Boxed Warning
Hepatotoxicity:
Because of the risk of potentially fatal acute fulminant liver failure, tolcapone should ordinarily be used in patients with Parkinson disease on L-dopa/carbidopa who are experiencing symptom fluctuations and are not responding satisfactorily to or are not appropriate candidates for other adjunctive therapies.
Because of the risk of liver injury and because tolcapone, when it is effective, provides an observable symptomatic benefit, the patient who fails to show substantial clinical benefit within 3 weeks of initiation of treatment should be withdrawn from tolcapone.
Tolcapone should not be initiated if the patient exhibits clinical evidence of liver disease or 2 ALT or AST values greater than the upper limit of normal. Patients with severe dyskinesia or dystonia should be treated with caution.
Patients who develop evidence of hepatocellular injury while on tolcapone and are withdrawn from the drug for any reason may be at increased risk for liver injury if tolcapone is reintroduced. Accordingly, such patients should not ordinarily be considered for re-treatment.
Cases of severe hepatocellular injury, including fulminant liver failure resulting in death, have been reported in postmarketing use. As of May 2005, 3 cases of fatal fulminant hepatic failure have been reported from more than 40,000 patient-years of worldwide use. This incidence may be 10- to 100-fold higher than the background incidence in the general population. Underreporting of cases may lead to significant underestimation of the increased risk associated with the use of tolcapone. All 3 cases were reported within the first 6 months of initiation of treatment with tolcapone. Analysis of the laboratory monitoring data in over 3,400 tolcapone patients participating in clinical trials indicated that increases in ALT or AST, when present, generally occurred within the first 6 months of treatment with tolcapone.
A prescriber who elects to use tolcapone in the face of the increased risk of liver injury is strongly advised to monitor patients for evidence of emergent liver injury. Patients should be advised of the need for self-monitoring for both the classical signs of liver disease (eg, clay-colored stools, jaundice) and the nonspecific ones (eg, fatigue, loss of appetite, lethargy).
Although a program of frequent laboratory monitoring for evidence of hepatocellular injury is recommended, it is not clear that periodic monitoring of liver enzymes will prevent the occurrence of fulminant liver failure. However, it is generally believed that early detection of drug-induced hepatic injury along with immediate withdrawal of the suspect drug enhances the likelihood for recovery. Accordingly, the following liver monitoring program is recommended.
Before starting treatment with tolcapone, the health care provider should conduct appropriate tests to exclude the presence of liver disease. In patients determined to be appropriate candidates for treatment with tolcapone, ALT and AST levels should be determined at baseline and then periodically (ie, every 2 to 4 weeks) for the first 6 months of therapy. After the first 6 months, periodic monitoring is recommended at intervals deemed clinically relevant. Although more frequent monitoring increases the chances of early detection, the precise schedule for monitoring is a matter of clinical judgment. If the dose is increased to 200 mg 3 times daily, liver enzyme monitoring should take place before increasing the dose and then be conducted every 2 to 4 weeks for the following 6 months of therapy. After 6 months, periodic monitoring is recommended at intervals deemed clinically relevant.
Tolcapone should be discontinued if ALT or AST exceeds 2 times the upper limit of normal (ULN) or if clinical signs and symptoms suggest the onset of hepatic dysfunction (eg, persistent nausea, fatigue, lethargy, anorexia, jaundice, dark urine, pruritus, right upper quadrant tenderness).
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
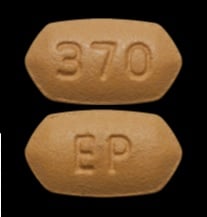
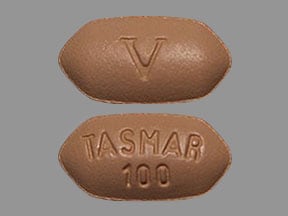
Tablet, Oral:
Tasmar: 100 mg
Generic: 100 mg
Pharmacology
Mechanism of Action
Tolcapone is a selective and reversible inhibitor of catechol-o-methyltransferase (COMT). In the presence of a decarboxylase inhibitor (eg, carbidopa), COMT is the major degradation pathway for levodopa. Inhibition of COMT leads to more sustained plasma levels of levodopa and enhanced central dopaminergic activity.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
9 L
Metabolism
Hepatic, via glucuronidation, to inactive metabolite (>99%)
Excretion
Urine (60% as metabolites; 0.5% as unchanged drug); feces (40%)
Time to Peak
~2 hours
Half-Life Elimination
2 to 3 hours
Protein Binding
>99.9%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
In patients with moderate cirrhotic liver disease, clearance and Vd is reduced about 50%. Do not initiate therapy if the patient exhibits clinical evidence of active liver disease or 2 ALT or AST values greater than the ULN.
Use: Labeled Indications
Adjunct to levodopa and carbidopa for the treatment of signs and symptoms of idiopathic Parkinson disease in patients with motor fluctuations not responsive to other therapies
Contraindications
Hypersensitivity to tolcapone or any component of the formulation; patients with liver disease or a history of tolcapone-induced hepatocellular injury; history of nontraumatic rhabdomyolysis or hyperpyrexia and confusion potentially related to medication
Dosage and Administration
Dosing: Adult
Note: Because of the risk of potentially fatal, acute fulminant liver failure, tolcapone is only appropriate in patients who are experiencing symptom fluctuations while receiving levodopa/carbidopa and who are not responding satisfactorily to or are not appropriate candidates for other adjunctive therapies. If clinical improvement is not observed after 3 weeks of therapy (regardless of dose), tolcapone treatment should be discontinued.
Parkinson disease: Oral: Initial: 100 mg 3 times daily always as an adjunct to levodopa/carbidopa; may increase as tolerated to 200 mg 3 times daily only if clinical benefit is justified (dosage associated with an increased incidence of ALT elevations). Note: Levodopa dose may need to be decreased upon initiation of tolcapone (average reduction in clinical trials was 30%). As many as 70% of patients receiving levodopa doses >600 mg daily required levodopa dosage reduction in clinical trials. Patients with moderate to severe dyskinesia prior to initiation are also more likely to require dosage reduction.
Dosing: Geriatric
Refer to adult dosing.
Administration
May be administered without regard to meals. In clinical studies, the first dose of the day was administered with levodopa/carbidopa, and the subsequent doses were administered 6 hours and 12 hours later.
Dietary Considerations
May be taken without regard to meals.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Tolcapone Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
COMT Substrates: COMT Inhibitors may decrease the metabolism of COMT Substrates. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Monoamine Oxidase Inhibitors: COMT Inhibitors may enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Consider therapy modification
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pipamperone [INT]: COMT Inhibitors may diminish the therapeutic effect of Pipamperone [INT]. Pipamperone [INT] may diminish the therapeutic effect of COMT Inhibitors. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
>10%:
Cardiovascular: Orthostatic hypotension (17%)
Central nervous system: Drowsiness (14% to 32%), sleep disorder (24% to 25%), hallucination (8% to 24%), dystonia (19% to 22%), increased dream activity (16% to 21%), dizziness (6% to 13%), confusion (10% to 11%), headache (10% to 11%)
Gastrointestinal: Nausea (28% to 50%), diarrhea (16% to 34%; severe: 3% to 4%), anorexia (19% to 23%)
Neuromuscular & skeletal: Dyskinesia (42% to 51%), muscle cramps (17% to 18%)
1% to 10%:
Cardiovascular: Syncope (4% to 5%), chest pain (1% to 3%), hypotension (2%), palpitations
Central nervous system: Fatigue (3% to 7%), loss of balance (2% to 3%), paresthesia (1% to 3%), burning sensation (1% to 2%), agitation (1%), euphoria (1%), hyperactivity (1%), malaise (1%), panic (1%), irritability (1%), mental deficiency (1%), depression, emotional lability, flank pain, hypoesthesia, speech disturbance, vertigo
Dermatologic: Diaphoresis (4% to 7%), alopecia (1%), skin rash
Gastrointestinal: Vomiting (8% to 10%), constipation (6% to 8%), abdominal pain (5% to 6%), xerostomia (5% to 6%), dyspepsia (3% to 4%), flatulence (2% to 4%)
Genitourinary: Urinary tract infection (5%), hematuria (4% to 5%), urine discoloration (2% to 3%), urination disorder (1% to 2%), impotence, urinary incontinence
Hematologic & oncologic: Hemorrhage (1%), skin neoplasm (1%), uterine neoplasm (1%)
Hepatic: Increased serum transaminases (1% to 3%; 3 x ULN, usually with first 6 months of therapy)
Infection: Influenza (3% to 4%), infection
Neuromuscular & skeletal: Hyperkinesia (≤3%), hypokinesia (≤3%), muscle rigidity (2%), neck pain (2%), arthritis (1% to 2%), myalgia, rhabdomyolysis, tremor
Ophthalmic: Cataract (1%), ophthalmic inflammation (1%)
Otic: Tinnitus
Respiratory: Upper respiratory tract infection (5% to 7%), dyspnea (3%), sinus congestion (1% to 2%), bronchitis, pharyngitis
Miscellaneous: Fever (1%), accidental injury
<1%, postmarketing, and/or case reports: Abnormal stools, abnormality in thinking, abscess, altered sense of smell, amnesia, anemia, antisocial behavior, apathy, apnea, arteriosclerosis, arthropathy, asthma, bacterial infection, bladder calculus, brain disease, breast neoplasm, carcinoma, cardiovascular signs and symptoms, cellulitis, cerebral ischemia, cerebrovascular accident, change in libido, chills, cholecystitis, cholelithiasis, choreoathetosis, colitis, cough, dehydration, delirium, delusions, dermatological disease, diabetes mellitus, diplopia, disease of the lacrimal apparatus, duodenal ulcer, dysphagia, dysuria, eczema, edema, epistaxis, erythema multiforme, esophagitis, extrapyramidal reaction, eye pain, facial edema, fungal infection, furunculosis, gastric atony, gastroenteritis, gastrointestinal carcinoma, gastrointestinal hemorrhage, genitourinary disease, glaucoma, hemiplegia, hemophthalmos, hernia, herpes simplex infection, herpes zoster, hiccups, hostility, hypercholesteremia, hypersensitivity reaction, hyperventilation, hypoxia, increased thirst, laryngitis, leukemia, manic reaction, meningitis, myoclonus, neoplasm, nephrolithiasis, nervousness, neuralgia, neuropathy, nocturia, oliguria, oral mucosa ulcer, otalgia, otitis media, ovarian carcinoma, pain, paranoia, pericardial effusion, polyuria, prostate carcinoma, prostatic disease, pruritus, psychosis, pulmonary edema, rectal disease, rhinitis, seborrhea, sialorrhea, skin discoloration, surgery, tenosynovitis, thrombocytopenia, thrombosis, tongue disease, twitching, urinary retention, urticaria, uterine atony, uterine disease, uterine hemorrhage, vaginitis, viral infection
Warnings/Precautions
Concerns related to adverse effects:
- Abnormal thinking/behavioral changes: Abnormal thinking and behavior changes have been reported and may include paranoid ideation, delusions, confusion, psychotic-like behavior, disorientation, aggressive behavior, agitation, and delirium.
- CNS depression: Patients have reported falling asleep while engaging in activities of daily living; this has been reported to occur without significant warning signs. Monitor for daytime somnolence or preexisting sleep disorder. Use caution with other CNS depressants, sedating agents, psychoactive drugs, or ethanol. Patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery, driving). Discontinuation of treatment may be required in patients experiencing significant drowsiness.
- Diarrhea: Has been associated with delayed development of diarrhea (onset after 2 to 12 weeks); use with caution in patients with lower gastrointestinal disease or an increased risk of dehydration.
- Hallucinations: May cause hallucinations (onset within 2 weeks), which may improve with reduction in levodopa therapy; incidence may be increased in patients >75 years of age.
- Hematuria: Has been associated with hematuria; ~2% to 5% of patients experienced hematuria in clinical trials.
- Hepatotoxicity: [US Boxed Warning]: Due to reports of fatal liver injury associated with use of this drug, the manufacturer is advising that tolcapone be reserved for patients who are experiencing inadequate symptom control or who are not appropriate candidates for other available treatments. Patients must provide written consent acknowledging the risks of hepatic injury. Close monitoring for potential hepatotoxicity is required during use. Do not initiate in patients with clinical evidence of liver disease or with two transaminases values greater than the upper limit of normal. Discontinue if signs and/or symptoms of hepatic injury are noted (eg, anorexia, jaundice, lethargy, or transaminases >2 times upper limit of normal) or if clinical improvement is not evident after 3 weeks of therapy. Tolcapone should not be reinitiated in patients who discontinued therapy due to evidence of liver injury; may be at increased risk for liver injury.
- Impulse control disorders: Dopaminergic agents used for Parkinson disease or restless legs syndrome have been associated with compulsive behaviors and/or loss of impulse control, which has manifested as pathological gambling, libido increases (hypersexuality), and/or binge eating. Causality has not been established, and controversy exists as to whether this phenomenon is related to the underlying disease, prior behaviors/addictions and/or drug therapy. Dose reduction or discontinuation of therapy has been reported to reverse these behaviors in some, but not all cases.
- Melanoma: Risk for melanoma development is increased in Parkinson disease patients; drug causation or factors contributing to risk have not been established. Patients should be monitored closely and periodic skin examinations should be performed.
- Orthostatic hypotension: May cause orthostatic hypotension and syncope; Parkinson disease patients appear to have an impaired capacity to respond to a postural challenge; use with caution in patients at risk of hypotension (such as those receiving antihypertensive drugs) or where transient hypotensive episodes would be poorly tolerated (cardiovascular disease or cerebrovascular disease). Parkinson patients being treated with dopaminergic agonists ordinarily require careful monitoring for signs and symptoms of postural hypotension, especially during dose escalation, and should be informed of this risk.
- Pleural/retroperitoneal fibrosis: Dopaminergic agents from the ergot class have been associated with fibrotic complications, such as retroperitoneal fibrosis, pulmonary infiltrates or effusion and pleural thickening. It is unknown whether nonergot, pro-dopaminergic agents like tolcapone confer this risk.
- Rhabdomyolysis: Severe rhabdomyolysis has been reported with use.
Disease-related concerns:
- Dyskinesia: Use with caution in patients with preexisting dyskinesias; exacerbation of preexisting dyskinesia has been reported. Levodopa dosage reduction may be required, particularly in patients with levodopa dosages >600 mg daily or with moderate to severe dyskinesia prior to initiation.
- Hepatic impairment: Avoid in patients who have ALT or AST values exceeding two times the upper limit of normal or any other evidence of hepatocellular dysfunction. Use is contraindicated in patients with hepatic impairment.
- Psychotic disorders: Avoid use in patients with a major psychotic disorder; may exacerbate psychosis.
- Renal impairment: Use with caution in patients with severe renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Discontinuation of therapy: Dopaminergic agents have been associated with a syndrome resembling neuroleptic malignant syndrome upon withdrawal or abrupt dosage reduction; patients should be monitored closely if therapy is discontinued.
Monitoring Parameters
Blood pressure; symptoms of Parkinson disease; mental status; periodic skin examinations for melanoma; liver enzymes at baseline and then every 2 to 4 weeks for the first 6 months of therapy; thereafter, periodic monitoring should be conducted as deemed clinically relevant. If the dose is increased to 200 mg 3 times/day, reinitiate LFT monitoring prior to dose increase and then every 2 to 4 weeks for 6 months, and then resume periodic monitoring. Discontinue therapy if the ALT or AST exceeds 2 times ULN or if the clinical signs and symptoms suggest the onset of liver failure.
Pregnancy
Pregnancy Considerations
Adverse events were observed in animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat Parkinson's disease.
Frequently reported side effects of this drug
- Headache
- Sweating a lot
- Trouble sleeping
- Lack of appetite
- Diarrhea
- Nausea
- Vomiting
- Constipation
- Abdominal pain
- Urine discoloration
- Common cold symptoms
- Dry mouth
- Loss of strength and energy.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Severe fatigue
- Narcolepsy
- Confusion
- Severe dizziness
- Passing out
- Behavioral changes
- Sensing things that seem real but are not
- Mood changes
- Muscle pain
- Muscle weakness
- Dark urine
- Trouble passing urine
- Uncontrollable urges
- Skin growths
- Mole changes
- Abnormal movements
- Nightmares
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.