Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
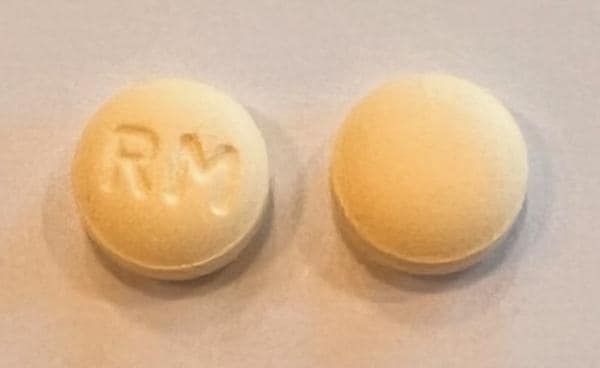
Tablet, Oral:
Rozerem: 8 mg
Generic: 8 mg
Pharmacology
Mechanism of Action
Potent, selective agonist of melatonin receptors MT1 and MT2 (with little affinity for MT3) within the suprachiasmic nucleus of the hypothalamus, an area responsible for determination of circadian rhythms and synchronization of the sleep-wake cycle. Agonism of MT1 is thought to preferentially induce sleepiness, while MT2 receptor activation preferentially influences regulation of circadian rhythms. Ramelteon is eightfold more selective for MT1 than MT2 and exhibits nearly sixfold higher affinity for MT1 than melatonin, presumably allowing for enhanced effects on sleep induction (Hatta 2014).
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid; high-fat meal delays Tmax and increases AUC (~31%)
Distribution
74 L
Metabolism
Extensive first-pass effect; oxidative metabolism primarily through CYP1A2 and to a lesser extent through CYP2C and CYP3A4; forms active metabolite (M-II)
Excretion
Primarily as metabolites: Urine (84%); feces (4%)
Onset of Action
30 minutes
Time to Peak
Median: 0.5 to 1.5 hours
Half-Life Elimination
Ramelteon: 1 to 2.6 hours; M-II: 2 to 5 hours
Protein Binding
~82%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Patients with mild and moderate hepatic impairment experienced a 4-fold and more than 10-fold increase in exposure, respectively.
Special Populations: Elderly
AUC is 97% higher and Cmax is 86% higher than in younger adults. AUC and Cmax of M-II metabolite increased 30% and 13%, respectively.
Use: Labeled Indications
Insomnia: Treatment of insomnia characterized by difficulty with sleep onset
Use: Off Label
Delirium (prevention), ICU relatedc
Evidence from a small number of patients >65 years of age in a controlled trial evaluating ramelteon use in the prevention of delirium in the intensive care unit (ICU) setting suggests a beneficial effect. However, the small sample size (N=24), limited observation period, and use of a delirium scale not typically employed in the United States or Europe warrant caution in the application of these results to other ICU populations. Larger controlled trials are needed to establish the role of ramelteon in the prevention of delirium. American College of Critical Care Medicine (ACCM), Society of Critical Care Medicine (SCCM), and American Society of Health-System Pharmacists (ASHP) clinical practice guidelines for the management of pain, agitation, and delirium in adult ICU patients do not mention ramelteon.
Contraindications
History of angioedema with previous ramelteon therapy (do not rechallenge); concurrent use with fluvoxamine
Dosage and Administration
Dosing: Adult
Insomnia: Oral: 8 mg once daily administered within 30 minutes of bedtime. Maximum dose: 8 mg/day.
Delirium (prevention), ICU related (off-label use): 8 mg once daily at bedtime (Hatta 2014). Additional trials may be necessary to further define the role of ramelteon in the prevention of ICU delirium.
Dosing: Geriatric
Refer to adult dosing; use with caution.
Administration
Administration with or immediately after a high-fat meal is not recommended due to delayed Tmax, reduced Cmax, and increased AUC. Swallow tablet whole; do not break. After taking ramelteon, patients should confine their activities to those necessary to prepare for bed.
Dietary Considerations
Do not take with high-fat meal.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture.
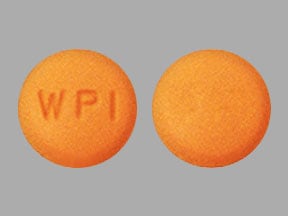
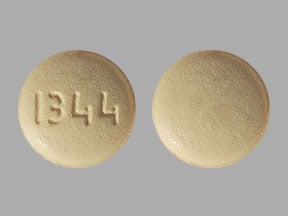
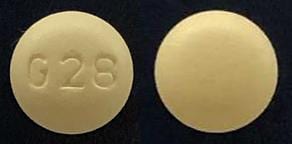
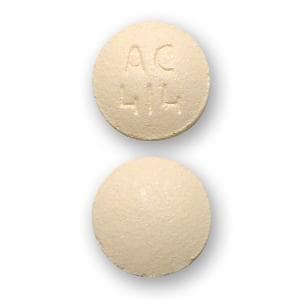
Ramelteon Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of Ramelteon. Monitor therapy
CYP1A2 Inhibitors (Strong): May increase the serum concentration of Ramelteon. Avoid combination
CYP3A4 Inducers (Strong): May decrease the serum concentration of Ramelteon. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Ramelteon. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Fluconazole: May increase the serum concentration of Ramelteon. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Melatonin: May enhance the sedative effect of Hypnotics (Nonbenzodiazepine). Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: Hypnotics (Nonbenzodiazepine) may enhance the CNS depressant effect of Sodium Oxybate. Avoid combination
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
1% to 10%:
Central nervous system: Dizziness (4% to 5%), somnolence (3% to 5%), fatigue (3% to 4%), insomnia worsened (3%), depression (2%)
Endocrine & metabolic: Serum cortisol decreased (1%)
Gastrointestinal: Nausea (3%), taste perversion (2%)
Neuromuscular & skeletal: Myalgia (2%), arthralgia (2%)
Respiratory: Upper respiratory infection (3%)
Miscellaneous: Influenza (1%)
Postmarketing and/or case reports: Anaphylaxis, angioedema, complex sleep-related behavior (sleep-driving, cooking or eating food, making phone calls), prolactin levels increased, testosterone levels decreased
Warnings/Precautions
Concerns related to adverse effects:
- Abnormal thinking/behavioral changes: Hypnotics/sedatives have been associated with abnormal thinking and behavior changes including decreased inhibition, aggression, bizarre behavior, agitation, hallucinations, and depersonalization. These changes may occur unpredictably and may indicate previously unrecognized psychiatric disorders; evaluate appropriately.
- CNS depression: May cause CNS depression impairing physical and mental capabilities; patients must be cautioned about performing tasks, which require mental alertness (operating machinery or driving).
- Hyperprolactinemia: May increase prolactin levels.
- Hypersensitivity reactions: Hypersensitivity reactions, including angioedema, have been reported (rare). Do not rechallenge patient if such reactions occur.
- Sleep-related activities: An increased risk for hazardous sleep-related activities such as sleep-driving, cooking and eating food, having sex, and making phone calls while asleep have been noted; amnesia, anxiety, and other neuropsychiatric symptoms may also occur. The use of alcohol, other CNS depressants, and exceeding the recommended maximum dose may increase the risk of these activities. Discontinue treatment in patients who report any complex sleep behavior.
Disease-related concerns:
- Depression: Use with caution in patients with depression; worsening of depression, including suicidal ideation has been reported with the use of hypnotics.
- Hepatic impairment: Use with caution in patients with hepatic impairment; use not recommended with severe impairment.
- Respiratory disease: Use with caution in patients with respiratory compromise, COPD or sleep apnea. Use is not recommended in patients with severe sleep apnea (has not been studied).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: Symptomatic treatment of insomnia should be initiated only after careful evaluation of potential causes of sleep disturbance. Failure of sleep disturbance to resolve after 7 to 10 days may indicate psychiatric and/or medical illness.
- Rapid onset: Because of the rapid onset of action, administer immediately prior to bedtime.
Pregnancy
Pregnancy Considerations
Adverse events were observed in some animal reproduction studies. May cause disturbances of reproductive hormonal regulation (eg, disruption of menses or decreased libido).
Patient Education
What is this drug used for?
- It is used to treat sleep problems.
Frequently reported side effects of this drug
- Fatigue
- Dizziness
- Loss of strength and energy
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Confusion
- Behavioral changes
- Mood changes
- Sensing things that seem real but are not
- Nightmares
- Trouble with memory
- Nausea
- Vomiting
- Swelling in your throat
- No menstrual periods
- Nipple discharge
- Decreased sex drive
- Trouble getting pregnant
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.