Boxed Warning
Fetal toxicity:
When pregnancy is detected, discontinue trandolapril as soon as possible. Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral:
Mavik: 1 mg [DSC], 2 mg [DSC]
Generic: 1 mg, 2 mg, 4 mg
Pharmacology
Mechanism of Action
Trandolapril is an ACE inhibitor which prevents the formation of angiotensin II from angiotensin I. Trandolapril must undergo enzymatic hydrolysis, mainly in liver, to its biologically active metabolite, trandolaprilat. A CNS mechanism may also be involved in the hypotensive effect as angiotensin II increases adrenergic outflow from the CNS. Vasoactive kallikreins may be decreased in conversion to active hormones by ACE inhibitors, thus reducing blood pressure.
Pharmacokinetics/Pharmacodynamics
Absorption
Slowed with food
Distribution
Trandolapril: ~18 L
Metabolism
Hepatically hydrolyzed to active metabolite, trandolaprilat and at least 7 other metabolites
Excretion
Urine (~33% as trandolapril and trandolaprilat); feces (~66%)
Renal clearance: 1 to 4 L/hour (dose dependent); reduced in renal impairment
Time to Peak
Trandolapril: ~1 hour; Trandolaprilat: 4 to 10 hours
Half-Life Elimination
Trandolapril: ~6 hours; Trandolaprilat: Effective: 22.5 hours
Protein Binding
Trandolapril: ~80%; Trandolaprilat: 65% to 94% (concentration dependent)
Use in Specific Populations
Special Populations: Renal Function Impairment
Plasma trandolapril and trandolaprilat are approximately 2-fold greater and renal Cl is decreased ~85% in patients with CrCl <30 mL/minute and in hemodialysis patients.
Special Populations: Hepatic Function Impairment
In patients with mild to moderate alcoholic cirrhosis, plasma concentrations of trandolapril and trandolaprilat were 9- and 2-fold greater, respectively, but inhibition of ACE activity was not affected.
Special Populations: Elderly
Plasma concentration of trandolapril is increased.
Use: Labeled Indications
Hypertension: Management of hypertension
Guideline recommendations: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults recommends if monotherapy is warranted, in the absence of comorbidities (eg, cerebrovascular disease, chronic kidney disease, diabetes, heart failure [HF], ischemic heart disease, etc.), that thiazide-like diuretics or dihydropyridine calcium channel blockers may be preferred options due to improved cardiovascular endpoints (eg, prevention of HF and stroke). ACE inhibitors and ARBs are also acceptable for monotherapy. Combination therapy may be required to achieve blood pressure goals and is initially preferred in patients at high risk (stage 2 hypertension or atherosclerotic cardiovascular disease [ASCVD] risk ≥10%) (ACC/AHA [Whelton 2017]).
Post-myocardial infarction (MI) heart failure or left-ventricular dysfunction: Treatment of post-MI HF in patients who are symptomatic from HF within the first few days after sustaining acute MI or post-MI left ventricular dysfunction in stable patients who have evidence of left ventricular systolic dysfunction (identified by wall motion abnormalities)
Use: Off Label
Heart failureyes
The American College of Cardiology/American Heart Association (ACC/AHA) 2013 Heart Failure Guidelines recommend the use of ACE inhibitors, along with other guideline-directed medical therapies, to prevent progression of heart failure (HF) and reduced ejection fraction in asymptomatic patients with or without a history of myocardial infarction (Stage B HF), or to treat those with symptomatic HF and reduced ejection fraction to reduce morbidity and mortality (Stage C HFrEF).
Non–ST-elevation acute coronary syndromeyes
Based on the ACC/AHA guidelines for the management of patients with non-ST-elevation acute coronary syndromes (NSTE-ACS), an ACE inhibitor should be initiated and continued indefinitely after NSTE-ACS in patients with a left ventricular ejection fraction (LVEF) ≤40% and in those with hypertension, diabetes mellitus, or stable CKD unless contraindicated. Use of an ACE inhibitor may also be useful in all other patients with cardiac or other vascular disease.
Stable coronary artery diseaseyes
Based on the ACC/AHA guideline for the diagnosis and management of patients with stable ischemic heart disease, an ACE inhibitor or ARB should be prescribed in all patients with stable ischemic heart disease who also have hypertension, diabetes mellitus, LVEF <40%, or CKD unless contraindicated.
ST-elevation acute coronary syndromeyes
Based on the 2013 ACC/AHA guidelines for the management of patients with ST-elevation acute coronary syndromes (STE-ACS), an ACE inhibitor should be initiated within the first 24 hours to all patients with STE-ACS with anterior location, HF, or LVEF ≤40%, unless contraindicated. It is also reasonable to initiate an ACE inhibitor in all patients with STE-ACS.
Contraindications
Hypersensitivity to trandolapril or any component of the formulation; coadministration with aliskiren in patients with diabetes; hereditary/idiopathic angioedema; history of angioedema related to previous treatment with an ACE inhibitor; coadministration with or within 36 hours of switching to or from a neprilysin inhibitor (eg, sacubitril).
Documentation of allergenic cross-reactivity for Angiotensin-Converting Enzyme Inhibitors is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to other ACE inhibitors; women who are pregnant, planning to become pregnant, or women of childbearing potential and not using adequate contraception; breastfeeding; hypotensive or hemodynamically unstable states; hemodynamically significant bilateral artery stenosis or severe artery stenosis of a solitary functioning kidney; concomitant use with sacubitril/valsartan; concomitant use with ACE inhibitors, angiotensin receptor blockers (ARBs) or aliskiren-containing medications in patients with type 1 or 2 diabetes mellitus, moderate to severe renal impairment (GFR <60 mL/minute/1.73 m2), hyperkalemia (>5 mMol/L) or with heart failure who are hypotensive; hereditary problems of galactose intolerance, Lapp lactase deficiency or glucose-galactose malabsorption.
Dosage and Administration
Dosing: Adult
Hypertension: Oral: Initial: 1 mg once daily; titrate dose as needed up to 4 mg once daily at intervals of ≥1 week based on patient response (ACC/AHA [Whelton 2017]). There is little experience with doses >8 mg daily.
Post-MI heart failure or LV dysfunction: Oral: Initial: 1 mg once daily; titrate (as tolerated) toward target dose of 4 mg once daily. If 4 mg dose is not tolerated, patients may continue therapy with the greatest tolerated dose. The American College of Cardiology/American Heart Association guidelines recommend the use of a 0.5 mg test dose with titration up to 4 mg daily as tolerated (ACC/AHA [O’Gara 2013]).
Heart failure with reduced ejection fraction (HFrEF) (off-label use): Oral: Initial: 1 mg once daily; target dose: 4 mg once daily (ACCF/AHA [Yancy 2013]).
Dosing: Geriatric
Refer to adult dosing.
Dietary Considerations
Use potassium-containing salt substitutes cautiously in patients with diabetes, renal impairment, or those maintained on potassium supplements or potassium-sparing diuretics.
Storage
Store at 20°C to 25°C (68°F to 77°F).
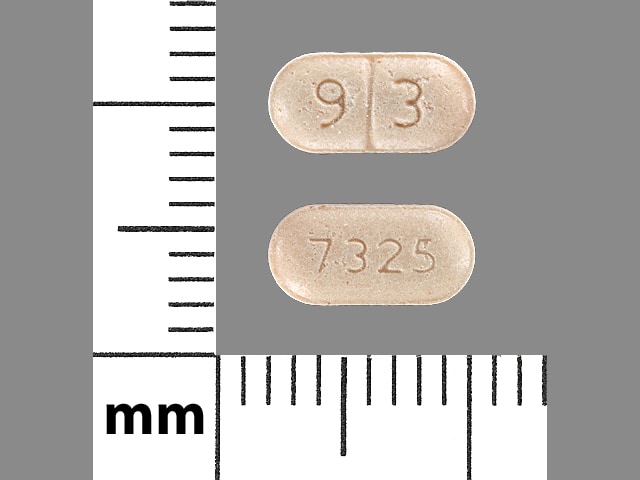
Trandolapril Images
Drug Interactions
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Aliskiren: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Aliskiren may enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Aliskiren may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Management: Aliskiren use with ACEIs or ARBs in patients with diabetes is contraindicated. Combined use in other patients should be avoided, particularly when CrCl is less than 60 mL/min. If combined, monitor potassium, creatinine, and blood pressure closely. Consider therapy modification
Allopurinol: Angiotensin-Converting Enzyme Inhibitors may enhance the potential for allergic or hypersensitivity reactions to Allopurinol. Consider therapy modification
Alteplase: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Alteplase. Specifically, the risk for angioedema may be increased. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Angiotensin II: Angiotensin-Converting Enzyme Inhibitors may enhance the therapeutic effect of Angiotensin II. Monitor therapy
Angiotensin II Receptor Blockers: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Angiotensin II Receptor Blockers may increase the serum concentration of Angiotensin-Converting Enzyme Inhibitors. Management: In US labeling, use of telmisartan and ramipril is not recommended. It is not clear if any other combination of an ACE inhibitor and an ARB would be any safer. Consider alternatives to the combination when possible. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Aprotinin: May diminish the antihypertensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
AzaTHIOprine: Angiotensin-Converting Enzyme Inhibitors may enhance the myelosuppressive effect of AzaTHIOprine. Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Dapoxetine: May enhance the orthostatic hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dipeptidyl Peptidase-IV Inhibitors: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Specifically, the risk of angioedema may be increased. Monitor therapy
Drospirenone: Angiotensin-Converting Enzyme Inhibitors may enhance the hyperkalemic effect of Drospirenone. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Eplerenone: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Everolimus: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Specifically, the risk of angioedema may be increased. Monitor therapy
Ferric Gluconate: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Ferric Gluconate. Monitor therapy
Ferric Hydroxide Polymaltose Complex: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Ferric Hydroxide Polymaltose Complex. Specifically, the risk for angioedema or allergic reactions may be increased. Monitor therapy
Gelatin (Succinylated): Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Gelatin (Succinylated). Specifically, the risk of a paradoxical hypotensive reaction may be increased. Monitor therapy
Gold Sodium Thiomalate: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Gold Sodium Thiomalate. An increased risk of nitritoid reactions has been appreciated. Monitor therapy
Grass Pollen Allergen Extract (5 Grass Extract): Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Grass Pollen Allergen Extract (5 Grass Extract). Specifically, ACE inhibitors may increase the risk of severe allergic reaction to Grass Pollen Allergen Extract (5 Grass Extract). Consider therapy modification
Heparin: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Heparins (Low Molecular Weight): May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Icatibant: May diminish the antihypertensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Iron Dextran Complex: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Iron Dextran Complex. Specifically, patients receiving an ACE inhibitor may be at an increased risk for anaphylactic-type reactions. Management: Follow iron dextran recommendations closely regarding both having resuscitation equipment and trained personnel on-hand prior to iron dextran administration and the use of a test dose prior to the first therapeutic dose. Consider therapy modification
Lanthanum: May decrease the serum concentration of Angiotensin-Converting Enzyme Inhibitors. Management: Administer angiotensin-converting enzyme inhibitors at least two hours before or after lanthanum. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lithium: Angiotensin-Converting Enzyme Inhibitors may increase the serum concentration of Lithium. Management: Lithium dosage reductions will likely be needed following the addition of an ACE inhibitor. Monitor patient response to lithium closely following addition or discontinuation of concurrent ACE inhibitor treatment. Consider therapy modification
Loop Diuretics: May enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Loop Diuretics may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Potassium Salts: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Potassium-Sparing Diuretics: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Pregabalin: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Pregabalin. Specifically, the risk of angioedema may be increased. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Racecadotril: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Specifically, the risk for angioedema may be increased with this combination. Monitor therapy
Ranolazine: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Sacubitril: Angiotensin-Converting Enzyme Inhibitors may enhance the adverse/toxic effect of Sacubitril. Specifically, the risk of angioedema may be increased with this combination. Avoid combination
Salicylates: May enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Salicylates may diminish the therapeutic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Sirolimus: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Sodium Phosphates: Angiotensin-Converting Enzyme Inhibitors may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with ACEIs, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, maintain adequate hydration and monitor renal function closely. Consider therapy modification
Tacrolimus (Systemic): Angiotensin-Converting Enzyme Inhibitors may enhance the hyperkalemic effect of Tacrolimus (Systemic). Monitor therapy
Temsirolimus: May enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Thiazide and Thiazide-Like Diuretics: May enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Thiazide and Thiazide-Like Diuretics may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
TiZANidine: May enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Tolvaptan: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Trimethoprim: May enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Urapidil: May interact via an unknown mechanism with Angiotensin-Converting Enzyme Inhibitors. Management: Avoid concomitant use of urapidil and angiotensin-converting enzyme (ACE) inhibitors. Consider therapy modification
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
May lead to false-negative aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
Frequency ranges include data from hypertension and heart failure trials. Higher rates of adverse reactions have generally been noted in patients with heart failure. However, the frequency of adverse effects associated with placebo is also increased in this population.
>10%:
Cardiovascular: Hypotension (≤11%)
Central nervous system: Dizziness (1% to 23%)
Endocrine & metabolic: Increased uric acid (15%)
Respiratory: Cough (2% to 35%)
1% to 10%:
Cardiovascular: Syncope (6%), bradycardia (≤5%), cardiogenic shock (4%), intermittent claudication (4%), cerebrovascular accident (3%)
Endocrine & metabolic: Hyperkalemia (5%), hypocalcemia (5%)
Gastrointestinal: Gastritis (4%), diarrhea (1%)
Neuromuscular & skeletal: Myalgia (5%), weakness (3%)
Renal: Increased blood urea nitrogen (9%), increased serum creatinine (1% to 5%)
<1%, postmarketing, and/or case reports: Abdominal distention, abdominal pain, agranulocytosis, alopecia, angina pectoris, angioedema, anxiety, bronchitis, bronchospasm, cardiac arrhythmia, cardiac failure, cerebral hemorrhage, chest pain, cholestasis, constipation, decreased libido, depression, dermatitis, diaphoresis, drowsiness, dyspepsia, dyspnea, edema, epistaxis, equilibrium disturbance, fever, first degree atrioventricular block, flushing, gout, hallucination, hepatitis, hypersensitivity angiitis, hyponatremia, impotence, increased serum ALT, increased serum AST, increased serum bilirubin, increased serum transaminases, insomnia, intestinal angioedema, intestinal obstruction, ischemic heart disease, jaundice, laryngeal edema, leukopenia, limb pain, malaise, myalgia, myocardial infarction, nausea, neutropenia, palpitations, pancreatitis, pancytopenia, paresthesia, pemphigus, pharyngitis, pruritus, renal failure, skin rash, Stevens-Johnson syndrome, symptomatic hypotension, tachycardia, thrombocytopenia, toxic epidermal necrolysis, transient ischemic attacks, upper respiratory tract infection, urticaria, ventricular tachycardia, vertigo, visual impairment, vomiting, xerostomia
Warnings/Precautions
Concerns related to adverse reactions:
- Angioedema: At any time during treatment (especially following first dose) angioedema may occur rarely with ACE inhibitors; it may involve the head and neck (potentially compromising the airway) or the intestine (presenting with abdominal pain). African-Americans and patients with idiopathic or hereditary angioedema may be at an increased risk. Risk may also be increased with concomitant use of mTOR inhibitor (eg, everolimus) therapy or a neprilysin inhibitor (eg, sacubitril). Prolonged frequent monitoring may be required especially if tongue, glottis, or larynx are involved as they are associated with airway obstruction. Patients with a history of airway surgery may have a higher risk of airway obstruction. Aggressive early and appropriate management is critical. Use in patients with previous angioedema associated with ACE inhibitor therapy is contraindicated.
- Cholestatic jaundice: A rare toxicity associated with ACE inhibitors includes cholestatic jaundice, which may progress to fulminant hepatic necrosis (some fatal); discontinue if marked elevation of hepatic transaminases or jaundice occurs.
- Cough: An ACE inhibitor cough is a dry, hacking, nonproductive one that usually occurs within the first few months of treatment and should generally resolve within 1 to 4 weeks after discontinuation of the ACE inhibitor. Other causes of cough should be considered (eg, pulmonary congestion in patients with heart failure) and excluded prior to discontinuation.
- Hematologic effects: Another ACE inhibitor, captopril, has been associated with neutropenia with myeloid hypoplasia and agranulocytosis; anemia and thrombocytopenia have also occurred. Patients with renal impairment are at high risk of developing neutropenia. Patients with both renal impairment and collagen vascular disease (eg, systemic lupus erythematosus) are at an even higher risk of developing neutropenia. Periodically monitor CBC with differential in these patients.
- Hyperkalemia: May occur with ACE inhibitors; risk factors include renal dysfunction, diabetes mellitus, concomitant use of potassium-sparing diuretics, potassium supplements, and/or potassium-containing salts. Use cautiously, if at all, with these agents and monitor potassium closely.
- Hypersensitivity reactions: Anaphylactic/anaphylactoid reactions can occur with ACE inhibitors. Severe anaphylactoid reactions may be seen during hemodialysis (eg, CVVHD) with high-flux dialysis membranes (eg, AN69), and rarely, during low density lipoprotein apheresis with dextran sulfate cellulose. Rare cases of anaphylactoid reactions have been reported in patients undergoing sensitization treatment with hymenoptera (bee, wasp) venom while receiving ACE inhibitors.
- Hypotension/syncope: Symptomatic hypotension with or without syncope can occur with ACE inhibitors (usually with the first several doses); effects are most often observed in volume-depleted patients; correct volume depletion prior to initiation; close monitoring of patient is required especially with initial dosing and dosing increases; blood pressure must be lowered at a rate appropriate for the patient's clinical condition. Although dose reduction may be necessary, hypotension is not a reason for discontinuation of future ACE inhibitor use especially in patients with heart failure where a reduction in systolic blood pressure is a desirable observation.
- Renal function deterioration: May be associated with deterioration of renal function and/or increases in BUN and serum creatinine, particularly in patients with low renal blood flow (eg, renal artery stenosis, heart failure) whose glomerular filtration rate (GFR) is dependent on efferent arteriolar vasoconstriction by angiotensin II; deterioration may result in oliguria, acute renal failure, and progressive azotemia. Small benign increases in serum creatinine may occur following initiation; consider discontinuation only in patients with progressive and/or significant deterioration in renal function (Bakris 2000).
Disease-related concerns:
- Aortic stenosis: Use with caution in patients with aortic stenosis; may reduce coronary perfusion resulting in ischemia.
- Ascites: Avoid use in patients with ascites due to cirrhosis or refractory ascites; if use cannot be avoided in patients with ascites due to cirrhosis, monitor blood pressure and renal function carefully to avoid rapid development of renal failure (AASLD [Runyon 2012]).
- Cardiovascular disease: Initiation of therapy in patients with ischemic heart disease or cerebrovascular disease warrants close observation due to the potential consequences posed by falling blood pressure (eg, MI, stroke). Fluid replacement, if needed, may restore blood pressure; therapy may then be resumed. Discontinue therapy in patients whose hypotension recurs.
- Collagen vascular disease: Use with caution in patients with collagen vascular disease especially with concomitant renal impairment; may be at increased risk for hematologic toxicity.
- Hepatic impairment: Use with caution in patients with hepatic impairment; dosage adjustment recommended in patients with cirrhosis and lower doses should be considered in patients with hepatic impairment.
- Hypertrophic cardiomyopathy (HCM) with outflow tract obstruction: Use with caution in patients with HCM and outflow tract obstruction since reduction in afterload may worsen symptoms associated with this condition (ACC/AHA [Gersh 2011]).
- Renal artery stenosis: Use with caution in patients with unstented unilateral/bilateral renal artery stenosis. When unstented bilateral renal artery stenosis is present, use is generally avoided due to the elevated risk of deterioration in renal function unless possible benefits outweigh risks.
- Renal impairment: Use with caution in patients with renal impairment; dosage adjustment recommended in patients with CrCl <30 mL/minute. Avoid rapid dosage escalation, which may lead to further renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Black patients: ACE inhibitors' effectiveness is less in black patients than in non-blacks. In addition, ACE inhibitors cause a higher rate of angioedema in black than in non-black patients.
- Pregnancy: [US Boxed Warning]: Drugs that act on the renin-angiotensin system can cause injury and death to the developing fetus. Discontinue as soon as possible once pregnancy is detected.
- Surgical patients: In patients on chronic ACE inhibitor therapy, intraoperative hypotension may occur with induction and maintenance of general anesthesia; use with caution before, during, or immediately after major surgery. Cardiopulmonary bypass, intraoperative blood loss, or vasodilating anesthesia increases endogenous renin release. Use of ACE inhibitors perioperatively will blunt angiotensin II formation and may result in hypotension. However, discontinuation of therapy prior to surgery is controversial. If continued preoperatively, avoidance of hypotensive agents during surgery is prudent (Hillis 2011). Based on current research and clinical guidelines in patients undergoing non-cardiac surgery, continuing ACE inhibitors is reasonable in the perioperative period. If ACE inhibitors are held before surgery, it is reasonable to restart postoperatively as soon as clinically feasible (ACC/AHA [Fleisher 2014]).
Monitoring Parameters
Blood pressure; BUN, serum creatinine and electrolytes; if patient has collagen vascular disease and/or renal impairment, periodically monitor CBC with differential
Heart Failure: Within 1 to 2 weeks after initiation and periodically thereafter, reassess renal function and serum potassium especially in patients with preexisting hypotension, hyponatremia, diabetes mellitus, azotemia, or those taking potassium supplements (ACC/AHA [Yancy 2013]).
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year atherosclerotic cardiovascular disease (ASCVD) risk ≥10%: Target blood pressure <130/80 mm Hg is recommended
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable
Diabetes and hypertension: The American Diabetes Association (ADA) guidelines (ADA 2019):
Patients 18 to 65 years of age, without ASCVD, and 10-year ASCVD risk <15%: Target blood pressure <140/90 mm Hg is recommended.
Patients 18 to 65 years of age and known ASCVD or 10-year ASCVD risk >15%: Target blood pressure <130/80 mm Hg may be appropriate if it can be safely attained.
Patients >65 years of age (healthy or complex/intermediate health): Target blood pressure <140/90 mm Hg is recommended.
Patients >65 years of age (very complex/poor health): Target blood pressure <150/90 mm Hg is recommended.
Pregnancy
Pregnancy Risk Factor
D
Pregnancy Considerations
Exposure to an angiotensin-converting enzyme (ACE) inhibitor during the first trimester of pregnancy may be associated with an increased risk of fetal malformations (ACOG 203 2019; ESC [Regitz-Zagrosek 2018]); however, outcomes observed may also be influenced by maternal disease (ACC/AHA [Whelton 2017]).
[US Boxed Warning]: Drugs that act on the renin-angiotensin system can cause injury and death to the developing fetus. Discontinue as soon as possible once pregnancy is detected. Drugs that act on the renin-angiotensin system are associated with oligohydramnios. Oligohydramnios, due to decreased fetal renal function, may lead to fetal lung hypoplasia and skeletal malformations. The use of these drugs in pregnancy is also associated with anuria, hypotension, renal failure, skull hypoplasia, and death in the fetus/neonate. Infants exposed to an ACE inhibitor in utero should be monitored for hyperkalemia, hypotension, and oliguria. Oligohydramnios may not appear until after irreversible fetal injury has occurred. Exchange transfusions or dialysis may be required to reverse hypotension or improve renal function, although data related to the effectiveness in neonates is limited.
Chronic maternal hypertension is also associated with adverse events in the fetus/infant. Chronic maternal hypertension may increase the risk of birth defects, low birth weight, premature delivery, stillbirth, and neonatal death. Actual fetal/neonatal risks may be related to duration and severity of maternal hypertension. Untreated chronic hypertension may also increase the risks of adverse maternal outcomes, including gestational diabetes, preeclampsia, delivery complications, stroke, and myocardial infarction (ACOG 203 2019).
When treatment of hypertension in pregnancy is indicated, ACE inhibitors should generally be avoided due to their adverse fetal events; use in pregnant women should only be considered for cases of hypertension refractory to other medications (ACOG 203 2019). ACE inhibitors are not recommended for the treatment of heart failure in pregnancy (Regitz-Zagrosek [ESC 2018]).
ACE inhibitors should be avoided in sexually active females of reproductive potential not using effective contraception (ADA 2020). ACE inhibitors should generally be avoided for the treatment of hypertension in women planning a pregnancy; use should only be considered for cases of hypertension refractory to other medications (ACOG 203 2019).
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It is used to treat heart failure (weak heart).
- It is used to help heart function after a heart attack.
- It may be given to you for other reasons. Talk with the doctor.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- High potassium like abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, or numbness or tingling feeling
- Severe dizziness
- Passing out
- Persistent cough
- Severe abdominal pain
- Severe nausea
- Vomiting
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.