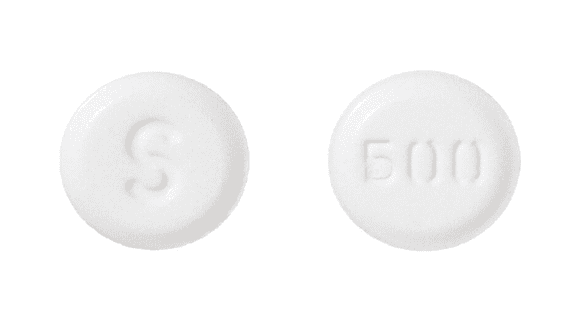
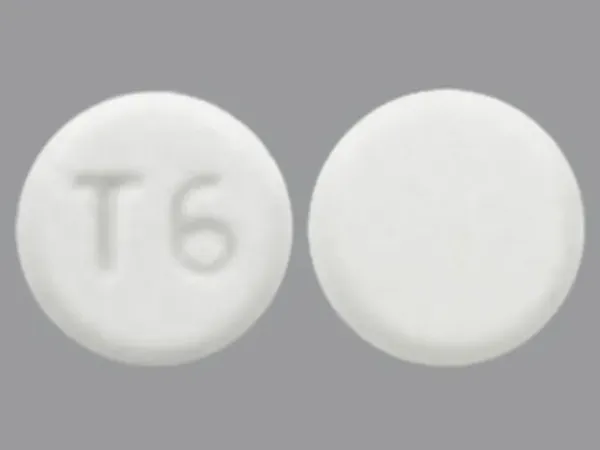
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Daliresp: 250 mcg, 500 mcg [contains corn starch]
Pharmacology
Mechanism of Action
Roflumilast and its active N-oxide metabolite selectively inhibit phosphodiesterase-4 (PDE4) leading to an accumulation of cyclic AMP (cAMP) within inflammatory and structural cells important in the pathogenesis of COPD. Anti-inflammatory effects include suppression of cytokine release and inhibition of lung infiltration by neutrophils and other leukocytes. Pulmonary remodeling and mucociliary malfunction are also attenuated.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: 2.9 L/kg
Metabolism
Hepatic via CYP3A4 and CYP1A2 to active N-oxide metabolite; also undergoes conjugation
Excretion
Urine (~70% as metabolites)
Time to Peak
~1 hour (delayed by food); N-oxide metabolite: ~8 hours
Half-Life Elimination
17 hours; N-oxide metabolite: 30 hours
Protein Binding
99%; N-oxide metabolite: 97%
Use in Specific Populations
Special Populations: Renal Function Impairment
In patients with severe renal impairment, roflumilast and N-oxide metabolite AUCs were decreased by 21% and 7%, respectively, and Cmax was reduced 16% and 12%, respectively.
Special Populations: Hepatic Function Impairment
The AUC of roflumilast and the N-oxide metabolite were increased by 51% and 24%, respectively, in Child-Pugh class A subjects and by 92% and 41%, respectively, in Child-Pugh class B subjects as compared with healthy subjects. The Cmax of roflumilast and the N-oxide metabolite was increased by 3% and 26%, respectively, in Child-Pugh class A subjects and by 26% and 40%, respectively, in Child-Pugh class B subjects.
Special Populations: Elderly
The roflumilast AUC and Cmax increased 27% and 16%, respectively, and the N-oxide metabolite AUC and Cmax increased 19% and 13%, respectively, in elderly patients.
Special Populations: Gender
The roflumilast and N-oxide metabolite AUC increased 39% and 33%, respectively, in healthy women when compared with healthy men.
Special Populations: Race
The AUC and Cmax of roflumilast and the N-oxide metabolite increased in white, black, Hispanic, and Japanese patients.
Special Populations Note
Cigarette smoking: The AUC of roflumilast in smokers was 13% less than in nonsmokers while the AUC of the N-oxide metabolite in smokers was 17% more than in nonsmokers.
Use: Labeled Indications
COPD: To reduce the risk of COPD exacerbations in patients with severe COPD associated with chronic bronchitis and a history of exacerbations
Limitations of use: Not indicated for the relief of acute bronchospasm
Contraindications
Moderate to severe hepatic impairment (Child-Pugh class B or C).
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to roflumilast or any component of the formulation.
Dosage and Administration
Dosing: Adult
COPD: Oral: 250 mcg once daily for 4 weeks, followed by 500 mcg once daily. Note: An initial dose of 250 mcg once daily is recommended for the first 4 weeks of treatment in an attempt to improve tolerability. However, this is not considered a therapeutic dose and the effect of this approach on long-term tolerability is uncertain.
Dosing: Geriatric
Refer to adult dosing.
Administration
Oral: Administer without regard to meals.
Storage
Store at 20°C to 25°C (68°F to 77°F), excursions permitted from 15°C to 30°C (59°F to 86°F).
Roflumilast Images
Drug Interactions
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Cimetidine: May increase serum concentrations of the active metabolite(s) of Roflumilast. Cimetidine may increase the serum concentration of Roflumilast. Monitor therapy
Ciprofloxacin (Systemic): May increase the serum concentration of Roflumilast. Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Roflumilast. Management: Roflumilast U.S. prescribing information recommends against combining strong CYP3A4 inducers with roflumilast. The Canadian product monograph makes no such recommendation but notes that such agents may reduce roflumilast therapeutic effects. Avoid combination
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
FluvoxaMINE: May increase serum concentrations of the active metabolite(s) of Roflumilast. FluvoxaMINE may increase the serum concentration of Roflumilast. Monitor therapy
Immunosuppressants: Roflumilast may enhance the immunosuppressive effect of Immunosuppressants. Exceptions: Beclomethasone (Oral Inhalation); Cytarabine (Liposomal); Fluticasone (Oral Inhalation). Consider therapy modification
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Loxapine: Agents to Treat Airway Disease may enhance the adverse/toxic effect of Loxapine. More specifically, the use of Agents to Treat Airway Disease is likely a marker of patients who are likely at a greater risk for experiencing significant bronchospasm from use of inhaled loxapine. Management: This is specific to the Adasuve brand of loxapine, which is an inhaled formulation. This does not apply to non-inhaled formulations of loxapine. Avoid combination
RifAMPin: May decrease the serum concentration of Roflumilast. Management: Roflumilast U.S. prescribing information recommends against combining rifampin with roflumilast. The Canadian product monograph makes no such recommendation but notes that rifampin may reduce roflumilast therapeutic effects. Avoid combination
Riociguat: Roflumilast may enhance the hypotensive effect of Riociguat. Management: Riociguat is contraindicated with nonselective phosphodiesterase (PDE) inhibitors and PDE type 5 inhibitors. Other types of PDE inhibitors are not contraindicated, but caution is advised and patients should be monitored for hypotension. Monitor therapy
Tobacco (Smoked): May decrease the serum concentration of Roflumilast. Monitor therapy
Adverse Reactions
2% to 10%:
Central nervous system: Headache (4%), dizziness (2%), insomnia (2%)
Endocrine & metabolic: Weight loss (5% to 10% of body weight: 8% to 20%; >10% loss: 7%)
Gastrointestinal: Diarrhea (10%), nausea (5%), decreased appetite (2%)
Infection: Influenza (3%)
Neuromuscular & skeletal: Back pain (3%)
<2%, postmarketing, and/or case reports: Abdominal pain, anemia, anxiety, arthralgia, arthritis, atrial fibrillation, constipation, depression, dysgeusia, dyspepsia, epistaxis, fatigue, gastritis, gastroesophageal reflux disease, gynecomastia, hematochezia, hypersensitivity, hypersensitivity reaction (including angioedema, urticaria, and rash), increased gamma-glutamyl transferase, increased lactate dehydrogenase, increased serum AST, limb pain, lung carcinoma, malaise, muscle spasm, myalgia, myasthenia, nervousness, pancreatitis, paresthesia, prostate carcinoma, renal failure, respiratory tract infection, rhinitis, sinusitis, suicidal ideation, suicidal tendencies, suicide, supraventricular cardiac arrhythmia, tremor, urinary tract infection, vertigo, vomiting, weakness
Warnings/Precautions
Concerns related to adverse effects:
- Neuropsychiatric: Neuropsychiatric effects (eg, anxiety, depression, insomnia) have been reported with use; rarely, suicidal behavior/ideation and completed suicide were reported. Assess risk versus benefits before prescribing in patients with a history of depression with suicidal behavior/ideations; instruct patients/caregivers to report psychiatric symptoms and consider discontinuation of therapy in such patients.
- Weight loss: Weight loss has occurred; monitor weight regularly. If unexplained or significant weight loss occurs, discontinuation should be considered.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with mild impairment (systemic exposure may be increased); use in moderate to severe impairment is contraindicated.
Other warnings/precautions:
- Appropriate use: Not indicated for relieving acute bronchospasm.
Monitoring Parameters
Liver function tests; weight (regularly during therapy); new or worsening insomnia, anxiety, depression, suicidal thoughts, or other mood changes.
Pregnancy
Pregnancy Considerations
Adverse events were observed in some animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat COPD (chronic obstructive pulmonary disease).
- This drug is not to be used to treat intense flare-ups of shortness of breath. Use a rescue inhaler. Talk with the doctor.
Frequently reported side effects of this drug
- Dizziness
- Nausea
- Diarrhea
- Headache
- Back pain
- Flu-like symptoms
- Trouble sleeping
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Severe anxiety
- Excessive weight loss
- Agitation
- Irritability
- Panic attacks
- Mood changes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.