Boxed Warning
Treatment initiation and monitoring (Samsca):
Tolvaptan (Samsca) should be initiated and reinitiated in patients only in a hospital where serum sodium can be closely monitored.
Too rapid correction of hyponatremia (eg, more than 12 mEq/L per 24 hours) can cause osmotic demyelination, resulting in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma, and/or death. In susceptible patients, including those with severe malnutrition, alcoholism, or advanced liver disease, slower rates of correction may be advisable.
Use of tolvaptan for autosomal dominant polycystic kidney disease outside of FDA-approved REMS:
Because of the risk of hepatotoxicity, tolvaptan (Samsca) should not be used for autosomal dominant polycystic kidney disease (ADPKD) outside of the FDA-approved REMS.
Risk of serious liver injury (Jynarque):
Tolvaptan (Jynarque) can cause serious and potentially fatal liver injury. Acute liver failure requiring liver transplantation has been reported.
Measure ALT, AST, and bilirubin before initiating treatment, at 2 weeks and 4 weeks after initiation, then monthly for the first 18 months and every 3 months thereafter. Prompt action in response to laboratory abnormalities, signs, or symptoms indicative of hepatic injury can mitigate, but not eliminate, the risk of serious hepatotoxicity.
Distribution program (Jynarque):
Because of the risk of serious liver injury, tolvaptan (Jynarque) is available only through a restricted distribution program under a Risk Evaluation and Mitigation Strategy (REMS) called the Jynarque REMS Program.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
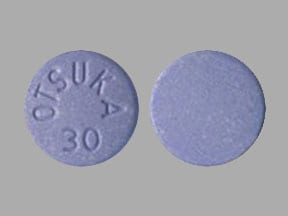
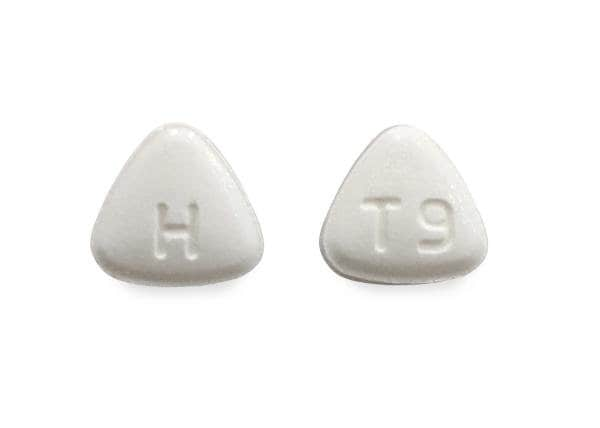
Tablet, Oral:
Jynarque: 15 mg, 30 mg [contains corn starch, fd&c blue #2 aluminum lake]
Samsca: 15 mg, 30 mg [contains fd&c blue #2 aluminum lake]
Tablet Therapy Pack, Oral:
Jynarque: 45 & 15 MG (14 ea); 60 & 30 MG (14 ea); 90 & 30 MG (14 ea) [contains corn starch, fd&c blue #2 aluminum lake]
Pharmacology
Mechanism of Action
An arginine vasopressin (AVP) receptor antagonist with affinity for AVP receptor subtypes V2 and V1a in a ratio of 29:1. Antagonism of the V2 receptor by tolvaptan promotes the excretion of free water (without loss of serum electrolytes) resulting in net fluid loss, increased urine output, decreased urine osmolality, and subsequent restoration of normal serum sodium levels.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: ~3 L/kg
Metabolism
Almost exclusively hepatic via CYP3A4 (none are pharmacodynamically active)
Excretion
Feces: 59% (19% as unchanged drug); Urine: 40% (<1% as unchanged drug)
Onset of Action
Aquaretic and sodium increasing effects (Samsca): 2 to 4 hours
Peak effect: Aquaretic and sodium increasing effects (Samsca): 4 to 8 hours
Time to Peak
Plasma: 2 to 4 hours
Duration of Action
Aquaretic and sodium increasing effects (Samsca): 60% peak serum sodium elevation is retained at 24 hours; urinary excretion of free water is no longer elevated
Half-Life Elimination
15 mg doses: 3 hours; ≥120 mg doses: ~12 hours. Note: Half-life increases with higher doses due to a more prolonged absorption.
Protein Binding
>98%
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC and Cmax were increased 90% and 10%, respectively, in patients with CrCl <30 mL/minute compared to patients with CrCl >60 mL/minute.
Special Populations: Hepatic Function Impairment
Moderate (Child-Pugh class A and B) or severe hepatic impairment (Child-Pugh class C) decreases the clearance and increases the volume of distribution of tolvaptan.
Use: Labeled Indications
Autosomal dominant polycystic kidney disease: Jynarque, Jinarc [Canadian product]: Slow the progression of kidney function decline in adults at risk of rapidly progressing autosomal dominant polycystic kidney disease (ADPKD)
Hypervolemic or euvolemic hyponatremia: Samsca: Treatment of clinically significant hypervolemic or euvolemic hyponatremia (serum sodium <125 mEq/L or less marked hyponatremia that is symptomatic and resistant to fluid restriction), including patients with heart failure and syndrome of inappropriate antidiuretic hormone (SIADH).
Limitations of use: Not indicated for use when urgent treatment of hyponatremia is required to prevent or treat serious neurological symptoms. It has not been established that raising serum sodium with tolvaptan provides symptomatic benefit.
Contraindications
Hypersensitivity (eg, anaphylactic shock, generalized rash) to tolvaptan or any component of the formulation; concurrent use with strong CYP3A inhibitors (eg, clarithromycin, indinavir, itraconazole, ketoconazole, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin); use in patients unable to sense or appropriately respond to thirst; anuria
Samsca: Additional contraindications: Hypovolemic hyponatremia; urgent need to raise serum sodium acutely; use in patients with autosomal dominant polycystic kidney disease (ADPKD) outside of the FDA-approved REMS
Samsca [Canadian product]: Additional contraindications: Hypersensitivity to benzazepine or benzazepine derivatives (eg, mirtazapine); hypovolemic hyponatremia; hypernatremia; urgent need to raise serum sodium acutely; use in patients with ADPKD outside of Health Canada Risk Management Plan (RMP); pregnancy; breastfeeding; galactose intolerance, Lapp lactase deficiency; glucose-galactose malabsorption
Jynarque: Additional contraindications: Patients with a history, signs, or symptoms of significant liver impairment or injury (not applicable to uncomplicated polycystic liver disease); use in patients with uncorrected abnormal blood sodium concentrations; uncorrected urinary outflow obstruction; hypovolemia
Jinarc [Canadian product]: Additional contraindications: Patients with a history of tolvaptan discontinuation; hypersensitivity to benzazepine or benzazepine derivatives (eg, mirtazapine); hypovolemia; hypernatremia; use in patients who do not have access to fluids; patients with a history, signs, or symptoms of significant liver impairment or injury (not applicable to uncomplicated polycystic liver disease); pregnancy; breastfeeding; galactose intolerance, Lapp lactase deficiency; glucose-galactose malabsorption
Dosage and Administration
Dosing: Adult
Autosomal dominant polycystic kidney disease (ADPKD): Jynarque, Jinarc [Canadian product]: Oral: Initial: 60 mg/day in divided doses (given as 45 mg upon wakening and 15 mg 8 hours later); titrate per response and tolerability at intervals of at least 7 days between titrations to 90 mg/day in divided doses (given as 60 mg upon wakening and 30 mg 8 hours later) followed by 120 mg/day in divided doses (given as 90 mg upon wakening and 30 mg 8 hours later). Maintain urine osmolality of <300 mOsm/kg if possible; if the maximum dose is not tolerated, administration of a lower dose with the goal of achieving urine osmolarity of 250 to 300 mOsm/kg is reasonable (Devuyst 2017).
Hypervolemic or euvolemic hyponatremia: Samsca: Oral: Initial: 15 mg once daily; after at least 24 hours, may increase to 30 mg once daily to a maximum of 60 mg once daily titrating at 24-hour intervals to desired serum sodium concentration. Avoid fluid restriction during the first 24 hours of therapy. Do not use for more than 30 days due to the risk of hepatotoxicity.
Dosage adjustment with concomitant medication:
Moderate CYP3A inhibitors (eg, aprepitant, erythromycin, fluconazole, verapamil):
Samsca: Avoid use.
Jynarque, Jinarc [Canadian product]:
Patients receiving tolvaptan 120 mg/day: Reduce dose to 60 mg/day [45 mg + 15 mg].
Patients receiving 90 mg/day: Reduce dose to 45 mg/day [30 mg + 15 mg].
Patients receiving 60 mg/day: Reduce dose to 30 mg/day [15 mg + 15 mg].
If reduced dose is not tolerated, further dose reduction may be necessary. Interrupt treatment temporarily for short term therapy with moderate CYP3A inhibitors if the recommended reduced doses are not available.
Strong CYP3A inhibitors (eg, ketoconazole, clarithromycin, ritonavir, saquinavir): Samsca, Jynarque: Use is contraindicated.
Strong CYP3A inducers (eg, rifampin, barbiturates, phenytoin, carbamazepine, St John's Wort):
Jynarque, Jinarc [Canadian product]: Avoid use.
Samsca: Avoid use. If concurrent use is necessary, monitor patient response and increase tolvaptan dose as necessary.
P-gp inhibitors (eg, cyclosporine, quinidine): Dose reduction of tolvaptan may be necessary.
Dosing: Geriatric
Refer to adult dosing.
Administration
Oral: May be administered without regards to meals. Water should be available at all times during use and patients encouraged to drink to avoid thirst and prevent dehydration from occurring. Interrupt therapy if the ability to drink or accessibility to water is limited.
Samsca: Treatment should be initiated or reinitiated in a hospital.
Nasogastric (NG) tube: Administration via NG tube resulted in an ~25% reduction in AUC and a modest reduction in Cmax in one study; 24-hour urine output was reduced by only 2.8%. Therefore, until further studies are done to determine a bioequivalent dose when administering via NG tube, NG tube administration of a crushed 15 mg tablet appears to be a viable alternative method of administration (McNeely 2012).
Dietary Considerations
Grapefruit juice may increase tolvaptan serum concentrations. Management: Avoid concurrent use with grapefruit juice.
Storage
Jynarque: Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F).
Samsca: Store at 25°C (77°F); excursions permitted between 15°C and 30°C (59°F and 86°F).
Tolvaptan Images
Drug Interactions
Angiotensin II Receptor Blockers: Tolvaptan may enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Tolvaptan may enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
BCRP/ABCG2 Substrates: Tolvaptan may increase the serum concentration of BCRP/ABCG2 Substrates. Consider therapy modification
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Tolvaptan. Management: If concurrent use is necessary, increased doses of tolvaptan (with close monitoring for toxicity and clinical response) may be needed. Avoid combination
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Tolvaptan. Management: Jynarque dose requires adjustment when used with a moderate CYP3A4 inhibitor. See labeling or full interaction monograph for specific recommendations. Use of Samsca with moderate CYP3A4 ihibitors should generally be avoided. Consider therapy modification
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Tolvaptan. Avoid combination
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Desmopressin: Tolvaptan may diminish the therapeutic effect of Desmopressin. Avoid combination
Digoxin: Tolvaptan may increase the serum concentration of Digoxin. Monitor therapy
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
GlyBURIDE: Tolvaptan may increase the serum concentration of GlyBURIDE. Consider therapy modification
Grapefruit Juice: May increase the serum concentration of Tolvaptan. Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
OAT1/3 Substrates: Tolvaptan may increase the serum concentration of OAT1/3 Substrates. Management: Patients being treated with the Jynarque brand of tolvaptan should avoid concomitant use of OAT1/3 substrates. Concentrations and effects of the OAT1/3 substrate would be expected to increase with any combined use. Consider therapy modification
OATP1B1/1B3 (SLCO1B1/1B3) Substrates: Tolvaptan may increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Potassium-Sparing Diuretics: Tolvaptan may enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Sodium Chloride: May enhance the adverse/toxic effect of Tolvaptan. Specifically, Hypertonic Saline may increase the risk for too rapid of an increase in serum sodium concentrations. Management: This interaction is specific to Hypertonic Saline. Avoid concurrent use of Hypertonic Saline with Tolvaptan. Avoid combination
St John's Wort: May decrease the serum concentration of Tolvaptan. Management: If concurrent use is necessary, increased doses of tolvaptan (with close monitoring for toxicity and clinical response) may be needed. Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Fatigue (14%), dizziness (11%)
Endocrine & metabolic: Increased thirst (12% to 64%)
Gastrointestinal: Nausea (21%), xerostomia (7% to 16%), diarrhea (13%)
Renal: Polyuria (including pollakiuria, 4% to 70%)
1% to 10%:
Cardiovascular: Palpitations (4%), cerebrovascular accident (<2%), deep vein thrombosis (<2%), intracardiac thrombus (<2%), pulmonary embolism (<2%), ventricular fibrillation (<2%)
Dermatologic: Xeroderma (5%), skin rash (4%)
Endocrine & metabolic: Increased serum sodium (2% to 7%), hyperglycemia (6%), hyperuricemia (4%), hypernatremia (≤4%), dehydration (2% to 3%), hypovolemia (2%), diabetic ketoacidosis (<2%)
Gastrointestinal: Gastrointestinal hemorrhage (cirrhosis patients, 10%), dyspepsia (8%), constipation (7%), decreased appetite (7%), abdominal distention (5%), anorexia (4%), ischemic colitis (<2%)
Genitourinary: Urethral bleeding (<2%), vaginal hemorrhage (<2%)
Hematologic & oncologic: Disseminated intravascular coagulation (<2%), prolonged prothrombin time (<2%)
Hepatic: Increased serum alanine aminotransferase (5%)
Neuromuscular & skeletal: Asthenia (9%), rhabdomyolysis (<2%)
Respiratory: Respiratory failure (<2%)
Miscellaneous: Fever (4%)
<1%, postmarketing, and/or case reports: Anaphylactic shock, anaphylaxis, hepatic failure, hepatotoxicity, hyperkalemia, hypersensitivity reaction, increased serum bilirubin, osmotic demyelination syndrome, skin rash
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: Dizziness, asthenia, and/or syncope have been reported when used for autosomal dominant polycystic kidney disease (ADPKD); advise patients to use caution when performing dangerous tasks (eg, driving, operating machinery).
- Hepatotoxicity: Tolvaptan may increase the risk of serious hepatotoxicity, including fatal hepatotoxicity.
- ADPKD patients: Cases of hepatotoxicity have been reported in patients treated for ADPKD generally during the first 18 months of therapy; liver failure resulting in liver transplantation has also been reported. During use, if signs/symptoms of hepatotoxicity develop or if ALT, AST, or bilirubin increase to >2 times ULN, immediately discontinue use, obtain repeat tests promptly within 48 to 72 hours, and continue testing as necessary; if laboratory abnormalities stabilize or resolve, treatment may be reinitiated with increased monitoring as long as ALT and AST <3 times ULN. Do not reinitiate therapy in patients with signs or symptoms of hepatic injury or ALT or AST >3 times ULN, unless there is another reason for liver injury and the liver injury has resolved. Patients with a stable, low baseline ALT or AST that experience an increase >2 times ULN (or an increase less than 2 times ULN) may be experiencing early liver injury; discontinuation of therapy may be necessary and repeat liver tests prior to reinitiation with increased monitoring.
- Hypervolemic or euvolemic hyponatremia patients: Treatment should be limited to 30 days. Avoid use in patients with liver disease (including cirrhosis) since the ability to recover from further liver injury may be impaired. During use, if signs/symptoms of hepatotoxicity develop, discontinue use.
- Hypovolemia/dehydration: Patients should ingest fluids in response to thirst during therapy. Interrupt or discontinue therapy in patients who develop significant signs or symptoms of hypovolemia.
- Serum sodium monitoring/initiating in hospital: [US Boxed Warning]: Samsca: Tolvaptan should be initiated and reinitiated in patients only in a hospital where serum sodium can be closely monitored. Too rapid correction of hyponatremia (ie, >12 mEq/L/24 hours) can cause osmotic demyelination resulting in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma, and death. In susceptible patients (including those with severe malnutrition, alcoholism, or advanced liver disease), slower rates of correction may be advisable. Patients with SIADH, very low baseline, or patients who are fluid restricted during the first 24 hours of therapy may be at greater risk of overly-rapid correction. Avoid fluid restriction during the initial 24 hours of therapy. Discontinue or interrupt therapy if sodium correction is too rapid and consider administration of hypotonic fluids.
Disease-related concerns:
- Hepatic impairment:
- ADPKD patients: Use is contraindicated in patients with significant hepatic impairment or disease (or a history of).
- Hypervolemic or euvolemic hyponatremia patients: Avoid use in patients with liver disease, including those with cirrhosis, since the ability to recover from further liver injury may be impaired. In addition, patients with cirrhosis have a higher risk of gastrointestinal bleeding.
- Hyperkalemia: Reductions in extracellular fluid volumes may cause hyperkalemia. Patients using concomitant medications that may increase potassium levels or with a pretreatment serum potassium >5 mEq/L should be monitored after initiation of therapy.
- Renal impairment: Use is contraindicated in patients who are anuric. In patients with hypervolemic or euvolemic hyponatremia, use is not recommended in patients with CrCl <10 mL/minute; has not been studied and effects of tolvaptan on serum sodium levels is likely lost at very low levels of renal function. In patients with ADPKD, studies have included patients with normal and reduced renal function.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use:
- ADPKD patients: Patients most likely to benefit from therapy are those with rapidly progressive disease or those who are developing progressive disease but lack extensive renal damage. Factors associated with rapid progression include large total renal cyst mass for a given age (measured by total kidney volume), chronic kidney disease stage 2 to 3, rapid deterioration of renal function, systemic hypertension or albuminuria.
- Hypervolemic or euvolemic hyponatremia patients: Monitor closely for rate of serum sodium increase and neurological status; rapid serum sodium correction (>12 mEq/L/24 hours) can lead to permanent neurological damage. Discontinue use if rate of serum sodium increase is undesirable; fluid restriction during the first 24 hours of sodium correction can increase the risk of overly-rapid correction and should generally be avoided; not intended for urgent correction of serum sodium to prevent or treat serious neurologic symptoms; it has not been demonstrated that raising serum sodium with tolvaptan provides a symptomatic benefit.
- Limitations of use: SIADH: Limitations to the use of tolvaptan in SIADH may exist due to concerns about safety, such as overly rapid correction of hyponatremia and potential for hepatotoxicity (Spasovski 2014). Based on available evidence, European clinical practice guidelines recommend against the use of vasopressin receptor antagonists in the treatment of hyponatremia in patients with SIADH (Spasovski 2014). Additional data may be necessary to define the appropriate clinical role of tolvaptan in this condition.
- REMS program [US Boxed Warning]: Jynarque: Because of the risk of serious liver injury, tolvaptan is available only through a restricted distribution program under a Risk Evaluation and Mitigation Strategy (REMS) called the Jynarque REMS Program. Prescribers must be certified by enrolling in the REMS program and must inform patients about the risk of hepatotoxicity associated with Jynarque and how to recognize symptoms of hepatotoxicity; patients must be enrolled in the REMS program and follow monitoring requirements; and pharmacies must be certified by enrolling in the REMS program and only dispense to patients authorized to receive Jynarque. Call 1-877-726-7220 or visit http://www.jynarquerems.com for more information.
Monitoring Parameters
Serum sodium concentration, rate of serum sodium increase, serum potassium concentration (if >5 mEq/L prior to administration or receiving medications known to elevate serum potassium); volume status; and/or signs of drug-induced hepatotoxicity (eg, anorexia, fatigue, right upper abdominal discomfort, jaundice, dark urine, itching); neurologic status (at initiation and after titration)
Additional monitoring recommendations: Jynarque: Hepatic function (ALT, AST, and bilirubin) prior to initiation, at 2 and 4 weeks after initiation, monthly for 18 months, and every 3 months thereafter
Additional monitoring recommendations: Jinarc [Canadian product]: Hepatic function testing prior to therapy initiation, monthly for the first 18 months, then every 3 months for 12 months, and then every 3 to 6 months during therapy. Urine osmolality or specific gravity (trough level prior to morning dose); serum uric acid (prior to initiation and as indicated during therapy
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events were observed in animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat low sodium levels.
- It is used to slow the progress of kidney problems in some people.
Frequently reported side effects of this drug
- Thirst
- Loss of strength and energy
- Constipation
- Dry mouth
- Passing a lot of urine
- Diarrhea
- Lack of appetite
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, severe dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, unable to pass urine or change in amount of urine passed, dry mouth, dry eyes, nausea, or vomiting
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Difficulty speaking
- Difficulty swallowing
- Fatigue
- Confusion
- Mood changes
- Abnormal movements
- Seizures
- Muscle weakness
- Dizziness
- Weight loss
- Difficulty walking
- Black, tarry, bloody stools
- Vomiting blood
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.