Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral:
Prandin: 0.5 mg [DSC], 1 mg [DSC], 2 mg [DSC] [contains corn starch]
Generic: 0.5 mg, 1 mg, 2 mg
Pharmacology
Mechanism of Action
Nonsulfonylurea hypoglycemic agent which blocks ATP-dependent potassium channels, depolarizing the membrane and facilitating calcium entry through calcium channels. Increased intracellular calcium stimulates insulin release from the pancreatic beta cells. Repaglinide-induced insulin release is glucose-dependent.
Pharmacokinetics/Pharmacodynamics
Absorption
Complete
Distribution
Vd: 31 L
Metabolism
Hepatic via CYP3A4 and CYP2C8 isoenzymes and glucuronidation to inactive metabolites
Excretion
Feces (~90%, <2% as unchanged drug); Urine (~8%, 0.1% as unchanged drug)
Time to Peak
Plasma: 1 hour
Half-Life Elimination
~1 hour
Protein Binding
Plasma: >98% to albumin
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC and Cmax are increased in severe renal impairment.
Special Populations: Hepatic Function Impairment
Higher and more prolonged serum concentrations have been observed in patients with moderate to severe hepatic impairment.
Use: Labeled Indications
Diabetes mellitus, type 2: To improve glycemic control in adults with type 2 diabetes mellitus as an adjunct to diet and exercise
Contraindications
Hypersensitivity to repaglinide or any component of the formulation; concurrent gemfibrozil therapy
Canadian labeling: Additional contraindications (not in US labeling): Severe hepatic impairment; concurrent use with clopidogrel; diabetic ketoacidosis, with or without coma; type 1 diabetes (insulin dependent)
Dosage and Administration
Dosing: Adult
Diabetes mellitus, type 2: Oral:
Patients whose HbA1c is <8%: Initial: 0.5 mg before each meal (2, 3, or 4 times/day depending on number of meals); may double the dose with each meal at intervals of ≥1 week until adequate glycemic control is achieved; maximum: 4 mg/dose or 16 mg/day.
Patients whose HbA1c is ≥8%: Initial: 1 or 2 mg before each meal (2, 3, or 4 times/day depending on number of meals); may double the dose with each meal at intervals of ≥1 week until adequate glycemic control is achieved; maximum: 4 mg/dose or 16 mg/day.
Dosage adjustment for concomitant therapy:
Clopidogrel: Avoid concomitant use; if concomitant use is necessary, initiate repaglinide at 0.5 mg before each meal; maximum: 4 mg/day.
Cyclosporine: Maximum: 6 mg/day of repaglinide.
Dosing: Geriatric
Refer to adult dosing.
Administration
Oral: Administer within 30 minutes before meals; may be administered preprandially 2, 3, or 4 times/day in response to changes in meal pattern. If a meal is missed, do not administer next scheduled dose; if hypoglycemia occurs, reduce dose.
Dietary Considerations
Administer 30 minutes before meals. Individualized medical nutrition therapy based on ADA recommendations is an integral part of therapy.
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from moisture.
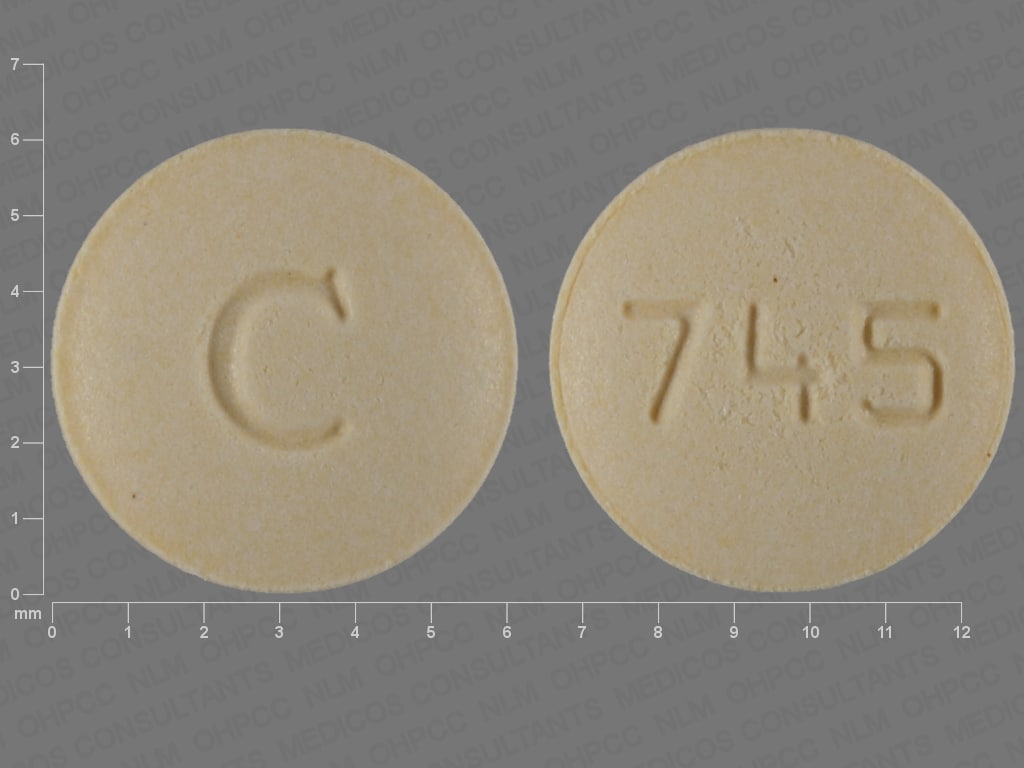
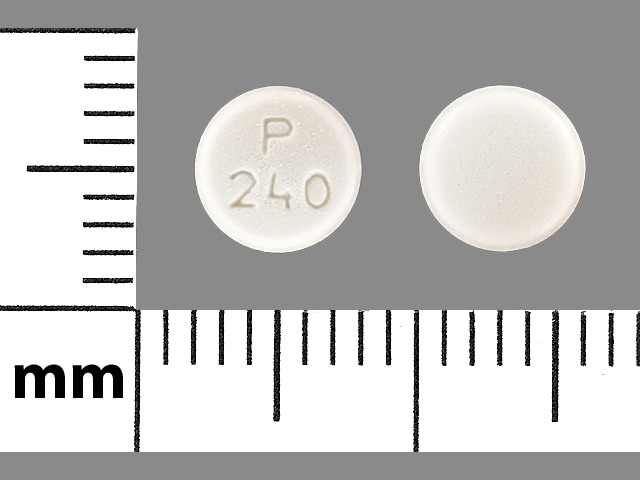
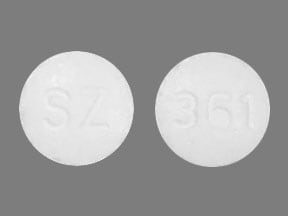
Repaglinide Images
Drug Interactions
Alpha-Lipoic Acid: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Antidiabetic Agents: May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Atazanavir: May increase the serum concentration of Repaglinide. Management: Use of repaglinide or other narrow therapeutic index CYP2C8 substrates with atazanavir without concurrent ritonavir is not recommended. If repaglinide is used with ritonavir-boosted atazanavir, no significant interaction is expected. Avoid combination
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Clopidogrel: May increase the serum concentration of Repaglinide. Management: Avoid use of clopidogrel and repaglinide if possible; if the combination must be used, limit total repaglinide daily dose to no more than 4 mg. This is contraindicated in some non-US labeling. Consider therapy modification
CycloSPORINE (Systemic): May increase the serum concentration of Repaglinide. Management: Limit the daily repaglinide dose to a maximum of 6 mg with concurrent use of cyclosporine, and monitor closely for increased repaglinide effects. Consider therapy modification
CYP2C8 Inhibitors (Moderate): May increase the serum concentration of Repaglinide. Exceptions: Clopidogrel. Monitor therapy
CYP2C8 Inhibitors (Strong): May increase the serum concentration of Repaglinide. Avoid combination
CYP2C8 Inhibitors (Weak): May increase the serum concentration of Repaglinide. Exceptions: Ketoconazole (Systemic). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Repaglinide. Management: The addition of a CYP2C8 inhibitor to this drug combination may substantially increase the magnitude of increase in repaglinide exposure. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Direct Acting Antiviral Agents (HCV): May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Eltrombopag: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erythromycin (Systemic): May increase the serum concentration of Repaglinide. Management: The addition of a CYP2C8 inhibitor to this drug combination may substantially increase the magnitude of increase in repaglinide exposure. Monitor therapy
Guanethidine: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Herbs (Hypoglycemic Properties): May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
HMG-CoA Reductase Inhibitors (Statins): May increase the serum concentration of Repaglinide. Monitor therapy
Hyperglycemia-Associated Agents: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Hypoglycemia-Associated Agents: May enhance the hypoglycemic effect of other Hypoglycemia-Associated Agents. Monitor therapy
Hypoglycemia-Associated Agents: Antidiabetic Agents may enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Letermovir: May increase the serum concentration of Repaglinide. Management: Monitor for increased repaglinide effects/toxicities (ie, hypoglycemia) if combined with letermovir. When letermovir is coadministered with cyclosporine, the use of repaglinide is not recommended. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
RifAMPin: May decrease the serum concentration of Repaglinide. Monitor therapy
Ritodrine: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Teriflunomide: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Thiazide and Thiazide-Like Diuretics: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tolvaptan: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Consider therapy modification
Adverse Reactions
>10%:
Central nervous system: Headache (9% to 11%)
Endocrine & metabolic: Hypoglycemia (16% to 31%)
Respiratory: Upper respiratory tract infection (10% to 16%)
1% to 10%:
Cardiovascular: Ischemia (4%), chest pain (2% to 3%)
Gastrointestinal: Diarrhea (4% to 5%), constipation (2% to 3%)
Genitourinary: Urinary tract infection (2% to 3%)
Hypersensitivity: Hypersensitivity reaction (1% to 2%)
Neuromuscular & skeletal: Back pain (5% to 6%), arthralgia (3% to 6%)
Respiratory: Sinusitis (3% to 6%), bronchitis (2% to 6%)
<1%, postmarketing, and/or case reports: Alopecia, anaphylactoid reaction, blurred vision (transient), cardiac arrhythmia, ECG abnormality, hemolytic anemia, hepatic insufficiency (severe), hepatitis, hypertension, increased liver enzymes, jaundice, leukopenia, myocardial infarction, palpitations, pancreatitis, Stevens-Johnson syndrome, thrombocytopenia, visual disturbance (transient)
Warnings/Precautions
Concerns related to adverse effects:
- Hypoglycemia: Severe hypoglycemia may occur; risk may be increased by changes in meal patterns, changes in physical activity levels, changes to coadministered medications, and concomitant use with other antidiabetic agents.
Disease-related concerns:
- Bariatric surgery:
– Altered absorption: Absorption may be altered given the anatomic and transit changes created by gastric bypass and sleeve gastrectomy surgery (Mingrone 2016; Mechanick 2013).
– Hypoglycemia: May increase the risk of hypoglycemia after gastric bypass, sleeve gastrectomy, and gastric band (Mechanick 2013). Insulin secretion and sensitivity may be partially or completely restored after these procedures (gastric bypass is most effective, followed by sleeve and, finally, band) (Korner 2009; Peterli 2012). First-phase insulin secretion and hepatic insulin sensitivity have been shown to be significantly improved in the immediate days after gastric bypass and sleeve gastrectomy. The restorative effects of these procedures on peripheral insulin sensitivity may occur later in the 3- to 12-month period after surgery. Where possible, the selection of antidiabetic agents without the potential for hypoglycemia is advised.
- Cardiovascular effects: Some studies suggest oral hypoglycemic drugs may be associated with increased cardiovascular events. Theoretically, repaglinide may also increase cardiovascular events, but there are no long-term studies assessing this concern. Use in combination with NPH insulin is not indicated; in two studies, reports of myocardial ischemia (6 events) in patients using repaglinide plus insulin have caused concern. Further evaluation is required to assess the safety of this combination.
- Hepatic impairment: Use with caution in patients with hepatic impairment; may be more susceptible to glucose-lowering effects.
- Renal impairment: Use with caution in patients with severe renal impairment; may be more susceptible to glucose-lowering effects.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant drug-drug interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: Not for use in patients with diabetic ketoacidosis or patients with type 1 diabetes mellitus.
Monitoring Parameters
Monitor fasting blood glucose (periodically) and glycosylated HbA1c levels (at least twice yearly in patients who have stable glycemic control and are meeting treatment goals; quarterly in patients not meeting treatment goals or with therapy change [ADA 2019]). During dose adjustment, fasting glucose can be used to determine response.
Pregnancy
Pregnancy Considerations
Repaglinide was shown to have a low potential to cross the placenta using an ex vivo perfusion model (Tertti 2011). Information describing the effects of repaglinide on pregnancy outcomes is limited.
Poorly controlled diabetes during pregnancy can be associated with an increased risk of adverse maternal and fetal outcomes, including diabetic ketoacidosis, preeclampsia, spontaneous abortion, preterm delivery, delivery complications, major birth defects, stillbirth, and macrosomia. To prevent adverse outcomes, prior to conception and throughout pregnancy, maternal blood glucose and HbA1c should be kept as close to target goals as possible but without causing significant hypoglycemia (ADA 2020; Blumer 2013).
Agents other than repaglinide are currently recommended to treat diabetes mellitus in pregnancy (ADA 2020).
Patient Education
What is this drug used for?
- It is used to lower blood sugar in patients with high blood sugar (diabetes).
Frequently reported side effects of this drug
- Headache
- Common cold symptoms
- Back pain
- Diarrhea
- Joint pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, a fast heartbeat, confusion, hunger, or sweating.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.