Boxed Warning
Hematologic toxicity:
Ticlopidine HCl can cause life-threatening hematological adverse reactions, including neutropenia/agranulocytosis and thrombotic thrombocytopenic purpura (TTP) and aplastic anemia.
Neutropenia/agranulocytosis:
Among 2048 patients in clinical trials, there were 50 cases (2.4%) of neutropenia (less than 1200 neutrophils/mm3), and the neutrophil count was below 450/mm3 in 17 of these patients (0.8% of the total population).
TTP:
One case of TTP was reported during clinical trials. Based on postmarketing data, US physicians reported about 100 cases between 1992 and 1997. Based on an estimated patient exposure of 2 million to 4 million, and assuming an event reporting rate of 10% (the true rate is not known), the incidence of ticlopidine-associated TTP may be as high as 1 case in every 2000 to 4000 patients exposed.
Aplastic anemia:
Aplastic anemia was not seen during clinical trials in stroke patients, but US physicians reported about 50 cases between 1992 and 1998. Based on an estimated patient exposure of 2 million to 4 million, and assuming an event reporting rate of 10% (the true rate is not known), the incidence of ticlopidine-associated aplastic anemia may be as high as 1 case in every 4000 to 8000 patients exposed.
Monitoring of clinical and hematologic status:
Severe hematologic adverse reactions may occur within a few days of the start of therapy. The incidence of TTP peaks after about 3 to 4 weeks of therapy and neutropenia peaks at approximately 4 to 6 weeks. The incidence of aplastic anemia peaks after about 4 to 8 weeks of therapy. The incidence of the hematologic adverse reactions declines thereafter. Only a few cases of neutropenia, TTP, or aplastic anemia have arisen after more than 3 months of treatment.
Hematological adverse reactions cannot be reliably predicted by any identified demographic or clinical characteristics. During the first 3 months of treatment, patients receiving ticlopidine HCl must, therefore, be hematologically and clinically monitored for evidence of neutropenia or TTP. If any such evidence is seen, ticlopidine HCl should be immediately discontinued.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
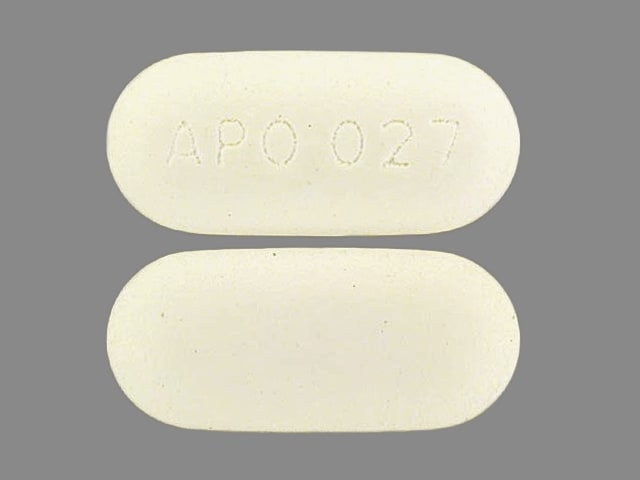
Tablet, Oral, as hydrochloride:
Generic: 250 mg [DSC]
Pharmacology
Mechanism of Action
Ticlopidine requires in vivo biotransformation to an unidentified active metabolite. This active metabolite irreversibly blocks the P2Y12 component of ADP receptors, which prevents activation of the GPIIb/IIIa receptor complex, thereby reducing platelet aggregation. Platelets blocked by ticlopidine are affected for the remainder of their lifespan.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Metabolism
Extensively hepatic; has at least 1 active metabolite
Excretion
Urine (60%); feces (23%)
Onset of Action
~6 hours; Peak effect: 3-5 days; serum levels do not correlate with clinical antiplatelet activity
Time to Peak
~2 hours
Half-Life Elimination
13 hours
Protein Binding
Parent drug: 98%; <15% bound to alpha1-acid glycoprotein
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Average plasma concentration is slightly higher in cirrhosis.
Use: Labeled Indications
Platelet aggregation inhibitor that reduces the risk of thrombotic stroke in patients who have had a stroke or stroke precursors (Note: Due to its association with life-threatening hematologic disorders, ticlopidine should be reserved for patients who are intolerant to aspirin, who have failed aspirin therapy, or who are not eligible to receive other antiplatelet therapy.)
Contraindications
Hypersensitivity to ticlopidine or any component of the formulation; active pathological bleeding such as peptic ulcer bleeding or intracranial hemorrhage; severe liver impairment; hematopoietic disorders (neutropenia, thrombocytopenia, or a past history of TTP or aplastic anemia); hemostatic disorders
Ticlopidine Images
Dosage and Administration
Dosing: Adult
Note: Ticlopidine is no longer available in the US.
Stroke prevention: Oral: 250 mg twice daily
Note: Overall, the use of ticlopidine is no longer recommended for this indication and has largely been replaced by clopidogrel (Lindsay 2012).
Dosing: Geriatric
Oral: 250 mg twice daily with food; dosage in older patients has not been determined; however, in two large clinical trials, the average age of subjects was 63 and 66 years. A dosage decrease may be necessary if bleeding occurs.
Administration
Administer with food.
Drug Interactions
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Apixaban: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Consider therapy modification
ARIPiprazole: CYP2D6 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
BuPROPion: CYP2B6 Inhibitors (Weak) may increase the serum concentration of BuPROPion. Monitor therapy
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Cilostazol: Ticlopidine may increase serum concentrations of the active metabolite(s) of Cilostazol. Ticlopidine may increase the serum concentration of Cilostazol. Monitor therapy
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Dabigatran Etexilate: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Dabigatran Etexilate. Specifically, the risk of bleeding may be increased. Antiplatelet Agents (P2Y12 Inhibitors) may increase the serum concentration of Dabigatran Etexilate. Specifically, clopidogrel may increase dabigatran serum concentrations. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dasatinib: May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Edoxaban: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider the anticipated risks and benefits of this combination. If combined, increased monitoring for bleeding is recommended. Consider therapy modification
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
FentaNYL: May diminish the antiplatelet effect of Antiplatelet Agents (P2Y12 Inhibitors). FentaNYL may decrease the serum concentration of Antiplatelet Agents (P2Y12 Inhibitors). Monitor therapy
Fosphenytoin: Ticlopidine may increase the serum concentration of Fosphenytoin. Monitor therapy
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Heparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or agents with antiplatelet properties if coadministration is required. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Morphine (Systemic): May diminish the antiplatelet effect of Antiplatelet Agents (P2Y12 Inhibitors). Morphine (Systemic) may decrease the serum concentration of Antiplatelet Agents (P2Y12 Inhibitors). Management: Consider alternative anti-ischemic/analgesic therapies (eg, beta-blockers, nitroglycerin) in patients with acute coronary syndromes treated with a P2Y12 inhibitor when possible. The risks associated with other opioids are unknown. Consider therapy modification
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Perhexiline: CYP2D6 Inhibitors (Weak) may increase the serum concentration of Perhexiline. Monitor therapy
Phenytoin: Ticlopidine may increase the serum concentration of Phenytoin. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Rivaroxaban: Antiplatelet Agents (P2Y12 Inhibitors) may enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Consider therapy modification
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Sibutramine: CYP2B6 Inhibitors (Weak) may increase serum concentrations of the active metabolite(s) of Sibutramine. CYP2B6 Inhibitors (Weak) may increase the serum concentration of Sibutramine. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Adverse Reactions
As with all drugs which may affect hemostasis, bleeding is associated with ticlopidine. Hemorrhage may occur at virtually any site. Risk is dependent on multiple variables, including the use of multiple agents which alter hemostasis and patient susceptibility.
>10%:
Endocrine & metabolic: Hyperlipidemia (8% to 10%; within 1 month of therapy), increased serum triglycerides
Gastrointestinal: Diarrhea (13%; may be chronic)
1% to 10%:
Central nervous system: Dizziness (1%)
Dermatologic: Skin rash (5%), pruritus (1%)
Gastrointestinal: Dyspepsia (7%), nausea (7%), gastrointestinal pain (4%), flatulence (2%), vomiting (2%), anorexia (1%)
Hematologic & oncologic: Neutropenia (2%), purpura (2%)
Hepatic: Increased serum alkaline phosphatase (>2 x upper limit of normal: 8%), abnormal hepatic function tests (1%)
<1%, postmarketing, and/or case reports: Agranulocytosis, anaphylaxis, angioedema, aplastic anemia, arthropathy, bone marrow depression, bronchiolitis obliterans organizing pneumonia, conjunctival hemorrhage, ecchymosis, eosinophilia, epistaxis, erythema multiforme, erythema nodosum, exfoliative dermatitis, gastrointestinal hemorrhage, headache, hematuria, hemolytic anemia, hepatic necrosis, hepatitis, hypermenorrhea, hypersensitivity pneumonitis, hyponatremia, increased serum bilirubin, intracranial hemorrhage, immune thrombocytopenia, increased serum creatinine, jaundice, maculopapular rash, myositis, nephrotic syndrome, pain, pancytopenia, peptic ulcer, peripheral neuropathy, positive ANA titer, renal failure, sepsis, serum sickness, Stevens-Johnson syndrome, systemic lupus erythematosus, thrombocythemia, thrombotic thrombocytopenic purpura (TTP), tinnitus, urticaria, vasculitis, weakness
Warnings/Precautions
Concerns related to adverse effects:
- Hematologic toxicity: [US Boxed Warning]: May cause life-threatening hematologic reactions, including neutropenia, agranulocytosis, thrombotic thrombocytopenia purpura (TTP), and aplastic anemia. Routine monitoring is required (see Monitoring Parameters). Monitor for signs and symptoms of neutropenia including WBC count. Discontinue if the absolute neutrophil count falls to <1,200/mm3 or if laboratory signs of TTP or aplastic anemia occur.
- Thienopyridine hypersensitivity: Because of structural similarities, cross-reactivity is possible among the thienopyridines (clopidogrel, prasugrel, and ticlopidine); use with caution or avoid in patients with previous thienopyridine hypersensitivity. Use of ticlopidine is contraindicated in patients with hypersensitivity to ticlopidine.
Disease-related concerns:
- Bleeding disorders: Use with caution in patients with platelet disorders, bleeding disorders and/or at increased risk for bleeding (eg, PUD, trauma, or surgery).
- Hepatic impairment: Use with caution in patients with mild-to-moderate hepatic impairment. Use is contraindicated with severe hepatic impairment.
- Renal impairment: Use with caution in patients with moderate-to-severe renal impairment (experience is limited); bleeding times may be significantly prolonged and the risk of hematologic adverse events (eg, neutropenia) may be increased.
Concurrent drug therapy issues:
- Anticoagulants and platelet aggregation inhibitors: Use with caution in patients receiving either anticoagulants (eg, heparin, warfarin) or other platelet aggregation inhibitors; bleeding risk is increased.
Special populations:
- Lower GI bleed patients: An individualized and multidisciplinary approach should be utilized to determine therapy discontinuation and management in patients with acute lower GI bleed (LGIB) who are on antiplatelet medications; risk of ongoing bleeding should be weighed with risk of thromboembolic events. In patients receiving dual antiplatelet therapy (aspirin plus P2Y12 receptor blocker [eg, clopidogrel, prasugrel, ticagrelor, ticlopidine]) or thienopyridine monotherapy, the thienopyridine should generally be resumed as soon as possible and at least within 7 days, taking into account control of bleeding and cardiovascular risk (aspirin should not be discontinued); however, dual antiplatelet therapy should not be discontinued in the 90 days post-acute coronary syndrome or 30 days post-coronary stenting (Strate 2016).
Other warnings/precautions:
- Coronary artery stents: In patients who have received bare-metal or drug-eluting stents (sirolimus or paclitaxel), premature interruption of antiplatelet therapy may result in stent thrombosis with subsequent fatal and nonfatal myocardial infarction. If ticlopidine is used, duration of therapy, in general, is determined by the type of stent placed (bare metal or drug eluting) and whether an ACS event was ongoing at the time of placement (Levine, 2011).
- Elective surgery: Consider discontinuing 10 to 14 days before elective surgery (except in patients with cardiac stents that have not completed their full course of dual antiplatelet therapy; patient-specific situations need to be discussed with cardiologist; AHA/ACC/SCAI/ACS/ADA Science Advisory provides recommendations).
Monitoring Parameters
Signs of bleeding; CBC with differential at baseline prior to treatment initiation and then weekly for the first 3 months of therapy; more frequent monitoring is recommended for patients whose absolute neutrophil counts have been consistently declining or are 30% less than baseline values. The peak incidence of TTP occurs between 3-4 weeks, the peak incidence of neutropenia occurs at approximately 4-6 weeks, and the incidence of aplastic anemia peaks after 4-8 weeks of therapy. Few cases have been reported after 3 months of treatment. Liver function tests (alkaline phosphatase and transaminases) should be performed in the first 4 months of therapy if liver dysfunction is suspected.
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Teratogenic effects have not been observed in animal reproduction studies; a case report has demonstrated the safe use of ticlopidine in pregnant women (Ueno 2001).
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience nausea or diarrhea. Have patient report immediately to prescriber signs of bleeding (vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any bleeding that is very bad or that will not stop), signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), signs of severe cerebrovascular disease (change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or change in eyesight), signs of infection, pinpoint red spots on skin, severe headache, severe loss of strength and energy, sensing things that seem real but are not, seizures, unable to pass urine, change in amount of urine passed, confusion, severe abdominal pain, or bloody diarrhea (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.