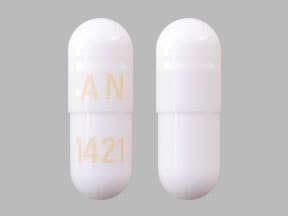
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Rapaflo: 4 mg, 8 mg
Generic: 4 mg, 8 mg
Pharmacology
Mechanism of Action
Silodosin is a selective antagonist of alpha1A-adrenoreceptors in the prostate and bladder. Smooth muscle tone in the prostate is mediated by alpha1A-adrenoreceptors; blocking them leads to relaxation of smooth muscle in the bladder neck and prostate causing an improvement of urine flow and decreased symptoms of BPH. Approximately 75% of the alpha1-receptors in the prostate are of the alpha1A subtype.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapidly absorbed (Lepor 2010)
Distribution
Vd: 49.5 L
Metabolism
Extensive, via CYP3A4, glucuronidation, and alcohol and aldehyde dehydrogenase pathways; KMD-3213G (active in vitro) and KMD-3293 (not significant) metabolites formed
Excretion
Feces (55%); urine (34%)
Time to Peak
Silodosin: ~3 hours; KMD-3213G: ~5.5 hours (Lepor 2010)
Half-Life Elimination
Healthy volunteers: Silodosin: ~13 hours (mean); KMD-3213G: ~24 hours
Protein Binding
~97%
Use in Specific Populations
Special Populations: Renal Function Impairment
Total silodosin (bound and unbound) AUC, Cmax, and elimination half-life were 3.2-, 3.1-, and 2-fold higher, respectively, in patients with moderate renal impairment. Unbound AUC and Cmax were 2- and 1.5-fold higher, respectively.
Special Populations: Hepatic Function Impairment
Pharmacokinetics are not altered in patients with moderate hepatic impairment. Patients with severe hepatic impairment have not been studied.
Special Populations: Elderly
Exposure and elimination half-life are approximately 15% and 20%, respectively, greater in subjects with a mean age of 69 years compared with subjects with a mean age of 24 years.
Use: Labeled Indications
Treatment of signs and symptoms of benign prostatic hyperplasia (BPH)
Use: Off Label
Ureteral calculi (distal)b
Use of alpha-1 adrenergic blockers for treating ureteral calculi is recommended by US guidelines and is supported by data from meta-analyses and controlled trials. Tamsulosin has the most data, but silodosin has demonstrated efficacy in facilitating expulsion of distal ureteral stones (<10 mm) as medical expulsive therapy Sur 2015, Wang 2016.
Data from two trials and a meta-analysis indicates that silodosin may lead to decreased expulsion time when compared to tamsulosin Dell’Atti 2015, Kumar 2015, Liu 2017; however, additional studies are needed to confirm this.
Contraindications
US labeling: Hypersensitivity to silodosin or any component of the formulation, concurrent use with strong CYP3A4 inhibitors (eg, clarithromycin, itraconazole, ketoconazole, ritonavir); severe renal impairment (CrCl <30 mL/minute); severe hepatic impairment (Child-Pugh class C)
Canadian labeling: Additional contraindications (not in US labeling): Concurrent use with other alpha-blockers (eg, prazosin, terazosin, doxazosin)
Dosage and Administration
Dosing: Adult
BPH: Oral: 8 mg once daily with a meal
Ureteral calculi (distal) expulsion (off-label use): Oral: 8 mg once daily, discontinue after successful expulsion (average time to expulsion was 3 to 18 days) (Dell’Atti 2015; Kumar 2015; Wang 2016). Note: Patients with stones >10 mm were excluded from studies.
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer with a meal. Capsules may be opened and the powder sprinkled onto a tablespoon of applesauce (not hot). The applesauce should be swallowed within 5 minutes without chewing and followed with 8 oz of cool water. Subdividing the capsule contents is not recommended. Do not store for future use.
Storage
Store at room temperature of 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light. Protect from moisture.
Silodosin Images
Drug Interactions
Alpha-/Beta-Agonists: Alpha1-Blockers may diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Similarly, Alpha-/Beta-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
Alpha1-Agonists: Alpha1-Blockers may diminish the vasoconstricting effect of Alpha1-Agonists. Similarly, Alpha1-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
Alpha1-Blockers: May enhance the antihypertensive effect of other Alpha1-Blockers. Avoid combination
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Beta-Blockers: May enhance the orthostatic hypotensive effect of Alpha1-Blockers. The risk associated with ophthalmic products is probably less than systemic products. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Calcium Channel Blockers: Alpha1-Blockers may enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Silodosin. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Silodosin. Avoid combination
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapoxetine: May enhance the orthostatic hypotensive effect of Alpha1-Blockers. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of Silodosin. Monitor therapy
Phosphodiesterase 5 Inhibitors: Alpha1-Blockers (Uroselective) may enhance the hypotensive effect of Phosphodiesterase 5 Inhibitors. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Rilmenidine: Alpha1-Blockers may enhance the hypotensive effect of Rilmenidine. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Adverse Reactions
>10%: Genitourinary: Retrograde ejaculation (28%)
1% to 10%:
Cardiovascular: Orthostatic hypotension (3%; increased in elderly ≥65 years up to 5%)
Central nervous system: Dizziness (3%), headache (2%), insomnia (1% to 2%)
Gastrointestinal: Diarrhea (3%), abdominal pain (1% to 2%)
Genitourinary: Prostate specific antigen increased (1% to 2%)
Neuromuscular & skeletal: Weakness (1% to 2%)
Respiratory: Nasal congestion (2%), rhinorrhea (1% to 2%), sinusitis (1% to 2%)
<1%, postmarketing, and/or case reports: Hepatic insufficiency, hypersensitivity reaction, increased serum transaminases, intraoperative floppy iris syndrome, jaundice, pharyngeal edema, priapism, pruritus, purpura, skin rash (including toxic), swollen tongue, syncope, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Floppy iris syndrome: Intraoperative floppy iris syndrome has been observed in cataract surgery patients who were on or were previously treated with alpha1-blockers; causality has not been established and there appears to be no benefit in discontinuing alpha-blocker therapy prior to surgery.
- Orthostatic hypotension/syncope: May cause significant orthostatic hypotension with or without syncope, especially with first dose; anticipate a similar effect if therapy is interrupted for a few days, if dosage is rapidly increased, or if another antihypertensive drug (particularly vasodilators) or a PDE-5 inhibitor (eg, sildenafil, tadalafil, vardenafil) is introduced although coadministration of sildenafil or tadalafil with silodosin was not associated with a clinically significant risk of orthostatic hypotension in one clinical trial (MacDiarmid 2010). “First-dose” orthostatic hypotension may occur 4 to 8 hours after dosing; may be dose related. Patients should be cautioned about performing hazardous tasks, driving, or operating heavy machinery when starting new therapy or adjusting dosage upward.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with mild-to-moderate hepatic impairment; contraindicated with severe impairment; not studied.
- Prostate cancer: It is recommended to rule out prostatic carcinoma before beginning therapy.
- Renal impairment: Use with caution in patients with moderate renal impairment; dosage adjustment recommended. Contraindicated in patients with severe impairment (CrCl <30 mL/minute).
Concurrent drug therapy issues:
- High potential for interactions: Contraindicated in patients on strong CYP3A4 inhibitors.
Special populations:
- Elderly: Use with caution in the elderly; risk of orthostatic hypotension increases with increasing age. Patients ≥65 years of age experienced an incidence of up to 5% in clinical trials.
- Females: Not indicated for use in women.
- Pediatric: Not indicated for use in children.
Other warnings/precautions:
- Antihypertensive use: Not intended for use as an antihypertensive drug.
Monitoring Parameters
Blood pressure; urinary symptoms
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Teratogenic effects were not observed in animal studies; however, silodosin is not approved for use in women.
Patient Education
What is this drug used for?
- In men, it is used to treat the signs of an enlarged prostate.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Sexual dysfunction
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.