Boxed Warning
Fetal toxicity:
When pregnancy is detected, discontinue trandolapril/verapamil as soon as possible. Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, variable release: Trandolapril 2 mg [immediate release] and verapamil hydrochloride 180 mg [sustained release]; Trandolapril 2 mg [immediate release] and verapamil hydrochloride 240 mg [sustained release]; Trandolapril 4 mg [immediate release] and verapamil hydrochloride 240 mg [sustained release]
Tarka:
1/240: Trandolapril 1 mg [immediate release] and verapamil hydrochloride 240 mg [sustained release] [DSC]
2/180: Trandolapril 2 mg [immediate release] and verapamil hydrochloride 180 mg [sustained release]
2/240: Trandolapril 2 mg [immediate release] and verapamil hydrochloride 240 mg [sustained release]
4/240: Trandolapril 4 mg [immediate release] and verapamil hydrochloride 240 mg [sustained release]
Pharmacology
Mechanism of Action
Trandolapril: Trandolapril is an ACE inhibitor that prevents the formation of angiotensin II from angiotensin I. Trandolapril must undergo enzymatic hydrolysis, mainly in liver, to its biologically active metabolite, trandolaprilat. A CNS mechanism may also be involved in the hypotensive effect as angiotensin II increases adrenergic outflow from the CNS. Vasoactive kallikreins may be decreased in conversion to active hormones by ACE inhibitors, thus reducing blood pressure.
Verapamil: Inhibits calcium ion from entering the "slow channels" or select voltage-sensitive areas of vascular smooth muscle and myocardium during depolarization; produces relaxation of coronary vascular smooth muscle and coronary vasodilation; increases myocardial oxygen delivery in patients with vasospastic angina; slows automaticity and conduction of AV node.
Use: Labeled Indications
Hypertension: Management of hypertension
Contraindications
Hypersensitivity to trandolapril, verapamil, or any component of the formulation; severe left ventricular dysfunction; hypotension (systolic pressure <90 mm Hg); cardiogenic shock; sick sinus syndrome (except in patients with a functioning pacemaker); atrial flutter or atrial fibrillation with an accessory bypass tract (eg, Wolff-Parkinson-White, Lown-Ganong-Levine syndromes); history of angioedema related to previous treatment with an ACE inhibitor; coadministration with or within 36 hours of switching to or from a neprilysin inhibitor (eg, sacubitril); second- or third-degree AV block (except in patients with a functioning pacemaker); coadministration with aliskiren in patients with diabetes; coadministration with flibanserin
Documentation of allergenic cross-reactivity for Angiotensin-Converting Enzyme Inhibitors and Calcium Channel Blockers. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Complicated MI (ventricular failure manifested by pulmonary congestion); marked bradycardia; hypotensive or hemodynamically unstable states; hemodynamically significant bilateral artery stenosis or severe artery stenosis of a solitary functioning kidney; severe renal impairment (CrCl <30 mL/minute); dialysis; hepatic cirrhosis with ascites; concomitant use with ACE inhibitors or angiotensin receptor blockers (ARBs) medications in patients with type 1 or 2 diabetes mellitus, moderate to severe renal impairment (GFR <60 mL/minute/1.73 m2), hyperkalemia (>5 mMol/L), or with heart failure who are hypotensive; concomitant use with aliskiren in patients with moderate to severe renal impairment (GFR <60 mL/minute/1.73 m2), hyperkalemia (>5 mMol/L), or with heart failure who are hypotensive; concomitant use with intravenous beta-adrenergic antagonists (except in an intensive care unit); concomitant use with ivabradine; hereditary/idiopathic angioedema; women who are pregnant, planning to become pregnant, or women of childbearing potential and not using adequate contraception; breastfeeding; children and adolescents <18 years of age
Dosage and Administration
Dosing: Adult
Note: Not for initial therapy; dose is individualized; may be substituted for individual components in patients currently maintained on both agents separately.
Hypertension: Oral: Trandolapril 1 to 4 mg/verapamil 180 to 240 mg once daily.
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer orally with food.
Dietary Considerations
Use potassium-containing salt substitutes cautiously in patients with diabetes, renal impairment, or those maintained on potassium supplements or potassium-sparing diuretics.
Storage
Store at 15°C to 25°C (59°F to 77°F).
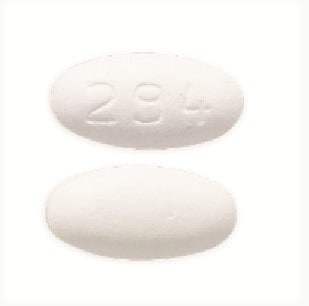
Trandolapril and Verapamil Images
Drug Interactions
Abemaciclib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Abemaciclib. Monitor therapy
Acalabrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Acalabrutinib. Management: Reduce acalabrutinib dose to 100 mg once daily with concurrent use of a moderate CYP3A4 inhibitor. Monitor patient closely for both acalabrutinib response and evidence of adverse effects with any concurrent use. Consider therapy modification
Afatinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Afatinib. Management: Reduce afatinib by 10 mg if not tolerated. Some non-US labeling recommends avoiding combination if possible. If used, administer the P-gp inhibitor simultaneously with or after the dose of afatinib. Consider therapy modification
Alcohol (Ethyl): Verapamil may increase the serum concentration of Alcohol (Ethyl). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Aliskiren: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Aliskiren may enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Aliskiren may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Management: Aliskiren use with ACEIs or ARBs in patients with diabetes is contraindicated. Combined use in other patients should be avoided, particularly when CrCl is less than 60 mL/min. If combined, monitor potassium, creatinine, and blood pressure closely. Consider therapy modification
Allopurinol: Angiotensin-Converting Enzyme Inhibitors may enhance the potential for allergic or hypersensitivity reactions to Allopurinol. Consider therapy modification
Alpha1-Blockers: May enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Alteplase: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Alteplase. Specifically, the risk for angioedema may be increased. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amiodarone: Calcium Channel Blockers (Nondihydropyridine) may enhance the bradycardic effect of Amiodarone. Sinus arrest has been reported. Monitor therapy
AmLODIPine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of AmLODIPine. Monitor therapy
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Angiotensin II: Angiotensin-Converting Enzyme Inhibitors may enhance the therapeutic effect of Angiotensin II. Monitor therapy
Angiotensin II Receptor Blockers: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Angiotensin II Receptor Blockers may increase the serum concentration of Angiotensin-Converting Enzyme Inhibitors. Management: In US labeling, use of telmisartan and ramipril is not recommended. It is not clear if any other combination of an ACE inhibitor and an ARB would be any safer. Consider alternatives to the combination when possible. Consider therapy modification
Antifungal Agents (Azole Derivatives, Systemic): May enhance the adverse/toxic effect of Calcium Channel Blockers. Specifically, itraconazole may enhance the negative inotropic effects of verapamil or diltiazem. Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Calcium Channel Blockers. Fluconazole and isavuconazonium likely exert weaker effects than other azoles and are addressed in separate monographs. Management: Concurrent use of felodipine or nisoldipine with itraconazole is specifically contraindicated. Frequent monitoring is warranted with any such combination; calcium channel blocker dose reductions may be required. Exceptions: Fluconazole; Isavuconazonium Sulfate. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Apixaban: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Apixaban. Monitor therapy
Aprepitant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Aprepitant. Avoid combination
Aprotinin: May diminish the antihypertensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
ARIPiprazole: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Aspirin: Calcium Channel Blockers (Nondihydropyridine) may enhance the antiplatelet effect of Aspirin. Monitor therapy
Asunaprevir: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Asunaprevir. Avoid combination
AtorvaSTATin: May increase the serum concentration of Verapamil. Verapamil may increase the serum concentration of AtorvaSTATin. Management: Consider using lower atorvastatin doses when used together with verapamil. Consider therapy modification
Atosiban: Calcium Channel Blockers may enhance the adverse/toxic effect of Atosiban. Specifically, there may be an increased risk for pulmonary edema and/or dyspnea. Monitor therapy
Avanafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Avanafil. Management: The maximum avanafil adult dose is 50 mg per 24-hour period when used together with a moderate CYP3A4 inhibitor. Patients receiving such a combination should also be monitored more closely for evidence of adverse effects. Consider therapy modification
Avapritinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Avapritinib. Management: Avoid use of moderate CYP3A4 inhibitors with avapritinib. If this combination cannot be avoided, reduce the avapritinib dose from 300 mg once daily to 100 mg once daily. Consider therapy modification
Axitinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Axitinib. Monitor therapy
AzaTHIOprine: Angiotensin-Converting Enzyme Inhibitors may enhance the myelosuppressive effect of AzaTHIOprine. Monitor therapy
Barbiturates: May increase the metabolism of Calcium Channel Blockers. Management: Monitor for decreased therapeutic effects of calcium channel blockers with concomitant barbiturate therapy. Calcium channel blocker dose adjustments may be necessary. Nimodipine Canadian labeling contraindicates concomitant use with phenobarbital. Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benzhydrocodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Benzhydrocodone. Specifically, the concentration of hydrocodone may be increased. Monitor therapy
Beta-Blockers: Calcium Channel Blockers (Nondihydropyridine) may enhance the hypotensive effect of Beta-Blockers. Bradycardia and signs of heart failure have also been reported. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Beta-Blockers. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Betrixaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Betrixaban. Management: Decrease the adult betrixaban dose to an initial single dose of 80 mg followed by 40 mg once daily if combined with a P-glycoprotein inhibitor. Consider therapy modification
Bilastine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Bilastine. Management: Consider alternatives when possible; bilastine should be avoided in patients with moderate to severe renal insufficiency who are receiving p-glycoprotein inhibitors. Consider therapy modification
Blonanserin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Blonanserin. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bosentan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bosentan. Management: Concomitant use of both a CYP2C9 inhibitor and a CYP3A inhibitor or a single agent that inhibits both enzymes with bosentan is likely to cause a large increase in serum concentrations of bosentan and is not recommended. See monograph for details. Monitor therapy
Bosutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bosutinib. Avoid combination
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Brexpiprazole: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Brexpiprazole. Management: The brexpiprazole dose should be reduced to 25% of usual if used together with both a moderate CYP3A4 inhibitor and a strong or moderate CYP2D6 inhibitor, or if a moderate CYP3A4 inhibitor is used in a CYP2D6 poor metabolizer. Monitor therapy
Brigatinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with moderate CYP3A4 inhibitors when possible. If such a combination cannot be avoided, reduce the dose of brigatinib by approximately 40% (ie, from 180 mg to 120 mg, from 120 mg to 90 mg, or from 90 mg to 60 mg). Consider therapy modification
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromocriptine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bromocriptine. Management: The bromocriptine dose should not exceed 1.6 mg daily with use of a moderate CYP3A4 inhibitor. The Cycloset brand specifically recommends this dose limitation, but other bromocriptine products do not make such specific recommendations. Consider therapy modification
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Budesonide (Systemic): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Budesonide (Systemic). Avoid combination
Budesonide (Topical): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Budesonide (Topical). Management: Per US prescribing information, avoid this combination. Canadian product labeling does not recommend strict avoidance. If combined, monitor for excessive glucocorticoid effects as budesonide exposure may be increased. Consider therapy modification
BusPIRone: Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of BusPIRone. Monitor therapy
Calcium Channel Blockers (Dihydropyridine): May enhance the hypotensive effect of Calcium Channel Blockers (Nondihydropyridine). Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
Calcium Salts: May diminish the therapeutic effect of Calcium Channel Blockers. Monitor therapy
Cannabidiol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cannabidiol. Monitor therapy
Cannabis: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be increased. Monitor therapy
CarBAMazepine: Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Calcium Channel Blockers (Nondihydropyridine). Management: Consider empiric reductions in carbamazepine dose with initiation of nondihydropyridine calcium channel blockers. Monitor for increased toxic effects of carbamazepine and reduced therapeutic effects of the calcium channel blocker. Consider therapy modification
Cardiac Glycosides: Calcium Channel Blockers (Nondihydropyridine) may enhance the AV-blocking effect of Cardiac Glycosides. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Celiprolol: Verapamil may enhance the bradycardic effect of Celiprolol. Verapamil may increase the serum concentration of Celiprolol. Management: Concomitant use of verapamil and celiprolol is not recommended, particularly in patients with pre-existing conduction abnormalities. When switching from one agent to the other, a drug-free period is recommended, and heart rate should be monitored closely. Consider therapy modification
Ceritinib: Bradycardia-Causing Agents may enhance the bradycardic effect of Ceritinib. Management: If this combination cannot be avoided, monitor patients for evidence of symptomatic bradycardia, and closely monitor blood pressure and heart rate during therapy. Exceptions are discussed in separate monographs. Consider therapy modification
Cilostazol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cilostazol. Management: Consider reducing the cilostazol dose to 50 mg twice daily in adult patients who are also receiving moderate inhibitors of CYP3A4. Consider therapy modification
Cimetidine: May increase the serum concentration of Calcium Channel Blockers. Management: Consider alternatives to cimetidine. If no suitable alternative exists, monitor for increased effects of calcium channel blockers following cimetidine initiation/dose increase, and decreased effects following cimetidine discontinuation/dose decrease. Consider therapy modification
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CloNIDine: May enhance the AV-blocking effect of Calcium Channel Blockers (Nondihydropyridine). Sinus node dysfunction may also be enhanced. Monitor therapy
Clopidogrel: Calcium Channel Blockers may diminish the therapeutic effect of Clopidogrel. Monitor therapy
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Cobimetinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cobimetinib. Management: Avoid the concomitant use of cobimetinib and moderate CYP3A4 inhibitors. If concurrent short term (14 days or less) use cannot be avoided, reduce the cobimetinib dose to 20 mg daily. Avoid combination
Codeine: CYP3A4 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
Colchicine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Colchicine. Management: Reduce colchicine dose as directed when using with a moderate CYP3A4 inhibitor, and increase monitoring for colchicine-related toxicity. See full monograph for details. Use extra caution in patients with impaired renal and/or hepatic function. Consider therapy modification
Colchicine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a p-glycoprotein inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CycloSPORINE (Systemic): Calcium Channel Blockers (Nondihydropyridine) may decrease the metabolism of CycloSPORINE (Systemic). CycloSPORINE (Systemic) may decrease the metabolism of Calcium Channel Blockers (Nondihydropyridine). Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
CYP3A4 Substrates (High risk with Inhibitors): CYP3A4 Inhibitors (Moderate) may decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Exceptions: Alitretinoin (Systemic); Praziquantel; Trabectedin; Vinorelbine. Monitor therapy
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inhibitors may increase serum concentrations of the active metabolite(s) of Dabigatran Etexilate. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dantrolene: May enhance the hyperkalemic effect of Calcium Channel Blockers (Nondihydropyridine). Dantrolene may enhance the negative inotropic effect of Calcium Channel Blockers (Nondihydropyridine). Management: This interaction has only been described with intravenous dantrolene administration. Avoid combination
Dapoxetine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Dapoxetine. Management: The dose of dapoxetine should be limited to 30 mg per day when used together with a moderate inhibitor of CYP3A4. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deflazacort: CYP3A4 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Deflazacort. Management: Administer one third of the recommended deflazacort dose when used together with a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dipeptidyl Peptidase-IV Inhibitors: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Specifically, the risk of angioedema may be increased. Monitor therapy
Disopyramide: Verapamil may enhance the adverse/toxic effect of Disopyramide. Of particular concern is the potential for profound depression of myocardial contractility. Management: Concurrent use of disopyramide within 48 hours prior to or 24 hours after verapamil should be avoided. Avoid combination
Dofetilide: Verapamil may increase the serum concentration of Dofetilide. Avoid combination
Domperidone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Domperidone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
DOXOrubicin (Conventional): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to moderate CYP3A4 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Dronabinol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Dronabinol. Monitor therapy
Dronedarone: Calcium Channel Blockers (Nondihydropyridine) may enhance the AV-blocking effect of Dronedarone. Other electrophysiologic effects of Dronedarone may also be increased. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Dronedarone. Dronedarone may increase the serum concentration of Calcium Channel Blockers (Nondihydropyridine). Management: Use lower starting doses of the nondihydropyridine calcium channel blockers (i.e., verapamil, diltiazem), and only consider increasing calcium channel blocker dose after obtaining ECG-based evidence that the combination is being well-tolerated. Consider therapy modification
Drospirenone: Angiotensin-Converting Enzyme Inhibitors may enhance the hyperkalemic effect of Drospirenone. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Edoxaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Edoxaban. Management: See full monograph for details. Reduced doses are recommended for patients receiving edoxaban for venous thromboembolism in combination with certain P-gp inhibitors. Similar dose adjustment is not recommended for edoxaban use in atrial fibrillation. Consider therapy modification
Efavirenz: May decrease the serum concentration of Calcium Channel Blockers. Monitor therapy
Eletriptan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eletriptan. Management: The use of eletriptan within 72 hours of a moderate CYP3A4 inhibitor should be avoided. Consider therapy modification
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Management: When combined with moderate CYP3A4 inhibitors, two elexacaftor/tezacaftor/ivacaftor (100 mg/50 mg/75 mg) tablets should be given in the morning, every other day. Ivacaftor (150 mg) should be given in the morning, every other day on alternate days. Consider therapy modification
Eliglustat: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eliglustat. Management: Use should be avoided under some circumstances. See full drug interaction monograph for details. Consider therapy modification
Encorafenib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Encorafenib. Management: Avoid concomitant use of encorafenib and moderate CYP3A4 inhibitors whenever possible. If concomitant administration is unavoidable, decrease the encorafenib dose prior to initiation of the CYP3A4 inhibitor. See full monograph for details. Consider therapy modification
Entrectinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Entrectinib. Management: Avoid moderate CYP3A4 inhibitors during treatment with entrectinib. Reduce dose to 200 mg/day if combination cannot be avoided in adults and those 12 yrs of age or older with a BSA of at least 1.5 square meters. No alternative dosing provided for others. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Eplerenone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eplerenone. Management: When used concomitantly with moderate inhibitors of CYP3A4, eplerenone dosing recommendations vary by indication and international labeling. See full drug interaction monograph for details. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Esmolol: Calcium Channel Blockers (Nondihydropyridine) may enhance the bradycardic effect of Esmolol. Management: Administration of IV verapamil or diltiazem together with esmolol is contraindicated if one agent is given while the effects of the other are still present. Canadian esmolol labeling specifies that use within 24 hours is contraindicated. Consider therapy modification
Estrogen Derivatives: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Estrogen Derivatives. Monitor therapy
Everolimus: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Everolimus. Management: Everolimus dose reductions are required for most indications. See full monograph or prescribing information for specific dose adjustment and monitoring recommendations. Consider therapy modification
Everolimus: Inhibitors of CYP3A4 (Moderate) and P-glycoprotein may increase the serum concentration of Everolimus. Management: Everolimus dose reductions are required for most indications. See full monograph or prescribing information for specific dose adjustment and monitoring recommendations. Consider therapy modification
FentaNYL: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of FentaNYL. Management: Monitor patients closely for several days following initiation of this combination, and adjust fentanyl dose as necessary. Consider therapy modification
Ferric Gluconate: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Ferric Gluconate. Monitor therapy
Ferric Hydroxide Polymaltose Complex: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Ferric Hydroxide Polymaltose Complex. Specifically, the risk for angioedema or allergic reactions may be increased. Monitor therapy
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fexofenadine: Verapamil may increase the serum concentration of Fexofenadine. Monitor therapy
Fingolimod: Verapamil may enhance the bradycardic effect of Fingolimod. Monitor therapy
Flecainide: Verapamil may enhance the adverse/toxic effect of Flecainide. In particular, this combination may significantly impair myocardial contractility and AV nodal conduction. Monitor therapy
Flibanserin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Flibanserin. Avoid combination
Fluconazole: May increase the serum concentration of Calcium Channel Blockers. Monitor therapy
Fosaprepitant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Fosaprepitant. Avoid combination
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: Calcium Channel Blockers may increase the serum concentration of Fosphenytoin. Management: Monitor for phenytoin toxicity with concomitant use of a calcium channel blocker (CCB) or decreased phenytoin effects with CCB discontinuation. Monitor for decreased CCB therapeutic effects. Nimodipine Canadian labeling contraindicates use with phenytoin. Consider therapy modification
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gelatin (Succinylated): Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Gelatin (Succinylated). Specifically, the risk of a paradoxical hypotensive reaction may be increased. Monitor therapy
Gold Sodium Thiomalate: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Gold Sodium Thiomalate. An increased risk of nitritoid reactions has been appreciated. Monitor therapy
Grapefruit Juice: May increase the serum concentration of Verapamil. Monitor therapy
Grass Pollen Allergen Extract (5 Grass Extract): Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Grass Pollen Allergen Extract (5 Grass Extract). Specifically, ACE inhibitors may increase the risk of severe allergic reaction to Grass Pollen Allergen Extract (5 Grass Extract). Consider therapy modification
GuanFACINE: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of GuanFACINE. Management: Reduce the guanfacine dose by 50% when initiating this combination. Consider therapy modification
Halofantrine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Halofantrine. Management: Extreme caution, with possibly increased monitoring of ECGs, should be used if halofantrine is combined with moderate CYP3A4 inhibitors. Drugs listed as exceptions to this monograph are discussed in separate drug interaction monographs. Monitor therapy
Heparin: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Heparins (Low Molecular Weight): May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
HYDROcodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of HYDROcodone. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Ibrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ibrutinib. Management: When treating B-cell malignancies, decrease ibrutinib to 280 mg daily when combined with moderate CYP3A4 inhibitors. When treating graft versus host disease, monitor patients closely and reduce the ibrutinib dose as needed based on adverse reactions. Consider therapy modification
Icatibant: May diminish the antihypertensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ifosfamide: CYP3A4 Inhibitors (Moderate) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Imatinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Imatinib. Monitor therapy
Iron Dextran Complex: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Iron Dextran Complex. Specifically, patients receiving an ACE inhibitor may be at an increased risk for anaphylactic-type reactions. Management: Follow iron dextran recommendations closely regarding both having resuscitation equipment and trained personnel on-hand prior to iron dextran administration and the use of a test dose prior to the first therapeutic dose. Consider therapy modification
Ivabradine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ivabradine. Avoid combination
Ivabradine: Calcium Channel Blockers (Nondihydropyridine) may enhance the bradycardic effect of Ivabradine. Ivabradine may enhance the QTc-prolonging effect of Calcium Channel Blockers (Nondihydropyridine). Specifically, the QTc prolonging effects of bepridil may be enhanced. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Ivabradine. Specifically, verapamil or diltiazem may increase serum ivabradine concentrations. Avoid combination
Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ivacaftor. Management: Ivacaftor dose reductions may be required; consult full monograph content for age- and weight-specific dosage recommendations. Consider therapy modification
Ivosidenib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ivosidenib. Management: Avoid use of moderate CYP3A4 inhibitors with ivosidenib whenever possible. If combined, monitor for increased ivosidenib toxicities. Drugs listed as exceptions are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Lanthanum: May decrease the serum concentration of Angiotensin-Converting Enzyme Inhibitors. Management: Administer angiotensin-converting enzyme inhibitors at least two hours before or after lanthanum. Consider therapy modification
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Larotrectinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Larotrectinib. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lefamulin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin tablets with P-glycoprotein/ABCB1 inhibitors. If concomitant use is required, monitor for lefamulin adverse effects. Consider therapy modification
Lemborexant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lemborexant. Avoid combination
Levamlodipine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Levamlodipine. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lithium: Angiotensin-Converting Enzyme Inhibitors may increase the serum concentration of Lithium. Management: Lithium dosage reductions will likely be needed following the addition of an ACE inhibitor. Monitor patient response to lithium closely following addition or discontinuation of concurrent ACE inhibitor treatment. Consider therapy modification
Lomitapide: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lomitapide. Avoid combination
Loop Diuretics: May enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Loop Diuretics may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Lovastatin: Verapamil may increase the serum concentration of Lovastatin. Management: Initiate lovastatin at a maximum adult dose of 10 mg/day, and do not exceed 20 mg/day, in patients receiving verapamil. Monitor closely for signs of HMG-CoA reductase inhibitor toxicity (e.g., myositis, rhabdomyolysis). Consider therapy modification
Lumateperone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lumateperone. Avoid combination
Lurasidone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lurasidone. Management: Lurasidone US labeling recommends reducing lurasidone dose by half with a moderate CYP3A4 inhibitor. Some non-US labeling recommends initiating lurasidone at 20 mg/day and limiting dose to 40 mg/day; avoid concurrent use of grapefruit products. Consider therapy modification
Macrolide Antibiotics: May decrease the metabolism of Calcium Channel Blockers. Management: Consider using a noninteracting macrolide. Felodipine Canadian labeling specifically recommends avoiding its use in combination with clarithromycin. Exceptions: Azithromycin (Systemic); Fidaxomicin; Roxithromycin; Spiramycin. Consider therapy modification
Magnesium Salts: Calcium Channel Blockers may enhance the adverse/toxic effect of Magnesium Salts. Magnesium Salts may enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Manidipine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Manidipine. Monitor therapy
Meperidine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Meperidine. Monitor therapy
MetFORMIN: Verapamil may diminish the therapeutic effect of MetFORMIN. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mirodenafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Mirodenafil. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naldemedine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Naldemedine. Monitor therapy
Naldemedine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naldemedine. Monitor therapy
Nalfurafine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Nalfurafine. Monitor therapy
Naloxegol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Naloxegol. Avoid combination
Neratinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Neratinib. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Neuromuscular-Blocking Agents (Nondepolarizing): Calcium Channel Blockers may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
NiMODipine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of NiMODipine. Monitor therapy
Nintedanib: Combined Inhibitors of CYP3A4 and P-glycoprotein may increase the serum concentration of Nintedanib. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Olaparib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Olaparib. Management: Avoid use of moderate CYP3A4 inhibitors in patients being treated with olaparib, if possible. If such concurrent use cannot be avoided, the dose of olaparib should be reduced to 150 mg twice daily. Consider therapy modification
Opioids (Anilidopiperidine): May enhance the bradycardic effect of Calcium Channel Blockers (Nondihydropyridine). Opioids (Anilidopiperidine) may enhance the hypotensive effect of Calcium Channel Blockers (Nondihydropyridine). Monitor therapy
OxyCODONE: CYP3A4 Inhibitors (Moderate) may enhance the adverse/toxic effect of OxyCODONE. CYP3A4 Inhibitors (Moderate) may increase the serum concentration of OxyCODONE. Serum concentrations of the active metabolite Oxymorphone may also be increased. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
PAZOPanib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pexidartinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Pexidartinib. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Exceptions: Loperamide. Monitor therapy
Phenytoin: Calcium Channel Blockers may increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Calcium Channel Blockers. Management: Avoid use of nimodipine or nifedipine with phenytoin. Monitor for phenytoin toxicity and/or decreased calcium channel blocker effects with any concurrent use. Consider therapy modification
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pimecrolimus: CYP3A4 Inhibitors (Moderate) may decrease the metabolism of Pimecrolimus. Monitor therapy
Pimozide: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Pimozide. Avoid combination
Potassium Salts: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Potassium-Sparing Diuretics: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Pregabalin: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Pregabalin. Specifically, the risk of angioedema may be increased. Monitor therapy
Propafenone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Propafenone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Protease Inhibitors: May decrease the metabolism of Calcium Channel Blockers (Nondihydropyridine). Increased serum concentrations of the calcium channel blocker may increase risk of AV nodal blockade. Management: Avoid concurrent use when possible. If used, monitor for CCB toxicity. The manufacturer of atazanavir recommends a 50% dose reduction for diltiazem be considered. Saquinavir, tipranavir, and darunavir/cobicistat use with bepridil is contraindicated. Consider therapy modification
Prucalopride: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Prucalopride. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNIDine: May enhance the hypotensive effect of Verapamil. Verapamil may increase the serum concentration of QuiNIDine. Monitor therapy
Racecadotril: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Specifically, the risk for angioedema may be increased with this combination. Monitor therapy
Ranolazine: Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Ranolazine. Management: Limit ranolazine dose to a maximum of 500 mg twice daily when used with diltiazem or verapamil. Consider therapy modification
Ranolazine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ranolazine. Management: Limit the ranolazine adult dose to a maximum of 500 mg twice daily in patients concurrently receiving moderate CYP3A4 inhibitors (e.g., diltiazem, verapamil, erythromycin, etc.). Consider therapy modification
Red Yeast Rice: Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Red Yeast Rice. Specifically, concentrations of lovastatin (and possibly other related compounds) may be increased. Monitor therapy
Regorafenib: May enhance the bradycardic effect of Calcium Channel Blockers (Nondihydropyridine). Monitor therapy
Rifamycin Derivatives: May decrease the serum concentration of Calcium Channel Blockers. This primarily affects oral forms of calcium channel blockers. Management: The labeling for some US and Canadian calcium channel blockers contraindicate use with rifampin, however recommendations vary. Consult appropriate labeling. Consider therapy modification
RifAXIMin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RifAXIMin. Monitor therapy
RisperiDONE: Verapamil may increase the serum concentration of RisperiDONE. Monitor therapy
Rivaroxaban: Inhibitors of CYP3A4 (Moderate) and P-glycoprotein may increase the serum concentration of Rivaroxaban. Management: No action is needed in patients with normal renal function. US labeling recommends avoidance in patients with estimated creatinine clearance 15 to 80 mL/min unless prospective benefits outweigh the risks. Other non-US labels may differ. Consider therapy modification
Rupatadine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Rupatadine. Monitor therapy
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Ruxolitinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ruxolitinib. Monitor therapy
Sacubitril: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Sacubitril. Specifically, the risk of angioedema may be increased with this combination. Avoid combination
Salicylates: May enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Salicylates may diminish the therapeutic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Salmeterol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Salmeterol. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
SAXagliptin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of SAXagliptin. Monitor therapy
Sildenafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Sildenafil. Monitor therapy
Silodosin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Silodosin. Monitor therapy
Silodosin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Silodosin. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Simeprevir. Avoid combination
Simvastatin: Verapamil may increase the serum concentration of Simvastatin. Management: Avoid concurrent use of verapamil with simvastatin when possible. If used together, limit adult maximum simvastatin dose to 10 mg/day, and avoid Simcor (simvastatin/niacin) because fixed simvastatin doses in the product exceed this maximum. Consider therapy modification
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
Sirolimus: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Sirolimus. Management: Monitor for increased serum concentrations of sirolimus if combined with a moderate CYP3A4 inhibitor. Lower initial sirolimus doses or sirolimus dose reductions will likely be required. Consider therapy modification
Sodium Phosphates: Angiotensin-Converting Enzyme Inhibitors may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with ACEIs, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, maintain adequate hydration and monitor renal function closely. Consider therapy modification
Sonidegib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Sonidegib. Management: Avoid concomitant use of sonidegib and moderate CYP3A4 inhibitors when possible. When concomitant use cannot be avoided, limit CYP3A4 inhibitor use to less than 14 days and monitor for sonidegib toxicity (particularly musculoskeletal adverse reactions). Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Suvorexant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Suvorexant. Management: The recommended dose of suvorexant is 5 mg daily in patients receiving a moderate CYP3A4 inhibitor. The dose can be increased to 10 mg daily (maximum dose) if necessary for efficacy. Consider therapy modification
Tacrolimus (Systemic): Calcium Channel Blockers (Nondihydropyridine) may decrease the metabolism of Tacrolimus (Systemic). Monitor therapy
Tacrolimus (Systemic): Angiotensin-Converting Enzyme Inhibitors may enhance the hyperkalemic effect of Tacrolimus (Systemic). Monitor therapy
Tacrolimus (Topical): Calcium Channel Blockers (Nondihydropyridine) may decrease the metabolism of Tacrolimus (Topical). Monitor therapy
Talazoparib: Verapamil may increase the serum concentration of Talazoparib. Management: If concurrent use cannot be avoided, reduce talazoparib dose to 0.75 mg once daily. After a period of 3 to 5 times the half-life of verapamil, increase the talazoparib dose to the dose used before initiation of verapamil. Consider therapy modification
Tamsulosin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tamsulosin. Monitor therapy
Tazemetostat: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tazemetostat. Management: Avoid coadministration of tazemetostat and moderate CYP3A4 inhibitors. If coadministration cannot be avoided, dose reductions are required. See full monograph for dosing recommendations. Consider therapy modification
Tegaserod: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Tegaserod. Monitor therapy
Telithromycin: May enhance the bradycardic effect of Verapamil. Telithromycin may enhance the hypotensive effect of Verapamil. Consider therapy modification
Temsirolimus: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Tetrahydrocannabinol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tezacaftor and Ivacaftor. Management: When combined with moderate CYP3A4 inhibitors, tezacaftor/ivacaftor should be given in the morning, every other day. Ivacaftor alone should be given in the morning, every other day on alternate days. Consider therapy modification
Theophylline Derivatives: Verapamil may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Thiazide and Thiazide-Like Diuretics: May enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Thiazide and Thiazide-Like Diuretics may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Ticagrelor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ticagrelor. Monitor therapy
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Tofacitinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tofacitinib. Monitor therapy
Tolvaptan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tolvaptan. Management: Jynarque dose requires adjustment when used with a moderate CYP3A4 inhibitor. See labeling or full interaction monograph for specific recommendations. Use of Samsca with moderate CYP3A4 ihibitors should generally be avoided. Consider therapy modification
Topotecan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Trabectedin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Trabectedin. Monitor therapy
Triazolam: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Triazolam. Management: Consider triazolam dose reduction in patients receiving concomitant moderate CYP3A4 inhibitors. Consider therapy modification
Trimethoprim: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Ubrogepant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and avoid a second dose for 24 hours when used with moderate CYP3A4 inhibitors. Consider therapy modification
Udenafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Udenafil. Monitor therapy
Ulipristal: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ulipristal. Management: This is specific for when ulipristal is being used for signs/symptoms of uterine fibroids (Canadian indication). When ulipristal is used as an emergency contraceptive, patients receiving this combination should be monitored for ulipristal toxicity. Avoid combination
Urapidil: May interact via an unknown mechanism with Angiotensin-Converting Enzyme Inhibitors. Management: Avoid concomitant use of urapidil and angiotensin-converting enzyme (ACE) inhibitors. Consider therapy modification
Venetoclax: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Venetoclax. Management: Reduce the venetoclax dose by at least 50% in patients requiring these combinations. Consider therapy modification
Venetoclax: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Venetoclax. Management: Consider a venetoclax dose reduction by at least 50% in patients requiring concomitant treatment with P-glycoprotein (P-gp) inhibitors. Consider therapy modification
Vilazodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Vilazodone. Monitor therapy
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vindesine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Vindesine. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Zanubrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zanubrutinib. Management: Decrease the zanubrutinib dose to 80 mg twice daily during coadministration with a moderate CYP3A4 inhibitor. Further dose adjustments may be required for zanubrutinib toxicities, refer to prescribing information for details. Consider therapy modification
Zopiclone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zopiclone. Management: The starting adult dose of zopiclone should not exceed 3.75 mg if combined with a moderate CYP3A4 inhibitor. Monitor patients for signs and symptoms of zopiclone toxicity if these agents are combined. Consider therapy modification
Zuclopenthixol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zuclopenthixol. Monitor therapy
Adverse Reactions
See individual agents.
Warnings/Precautions
Concerns related to adverse effects:
- Angioedema: At any time during treatment (especially following first dose) angioedema may occur rarely with ACE inhibitors; it may involve the head and neck (potentially compromising the airway) or the intestine (presenting with abdominal pain). African-Americans and patients with idiopathic or hereditary angioedema may be at an increased risk. Risk may also be increased with concomitant use of mTOR inhibitor (eg, everolimus) therapy or a neprilysin inhibitor (eg, sacubitril). Prolonged frequent monitoring may be required especially if tongue, glottis, or larynx are involved as they are associated with airway obstruction. Patients with a history of airway surgery may have a higher risk of airway obstruction. Aggressive early and appropriate management is critical. Use in patients with previous angioedema associated with ACE inhibitor therapy is contraindicated.
- Conduction abnormalities: Verapamil can cause first-degree AV block and transient bradycardia, sometimes accompanied by nodal escape rhythms; other conduction abnormalities are rare. Marked first-degree AV block or progressive development to second- or third-degree AV block requires a dose discontinuation. Use is contraindicated in patients with sick sinus syndrome, second- or third-degree AV block (except in patients with a functioning pacemaker), or an accessory bypass tract (eg, Wolff-Parkinson-White syndrome).
- Cough: An ACE inhibitor cough is a dry, hacking, nonproductive one that usually occurs within the first few months of treatment and should generally resolve within 1 to 4 weeks after discontinuation of the ACE inhibitor. Other causes of cough should be considered (eg, pulmonary congestion in patients with heart failure) and excluded prior to discontinuation.
- Hematologic effects: Another ACE Inhibitor, captopril, has been associated with neutropenia with myeloid hypoplasia and agranulocytosis; anemia and thrombocytopenia have also occurred. Patients with renal impairment are at high risk of developing neutropenia. Patients with both renal impairment and collagen vascular disease (eg, systemic lupus erythematosus) are at an even higher risk of developing neutropenia. Periodically monitor CBC with differential in these patients.
- Hepatic effects: Elevations of transaminases have been reported with verapamil. Several cases of hepatocellular injury related to verapamil have been proven by rechallenge. A rare toxicity associated with ACE inhibitors includes cholestatic jaundice, which may progress to fulminant hepatic necrosis (same fatal). Discontinue therapy if marked elevation of hepatic transaminases or jaundice occurs.
- Hyperkalemia: May occur with ACE inhibitors; risk factors include renal dysfunction, diabetes mellitus, concomitant use of potassium-sparing diuretics, potassium supplements, and/or potassium-containing salts. Use cautiously, if at all, with these agents and monitor potassium closely.
- Hypersensitivity reactions: Anaphylactic/anaphylactoid reactions can occur with ACE inhibitors. Severe anaphylactoid reactions may be seen during hemodialysis (eg, CVVHD) with high-flux dialysis membranes (eg, AN69), and rarely, during low density lipoprotein apheresis with dextran sulfate cellulose. Rare cases of anaphylactoid reactions have been reported in patients undergoing sensitization treatment with hymenoptera (bee, wasp) venom while receiving ACE inhibitors.
- Hypotension/syncope: Symptomatic hypotension with or without syncope can occur (usually with the first several doses); effects are most often observed in volume-depleted patients; correct volume depletion prior to initiation; close monitoring of patient is required especially with initial dosing and dosing increases; blood pressure must be lowered at a rate appropriate for the patient's clinical condition. Although dose reduction may be necessary, hypotension is not a reason for discontinuation of future ACE inhibitor use especially in patients with heart failure where a reduction in systolic blood pressure is a desirable observation.
- Renal function deterioration: ACE inhibitors may be associated with deterioration of renal function and/or increases in BUN and serum creatinine, particularly in patients with low renal blood flow (eg, renal artery stenosis, heart failure) whose glomerular filtration rate (GFR) is dependent on efferent arteriolar vasoconstriction by angiotensin II; deterioration may result in oliguria, acute renal failure, and progressive azotemia. Small, benign increases in serum creatinine may occur following initiation; consider discontinuation only in patients with progressive and/or significant deterioration in renal function (Bakris 2000).
Disease-related concerns:
- Aortic stenosis: Use trandolapril with caution in patients with aortic stenosis; may reduce coronary perfusion resulting in ischemia.
- Arrhythmia: Verapamil is considered contraindicated in patients with wide complex tachycardias unless known to be supraventricular in origin; severe hypotension likely to occur upon administration (ACLS [Neumar] 2010).
- Attenuated neuromuscular transmission: Decreased neuromuscular transmission has been reported with verapamil; use with caution in patients with attenuated neuromuscular transmission (Duchenne muscular dystrophy, myasthenia gravis); dosage reduction may be required.
- Cardiovascular disease: Initiation of therapy in patients with ischemic heart disease or cerebrovascular disease warrants close observation due to the potential consequences posed by falling blood pressure (eg, MI, stroke). Fluid replacement, if needed, may restore blood pressure; therapy may then be resumed. Discontinue therapy in patients whose hypotension recurs.
- Collagen vascular disease: Use trandolapril with caution in patients with collagen vascular disease especially with concomitant renal impairment; may be at increased risk for hematologic toxicity.
- Heart failure: Avoid verapamil in heart failure; can exacerbate condition. Contraindicated with severe left ventricular dysfunction (eg, ejection fraction <30%, pulmonary wedge pressure >20 mm Hg, severe symptoms of cardiac failure) or cardiogenic shock. In patients with any degree of ventricular dysfunction receiving a beta blocker, avoid use.
- Hepatic impairment: Use with caution in patients with hepatic impairment; lower doses are recommended.
- Hypertrophic cardiomyopathy (HCM) with outflow tract obstruction: Use with caution in patients with HCM with outflow tract obstruction (especially those with high gradients, advanced heart failure, or sinus bradycardia); reduction in afterload may worsen symptoms associated with this condition (ACCF/AHA [Gersh 2011]). Verapamil should not be used in patients with systemic hypotension or severe dyspnea at rest (Nishimura 2004).
- Renal artery stenosis: Use trandolapril with caution in patients with unstented unilateral/bilateral renal artery stenosis. When unstented bilateral renal artery stenosis is present, use is generally avoided due to the elevated risk of deterioration in renal function unless possible benefits outweigh risks.
- Renal impairment: Use with caution in patients with renal impairment; dosage adjustment is recommended.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Black patients: ACE inhibitor effectiveness is less in black patients than in nonblacks. In addition, ACE inhibitors cause a higher rate of angioedema in black than in non-black patients.
- Pregnancy: [US Boxed Warning]: Drugs that act on the renin-angiotensin system can cause injury and death to the developing fetus. Discontinue as soon as possible once pregnancy is detected.
Other warnings/precautions:
- Surgery: In patients on chronic ACE inhibitor therapy, intraoperative hypotension may occur with induction and maintenance of general anesthesia; use with caution before, during, or immediately after major surgery. Cardiopulmonary bypass, intraoperative blood loss, or vasodilating anesthesia increases endogenous renin release. Use of ACE inhibitors perioperatively will blunt angiotensin II formation and may result in hypotension. However, discontinuation of therapy prior to surgery is controversial. If continued preoperatively, avoidance of hypotensive agents during surgery is prudent (Hillis 2011).
Monitoring Parameters
Blood pressure and heart rate; BUN, serum creatinine and electrolytes; if patient has collagen vascular disease and/or renal impairment, periodically monitor CBC with differential.
Pregnancy
Pregnancy Considerations
[US Boxed Warning]: Drugs that act on the renin-angiotensin system can cause injury and death to the developing fetus. Discontinue as soon as possible once pregnancy is detected. See individual agents.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience cough. Have patient report immediately to prescriber signs of infection, signs of kidney problems (unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain), signs of high potassium (abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, or numbness or tingling feeling), signs of heart problems (cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out), signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), severe dizziness, passing out, persistent cough, chest pain, fast heartbeat, slow heartbeat, abnormal heartbeat, or muscle weakness (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.