Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral, as succinate:
VESIcare: 5 mg, 10 mg [contains corn starch]
Generic: 5 mg, 10 mg
Pharmacology
Mechanism of Action
Inhibits muscarinic receptors resulting in decreased urinary bladder contraction, increased residual urine volume, and decreased detrusor muscle pressure.
Pharmacokinetics/Pharmacodynamics
Distribution
Vdss: 600 L
Metabolism
Extensively hepatic; via N-oxidation and 4 R-hydroxylation, forms 1 active and 3 inactive metabolites; primary pathway for elimination is via CYP3A4
Excretion
Urine (69.2%; <15% as unchanged drug); feces (22.5%)
Time to Peak
Plasma: 3 to 8 hours
Half-Life Elimination
45 to 68 hours following chronic dosing; prolonged in severe renal (CrCl <30 mL/minute) or moderate hepatic (Child-Pugh class B) impairment
Protein Binding
~98%, primarily to alpha1-acid glycoprotein
Use in Specific Populations
Special Populations: Renal Function Impairment
There is a 2.1-fold increase in AUC and 1.6-fold increase in half-life of solifenacin in patients with severe impairment (CrCl <30 mL/minute).
Special Populations: Hepatic Function Impairment
There is a 2-fold increase in the half-life and 35% increase in AUC of solifenacin in patients with moderate impairment (Child-Pugh class B).
Special Populations: Elderly
In elderly patients (65 to 80 years), Cmax, AUC, and half-life values were 20% to 25% higher.
Use: Labeled Indications
Overactive bladder: Treatment of overactive bladder with symptoms of urinary frequency, urgency, or urge incontinence.
Contraindications
Hypersensitivity to solifenacin or any component of the formulation; urinary retention; gastric retention; uncontrolled narrow-angle glaucoma
Canadian labeling: Additional contraindication (not in the US labeling): Dialysis
Dosage and Administration
Dosing: Adult
Overactive bladder: Oral: Initial: 5 mg once daily; if tolerated, may increase to 10 mg once daily.
Dosage adjustment with concomitant potent CYP3A4 inhibitors (eg, ketoconazole): Maximum dose: 5 mg/day
Administration
Administer with water without regard to food. Swallow whole. Do not crush or chew.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
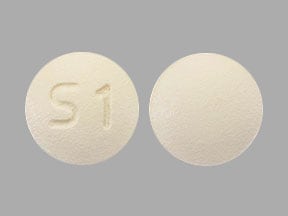
Solifenacin Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Cannabinoid-Containing Products: Anticholinergic Agents may enhance the tachycardic effect of Cannabinoid-Containing Products. Exceptions: Cannabidiol. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Solifenacin. Management: Limit solifenacin doses to 5 mg daily when combined with strong CYP3A4 inhibitors. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Itraconazole: May increase the serum concentration of Solifenacin. Management: Limit solifenacin doses to 5 mg daily when combined with itraconazole. Do not use solifenacin with itraconazole, or for 2 weeks after itraconazole discontinuation, in patients with moderate to severe hepatic impairment or severe renal impairment. Consider therapy modification
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mirabegron: May enhance the adverse/toxic effect of Solifenacin. Specifically, the risk of acute urinary retention may be enhanced. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: Anticholinergic Agents may enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Adverse Reactions
>10%: Gastrointestinal: Xerostomia (11% to 28%), constipation (5% to 13%)
1% to 10%:
Cardiovascular: Hypertension (1%), lower extremity edema (1%)
Central nervous system: Fatigue (2%), depression (1%)
Gastrointestinal: Dyspepsia (4%), nausea (3%), upper abdominal pain (2%), vomiting (1%)
Genitourinary: Urinary tract infection (5%), urinary retention (1%)
Ophthalmic: Blurred vision (4% to 5%), dry eye syndrome (2%)
Respiratory: Cough (1%)
Miscellaneous: Influenza (2%)
<1%, postmarketing, and/or case reports: Abnormal hepatic function tests, anaphylaxis, angioedema, atrial fibrillation, confusion, decreased appetite, delirium, drowsiness, dry nose, dysgeusia, erythema multiforme, exfoliative dermatitis, fecal impaction, gastroesophageal reflux disease, gastrointestinal obstruction, glaucoma, hallucination, headache, hyperkalemia, hypersensitivity reaction, myasthenia, palpitations, prolonged Q-T interval on ECG, peripheral edema, pruritus, renal insufficiency, skin rash, tachycardia, torsades de pointes, urticaria, voice disorder, xeroderma
Warnings/Precautions
Concerns related to adverse effects:
- Angioedema: Angioedema involving the face, lips, tongue, and/or larynx have been reported; some cases have occurred after the first dose. May be life-threatening. Immediately discontinue and institute supportive care if tongue, hypopharynx, or larynx is involved.
- CNS effects: CNS effects have been reported (eg, headache, confusion, hallucinations, somnolence); monitor for CNS effects, particularly at treatment initiation or dose increase; reduce dose or discontinue, if necessary. May cause drowsiness and/or blurred vision, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- Heat prostration: May occur in the presence of increased environmental temperature; use caution in hot weather and/or exercise.
- Hypersensitivity reactions: Anaphylactic reactions have been reported rarely; immediately discontinue therapy if anaphylactic reaction develops.
Disease-related concerns:
- Alzheimer disease: Preliminary data suggest that long-term use of anticholinergics may potentially adversely affect the clinical course of Alzheimer disease in patients receiving cholinesterase inhibitors (Lu 2003, Sink 2008). Additional monitoring for decreases in cognition and functional abilities and increased problematic behaviors should be considered in patients with dementia receiving dual therapy with an acetylcholinesterase inhibitor and a bladder anticholinergic, such as solifenacin.
- Bladder outflow obstruction: Use with caution in patients with bladder outflow obstruction (eg, BPH); may increase the risk of urinary retention.
- Gastrointestinal disease: Use with caution in patients with decreased GI motility (severe constipation, ulcerative colitis) or GI obstructive disorders (pyloric stenosis); may increase the risk of gastric retention.
- Glaucoma: Use with caution in patients with controlled (treated) narrow-angle glaucoma; use is contraindicated in uncontrolled narrow-angle glaucoma.
- Hepatic impairment: Use with caution in patients with moderate hepatic impairment (Child-Pugh class B); dosage adjustment required; use is not recommended in patients with severe hepatic impairment (Child-Pugh class C).
- QT prolongation: Use with caution in patients with a known history of QT prolongation or other risk factors for QT prolongation (eg, concomitant use of medications known to prolong QT interval, electrolyte abnormalities). The risk for QT prolongation is dose-related.
- Renal impairment: Use with caution in patients with renal impairment; dosage adjustment is required for severe renal impairment (CrCl <30 mL/minute).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
Anticholinergic effects (eg, CNS effects [headache, confusion, hallucinations, somnolence], fixed and dilated pupils, blurred vision, tremors, dry skin); creatinine clearance; hepatic function; post-void residuals when added to alpha-blocker therapy for BPH.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events were observed in some animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat an overactive bladder.
Frequently reported side effects of this drug
- Constipation
- Headache
- Dry eyes
- Blurred vision
- Dry mouth
- Fatigue
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain.
- Severe dizziness
- Passing out
- Severe loss of strength and energy
- Confusion
- Sensing things that seem real but are not
- Severe abdominal pain
- Lack of sweat
- Unable to pass urine
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.