihydropyridine calcium channel blocker) prior to initiation of antiarrhythmic.
Immediate-release tablet: 450 mg (weight <70 kg), 600 mg (weight ≥70 kg). May not repeat in ≤24 hours (Alboni, 2004; AHA/ACC/HRS [January 2014]).
Ventricular arrhythmia: Oral:
Immediate-release tablet: 150 mg every 8 hours; dosage increase may be made at minimum of 3- to 4-day intervals, may increase to 225 mg every 8 hours; if further increase is necessary, may increase to 300 mg every 8 hours(AHA/ACC/HRS [Al-Khatib 2017])
Extended-release capsule (off-label dose): 225 to 425 mg every 12 hours (AHA/ACC/HRS [Al-Khatib 2017])
Ventricular premature beats (off-label use): Oral:
Immediate-release tablet: 150 to 300 mg every 8 hours(AHA/ACC/HRS [Al-Khatib 2017])
Extended-release capsule: 225 to 425 mg every 12 hours (AHA/ACC/HRS [Al-Khatib 2017])
Dosing: Geriatric
Refer to adult dosing.
Administration
Oral: Capsules should be swallowed whole; do not crush or chew; may be taken without regard to meals.
The Canadian labeling recommends the tablet be swallowed whole with liquid and to be administered with food.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
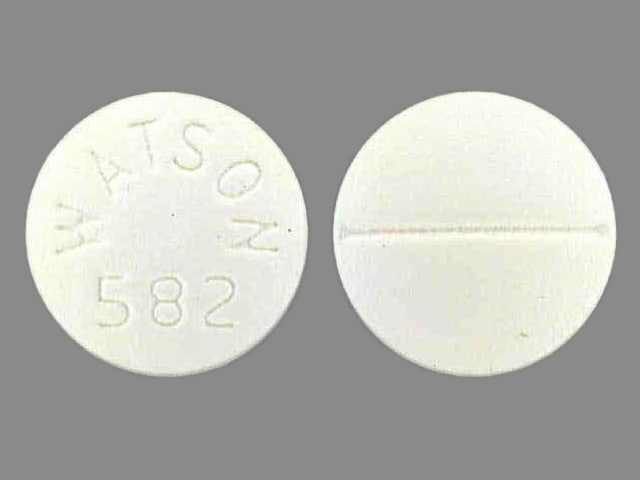
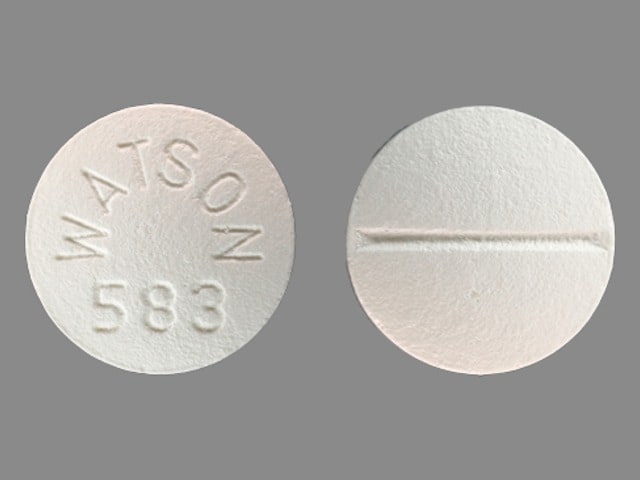
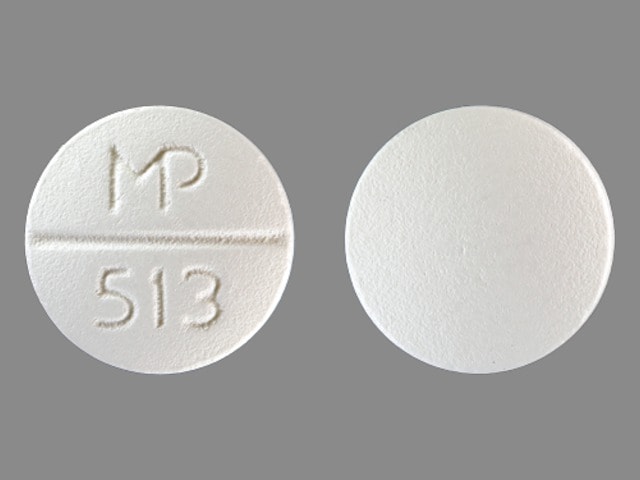
Propafenone Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Afatinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Afatinib. Management: Reduce afatinib by 10 mg if not tolerated. Some non-US labeling recommends avoiding combination if possible. If used, administer the P-gp inhibitor simultaneously with or after the dose of afatinib. Consider therapy modification
Amiodarone: May enhance the QTc-prolonging effect of Propafenone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Antihepaciviral Combination Products: May increase the serum concentration of Propafenone. Management: Canadian labeling recommends avoiding this combination. Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Asunaprevir: May increase the serum concentration of Propafenone. Avoid combination
Beta-Blockers: Propafenone may increase the serum concentration of Beta-Blockers. Propafenone possesses some independent beta blocking activity. Exceptions: Atenolol; Carteolol (Ophthalmic); Levobunolol; Metipranolol; Nadolol. Monitor therapy
Betrixaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Betrixaban. Management: Decrease the adult betrixaban dose to an initial single dose of 80 mg followed by 40 mg once daily if combined with a P-glycoprotein inhibitor. Consider therapy modification
Bilastine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Bilastine. Management: Consider alternatives when possible; bilastine should be avoided in patients with moderate to severe renal insufficiency who are receiving p-glycoprotein inhibitors. Consider therapy modification
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Cardiac Glycosides: Propafenone may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Celiprolol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Celiprolol. Monitor therapy
Cimetidine: May increase the serum concentration of Propafenone. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Colchicine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a p-glycoprotein inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Moderate): May increase the serum concentration of Propafenone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Exceptions: Thioridazine. Monitor therapy
CYP2D6 Inhibitors (Strong): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
CYP3A4 Inducers (Strong): May decrease the serum concentration of Propafenone. Monitor therapy
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Propafenone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Exceptions: Crizotinib; Erythromycin (Systemic); Fluconazole; Nilotinib; Ribociclib. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Propafenone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Exceptions: Ceritinib; Clarithromycin; Saquinavir; Voriconazole. Monitor therapy
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inhibitors may increase serum concentrations of the active metabolite(s) of Dabigatran Etexilate. Monitor therapy
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Domperidone: QT-prolonging Agents (Moderate Risk) may enhance the QTc-prolonging effect of Domperidone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Edoxaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Edoxaban. Management: See full monograph for details. Reduced doses are recommended for patients receiving edoxaban for venous thromboembolism in combination with certain P-gp inhibitors. Similar dose adjustment is not recommended for edoxaban use in atrial fibrillation. Consider therapy modification
Etravirine: May decrease the serum concentration of Propafenone. Monitor therapy
Everolimus: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Everolimus. Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
FLUoxetine: Propafenone may enhance the QTc-prolonging effect of FLUoxetine. FLUoxetine may increase the serum concentration of Propafenone. Monitor therapy
FluvoxaMINE: May increase the serum concentration of Propafenone. Monitor therapy
Fosamprenavir: May increase the serum concentration of Propafenone. Management: Concurrent use of ritonavir-boosted fosamprenavir with propafenone is contraindicated. The use of non-ritonavir-boosted fosamprenavir with propafenone is not specifically contraindicated but should only be undertaken with caution. Avoid combination
Haloperidol: QT-prolonging Class IC Antiarrhythmics (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ivabradine: Bradycardia-Causing Agents may enhance the bradycardic effect of Ivabradine. Monitor therapy
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Lacosamide: QT-prolonging Class IC Antiarrhythmics (Moderate Risk) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Larotrectinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Larotrectinib. Monitor therapy
Lefamulin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin tablets with P-glycoprotein/ABCB1 inhibitors. If concomitant use is required, monitor for lefamulin adverse effects. Consider therapy modification
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Methadone: Propafenone may enhance the QTc-prolonging effect of Methadone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Mirabegron: May increase the serum concentration of Propafenone. Management: Monitor clinical response to propafenone closely. Dose adjustment may be necessary. Canadian mirabegron labeling recommends restricting the maximum adult mirabegron dose to 25 mg/day in patients receiving propafenone. Monitor therapy
Naldemedine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naldemedine. Monitor therapy
Naloxegol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naloxegol. Monitor therapy
Ondansetron: QT-prolonging Class IC Antiarrhythmics (Moderate Risk) may enhance the QTc-prolonging effect of Ondansetron. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Orlistat: May decrease the serum concentration of Propafenone. Monitor therapy
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
PARoxetine: May increase the serum concentration of Propafenone. Monitor therapy
PAZOPanib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pentamidine (Systemic): QT-prolonging Class IC Antiarrhythmics (Moderate Risk) may enhance the QTc-prolonging effect of Pentamidine (Systemic). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Perhexiline: CYP2D6 Inhibitors (Weak) may increase the serum concentration of Perhexiline. Monitor therapy
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Exceptions: Loperamide. Monitor therapy
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Propranolol: Propafenone may increase the serum concentration of Propranolol. Monitor therapy
Prucalopride: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Prucalopride. Monitor therapy
QT-prolonging Antidepressants (Moderate Risk): QT-prolonging Class IC Antiarrhythmics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Antipsychotics (Moderate Risk): QT-prolonging Class IC Antiarrhythmics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Pimozide. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): Propafenone may enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): May enhance the QTc-prolonging effect of other QT-prolonging Class IC Antiarrhythmics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Class III Antiarrhythmics (Highest Risk): Propafenone may enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Kinase Inhibitors (Highest Risk): Propafenone may enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Kinase Inhibitors (Moderate Risk): QT-prolonging Class IC Antiarrhythmics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Miscellaneous Agents (Highest Risk): Propafenone may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Miscellaneous Agents (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Class IC Antiarrhythmics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): QT-prolonging Class IC Antiarrhythmics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Class IC Antiarrhythmics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): QT-prolonging Class IC Antiarrhythmics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Ranolazine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Ranolazine. Monitor therapy
RifAXIMin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RifAXIMin. Monitor therapy
Ritonavir: May increase the serum concentration of Propafenone. Avoid combination
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Sertraline: May enhance the QTc-prolonging effect of Propafenone. Sertraline may increase the serum concentration of Propafenone. Monitor therapy
Silodosin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Silodosin. Monitor therapy
Simeprevir: May increase the serum concentration of Propafenone. Monitor therapy
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
St John's Wort: May decrease the serum concentration of Propafenone. Monitor therapy
Talazoparib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Talazoparib. Management: These listed exceptions are discussed in detail in separate interaction monographs. Monitor therapy
Tegaserod: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Tegaserod. Monitor therapy
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Tipranavir: May increase the serum concentration of Propafenone. Avoid combination
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Topotecan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Ubrogepant: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and second dose (if needed) of 50 mg when used with a P-gp inhibitor. Consider therapy modification
Venetoclax: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Venetoclax. Management: Consider a venetoclax dose reduction by at least 50% in patients requiring concomitant treatment with P-glycoprotein (P-gp) inhibitors. Consider therapy modification
Venlafaxine: Propafenone may increase the serum concentration of Venlafaxine. Management: Monitor for increased venlafaxine levels/adverse effects (e.g., hallucinations, agitation, confusion) with propafenone initiation/dose increase. Conversely, monitor for decreased venlafaxine levels with profapenone discontinuation/dose decrease. Monitor therapy
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vitamin K Antagonists (eg, warfarin): Propafenone may increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Unusual taste (3% to 23%), dizziness (4% to 15%)
Gastrointestinal: Nausea (≤11%), vomiting (≤11%)
1% to 10%:
Cardiovascular: Cardiac arrhythmia (2% to 10%; new or worsened; proarrhythmic effect), angina pectoris (2% to 5%), cardiac failure (1% to 4%), first degree atrioventricular block (1% to 3%), palpitations (1% to 3%), ventricular tachycardia (1% to 3%), bradycardia (1% to 2%), chest pain (1% to 2%), widened QRS complex on ECG (1% to 2%), syncope (1% to 2%), ventricular premature contractions (1% to 2%), atrial fibrillation (1%), bundle branch block (≤1%), edema (≤1%), cardiac conduction delay (≤1%; intraventricular), hypotension (≤1%)
Central nervous system: Fatigue (2% to 6%), headache (2% to 5%), ataxia (≤2%), insomnia (≤2%), anxiety (1% to 2%), drowsiness (1%)
Dermatologic: Skin rash (1% to 3%), diaphoresis (1%)
Gastrointestinal: Constipation (2% to 7%), diarrhea (1% to 3%), dyspepsia (1% to 3%), abdominal pain (1% to 2%), anorexia (1% to 2%), xerostomia (1% to 2%), flatulence (≤1%)
Neuromuscular & skeletal: Weakness (1% to 2%), arthralgia (≤1%), tremor (≤1%)
Ophthalmic: Blurred vision (1% to 6%)
Respiratory: Dyspnea (2% to 5%)
<1%, postmarketing, and/or case reports: Abnormal dreams, agranulocytosis, alopecia, altered sense of smell, amnesia, anemia, apnea, asystole, atrioventricular block (second or third degree), atrioventricular dissociation, cardiac failure, cholestasis, coma, confusion, depression, eye irritation, flushing, gastroenteritis, granulocytopenia, hepatitis, hyperglycemia, hyponatremia, impotence, increased serum transaminases, leukopenia, lupus erythematosus, mania, muscle cramps, myasthenia, nephrotic syndrome, numbness, pain, paresthesia, peripheral neuropathy, positive ANA titer, prolongation P-R interval on ECG, prolonged bleeding time, pruritus, psychosis, purpura, renal failure, seizure, SIADH (syndrome of inappropriate antidiuretic hormone secretion), sinoatrial arrest, sinus node dysfunction, speech disturbance, thrombocytopenia, tinnitus, torsades de pointes, ventricular fibrillation, vertigo, visual disturbance
Warnings/Precautions
Concerns related to adverse effects:
- Agranulocytosis: Agranulocytosis has been reported; generally occurring within the first 2 months of therapy. Upon therapy discontinuation, WBC usually normalized by 14 days.
- CNS effects: May cause dizziness, fatigue, blurred vision; caution patients about performing dangerous tasks (eg, driving, operating machinery).
- Conduction disturbances: Slows atrioventricular conduction, potentially leading to first degree AV block; degree of PR interval prolongation and increased QRS duration are dose and concentration related. Avoid in patients with conduction disturbances (unless functioning pacemaker present).
- Elevated antinuclear antibody titers: Positive antinuclear antibody (ANA) titers have been reported with use. Titers have decreased with and without therapy discontinuation. Positive titers have not usually been associated with clinical symptoms, although at least one case of drug-induced lupus erythematosus has been reported. Consider therapy discontinuation in symptomatic patients with positive ANA titers.
- Hepatotoxicity: Hepatic abnormalities (including fulminant hepatitis and fatalities) have been reported; toxicity appeared due to hepatocellular injury and/or cholestasis.
- Proarrhythmic effects: Can cause life-threatening drug-induced arrhythmias, including ventricular fibrillation, ventricular tachycardia, asystole, and torsade de pointes (Hii 1991). The manufacturer notes that propafenone may increase the QT interval; however, due to QRS prolongation, changes in the QT interval are difficult to interpret. In an evaluation of propafenone (450 mg/day) in healthy individuals compared to other selected antiarrhythmic agents, propafenone did not affect repolarization time (eg, QT, QTc, JT, JTc) only depolarization time (ie, QRS interval) (Sarubbi 1998). Monitor for proarrhythmic effects, and when necessary, adjust dose to prevent QTc prolongation.
Disease-related concerns:
- Brugada syndrome: Initiation of propafenone may unmask Brugada syndrome; obtain ECG after treatment initiation and discontinue if ECG indicative of Brugada syndrome.
- Electrolyte imbalance: Use is contraindicated in patients with uncorrected electrolyte abnormalities. Correct electrolyte disturbances, especially hypokalemia or hypomagnesemia, prior to use and throughout therapy.
- Heart failure (HF): Avoid use in patients with HF; similar agents have been shown to increase mortality in this population; may precipitate or exacerbate condition (Lindenfeld 2010).
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Myasthenia gravis: Use with caution in patients with myasthenia gravis; may exacerbate condition.
- Pulmonary disease: Propafenone use may be considered in patients with obstructive lung disease who do not have bronchospasm (AHA/ACC/HRS [January 2014]). Use in patients with bronchospastic disease or severe obstructive lung disease is contraindicated.
- Renal impairment: Use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- CAST trial: [US Boxed Warning]: In the Cardiac Arrhythmia Suppression Trial (CAST), recent (>6 days but <2 years ago) myocardial infarction patients with asymptomatic, non-life-threatening ventricular arrhythmias did not benefit and may have been harmed by attempts to suppress the arrhythmia with flecainide or encainide. An increased mortality or nonfatal cardiac arrest rate (7.7%) was seen in the active treatment group compared with patients in the placebo group (3%). The applicability of the CAST results to other populations is unknown. Antiarrhythmic agents should be reserved for patients with life-threatening ventricular arrhythmias.
- Pacemakers: May alter pacing and sensing thresholds of artificial pacemakers.
Monitoring Parameters
ECG, blood pressure, pulse (particularly at initiation of therapy)
Pregnancy
Pregnancy Considerations
Propafenone and the 5-hydroxypropafenone metabolite cross the placenta and can be detected in the newborn (Libardoni 1991).
Due to pregnancy-induced physiologic changes, some pharmacokinetic properties of propafenone may be altered (Libardoni 1991).
Untreated maternal arrhythmias may cause adverse events in the mother and fetus; guidelines are available for the management of arrhythmias during pregnancy (ESC [Regitz-Zagrosek 2018]). Propafenone may be used for the ongoing management of pregnant women with highly symptomatic supraventricular tachycardia (SVT). The lowest effective dose is recommended; avoid use during the first trimester if possible (ACC/AHA/HRS [Page 2015]). Use is also recommended for the prevention of SVT in patients with Wolff-Parkinson-White (WPW) syndrome. Until more information is available, when prevention of SVT in patients without WPW syndrome, atrial tachycardia, or atrial fibrillation is needed in pregnant women, propafenone is generally reserved for use when other agents are not effective (ESC [Regitz-Zagrosek 2018]).
When used in males, reversible impairment of spermatogenesis may occur.
Patient Education
What is this drug used for?
- It is used to treat certain types of abnormal heartbeats.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Loss of strength and energy
- Constipation
- Change in taste
- Headache
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Chest pain
- Slow heartbeat
- Fast heartbeat
- Severe dizziness
- Passing out
- Abnormal heartbeat
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Blurred vision
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.