Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Oral [strength expressed as base]:
Primsol: 50 mg/5 mL (473 mL [DSC]) [alcohol free, dye free; contains methylparaben, propylene glycol, propylparaben, saccharin sodium, sodium benzoate]
Primsol: 50 mg/5 mL (473 mL) [alcohol free, dye free; contains methylparaben, propylene glycol, propylparaben, saccharin sodium, sodium benzoate; bubble-gum flavor]
Trimpex: 50 mg/5 mL (473 mL [DSC]) [alcohol free, dye free; contains methylparaben, propylene glycol, propylparaben, saccharin sodium, sodium benzoate, sorbitol; bubble-gum flavor]
Tablet, Oral:
Generic: 100 mg
Pharmacology
Mechanism of Action
Inhibits folic acid reduction to tetrahydrofolate by reversible inhibition of dihydrofolate reductase, inhibiting bacterial synthesis of nucleic acids and proteins
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Readily and extensively absorbed
Distribution
Widely into body tissues and fluids (middle ear, prostate, bile, aqueous humor, CSF); mean peak middle ear fluid concentration in children 1 to 12 years of 2 mcg/mL after a single 4 mg/kg dose; Vd:
Newborns: 2.7 L/kg (range: 1.3 to 4.1 hours) (Springer 1982)
Infants: 1.5 L/kg (Hoppu 1989)
Children (Hoppu 1987):
1 to 3 years: 0.86 L/kg
8 to 10 years: 1 L/kg
Adults: ~1.3 L/kg (Hoppu 1987)
Metabolism
Partially hepatic (10% to 20%) via demethylation, oxidation, and hydroxylation
Excretion
Urine (50% to 60%; 80% as unchanged drug); feces
Time to Peak
Serum: 1 to 4 hours
Half-Life Elimination
Prolonged with renal impairment
Newborns: 19 hours; range: 11 to 27 hours (Springer 1982)
Infants 2 months to 1 year: 4.6 hours; range: 3 to 6 hours (Hoppu 1989)
Children (Hoppu 1987): 1 to 3 years: 3.7 hours; 8 to 10 years: 5.4 hours
Adults, normal renal function: 8 to 10 hours
Protein Binding
~44%
Use in Specific Populations
Special Populations: Renal Function Impairment
Half-life is prolonged.
Use: Labeled Indications
Cystitis, acute uncomplicated, treatment (tablets, oral solution): Treatment of initial episodes of uncomplicated urinary tract infections due to susceptible strains of Escherichia coli, Proteus mirabilis, Klebsiella pneumoniae, Enterobacter species and coagulase-negative Staphylococcus species, including S. saprophyticus.
Otitis media, acute (oral solution): Treatment of acute otitis media in pediatric patients due to susceptible strains of Streptococcus pneumoniae and Haemophilus influenzae.
Use: Off Label
Acne vulgariscyes
Data from a limited number of controlled and noncontrolled trials suggest that trimethoprim may be beneficial for the treatment of acne vulgaris. Additional data may be necessary to further define the role of trimethoprim in this condition.
Based on the
Pneumocystis pneumonia, treatment of mild to moderate infectionyes
Based on the US Department of Health and Human Services (HHS) Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents and the HHS Guidelines for the Prevention and Treatment of Opportunistic Infections Among HIV-exposed and HIV-infected Children, trimethoprim (in combination with dapsone) is an effective and recommended alternative agent for the treatment of mild to moderate Pneumocystis pneumonia (PCP) in HIV-infected patients.
Urinary tract infection, prophylaxisb
Data from a double-blind, placebo-controlled trial and 2 other studies support the use of trimethoprim in the prophylaxis of recurrent urinary tract infection in women with ≥2 episodes of infection in the previous year (Brumfitt 1983; Kasanen 1974; Stamm 1980); clinical experience also suggests the utility of trimethoprim in the prophylaxis of recurrent urinary tract infection (Kodner 2010). Additional trials may be necessary to further define the role of trimethoprim in this condition.
Contraindications
Hypersensitivity to trimethoprim or any component of the formulation; megaloblastic anemia due to folate deficiency
Dosage and Administration
Dosing: Adult
Cystitis (acute uncomplicated), treatment: Oral: 100 mg every 12 hours for 3 days (Gupta 2011)
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice. 200 mg once daily.
Acne vulgaris (alternative therapy) (off-label use): Oral: 100 mg 3 times daily or 300 mg twice daily (Amin 2007; Cunliffe 1999). The shortest possible duration should be used to minimize development of bacterial resistance; re-evaluate at 3 to 4 months (AAD [Zaenglein 2016])
Pneumocystis pneumonia, treatment of mild to moderate infection (alternative agent) (off-label use): Oral: 15 mg/kg/day in 3 divided doses in combination with dapsone for 21 days (HHS [adult] 2019)
Urinary tract infection (uncomplicated), prophylaxis (off-label use): Oral: 100 mg once daily (Brumfitt 1983; Kasanen 1974; Stamm 1980)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Otitis media, acute: Infants ≥6 months, Children, and Adolescents: Oral: 10 mg/kg/day in divided doses every 12 hours for 10 days; maximum daily dose: 400 mg/day
Urinary tract infection (uncomplicated), treatment: Infants ≥2 months, Children, and Adolescents: Oral: 4 to 6 mg/kg/day in divided doses every 12 hours (Kliegman 2011); Note: Preferred therapy is sulfamethoxazole and trimethoprim combined product (AAP 2011).
Pneumocystis jirovecii pneumonia (PCP), treatment: Children and Adolescents: Oral: 15 mg/kg/day in 3 divided doses for 21 days; in combination with dapsone; data in children is limited; preferred therapy is sulfamethoxazole and trimethoprim combined product (DHHS [adult and pediatric] 2013)
Extemporaneously Prepared
Note: Commercial oral solution is available (10 mg/mL [dye free, ethanol free; contains propylene glycol, sodium benzoate; bubblegum flavor])
A 10 mg/mL oral suspension may be made with tablets. Crush ten 100 mg tablets in a mortar and reduce to a fine powder. Add 20 mL of a 1:1 mixture of Simple Syrup, NF, and Methylcellulose 1% and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 100 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 100 mL. Label "shake well" and "refrigerate". Stable for 91 days.
Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Administer without regard to food; may administer with milk or food if GI upset occurs.
Dietary Considerations
May cause folic acid deficiency, supplements may be needed.
Storage
Solution: Store between 15°C to 25°C (59°F to 77°F). Protect from light.
Tablets: Store at 20°C to 25°C (68°F to 77°F). Protect from light.
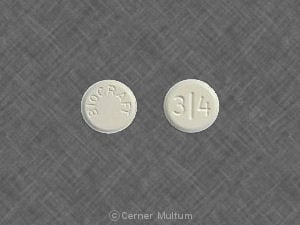
Trimethoprim Images
Drug Interactions
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Amantadine: Trimethoprim may enhance the adverse/toxic effect of Amantadine. Specifically, the risk of myoclonus and/or delirium may be increased. Amantadine may increase the serum concentration of Trimethoprim. Trimethoprim may increase the serum concentration of Amantadine. Monitor therapy
Amodiaquine: Trimethoprim may enhance the neutropenic effect of Amodiaquine. Trimethoprim may increase the serum concentration of Amodiaquine. Avoid combination
Angiotensin II Receptor Blockers: Trimethoprim may enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Trimethoprim may enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
AzaTHIOprine: Trimethoprim may enhance the myelosuppressive effect of AzaTHIOprine. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapsone (Systemic): Trimethoprim may increase the serum concentration of Dapsone (Systemic). Dapsone (Systemic) may increase the serum concentration of Trimethoprim. Monitor therapy
Dapsone (Topical): Trimethoprim may enhance the adverse/toxic effect of Dapsone (Topical). More specifically, trimethoprim may increase the risk for hemolysis Monitor therapy
Digoxin: Trimethoprim may increase the serum concentration of Digoxin. Monitor therapy
Dofetilide: Trimethoprim may increase the serum concentration of Dofetilide. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP2C9 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C9 substrate should be performed with caution and close monitoring. Consider therapy modification
Eplerenone: Trimethoprim may enhance the hyperkalemic effect of Eplerenone. Monitor therapy
Fosphenytoin: May decrease the serum concentration of Trimethoprim. Trimethoprim may increase the serum concentration of Fosphenytoin. Management: Consider alternatives to this combination when possible, to avoid potential decreased trimethoprim efficacy and increased phenytoin concentrations/effects. Monitor patients receiving this combination closely for both of these possible effects. Consider therapy modification
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
LamiVUDine: Trimethoprim may increase the serum concentration of LamiVUDine. Monitor therapy
Leucovorin Calcium-Levoleucovorin: May diminish the therapeutic effect of Trimethoprim. Management: Avoid concurrent use of leucovorin or levoleucovorin with trimethoprim (plus sulfamethoxazole) for Pneumocystis jirovecii pneumonia. If trimethoprim is used for another indication, monitor closely for reduced efficacy. Avoid combination
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Lumacaftor and Ivacaftor may increase the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Monitor therapy
Memantine: Trimethoprim may enhance the adverse/toxic effect of Memantine. Specifically, the risk of myoclonus and/or delirium may be increased. Trimethoprim may increase the serum concentration of Memantine. Memantine may increase the serum concentration of Trimethoprim. Monitor therapy
Mercaptopurine: Trimethoprim may enhance the myelosuppressive effect of Mercaptopurine. Monitor therapy
MetFORMIN: Trimethoprim may increase the serum concentration of MetFORMIN. Monitor therapy
Methotrexate: Trimethoprim may enhance the adverse/toxic effect of Methotrexate. Management: Consider avoiding concomitant use of methotrexate and either sulfamethoxazole or trimethoprim. If used concomitantly, monitor for the development of signs and symptoms of methotrexate toxicity (e.g., bone marrow suppression). Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP2C9 Substrates (High risk with Inhibitors). Management: Use CYP2C9 substrates at the lowest recommended dose, and monitor closely for adverse effects, during and in the 2 weeks following mifepristone treatment. Consider therapy modification
Phenytoin: Trimethoprim may increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Trimethoprim. Management: Consider alternatives to this combination when possible, to avoid potential decreased trimethoprim efficacy and increased phenytoin concentrations/effects. Monitor patients receiving this combination closely for both of these possible effects. Consider therapy modification
PRALAtrexate: Trimethoprim may increase the serum concentration of PRALAtrexate. More specifically, trimethoprim may decrease excretion of pralatrexate. Management: Closely monitor for increased pralatrexate serum level and/or possible toxicity with concomitant use of trimethoprim. Monitor for decreased pralatrexate levels with discontinuation of trimethoprim. Monitor therapy
Procainamide: Trimethoprim may increase serum concentrations of the active metabolite(s) of Procainamide. Trimethoprim may increase the serum concentration of Procainamide. Consider therapy modification
Pyrimethamine: May enhance the adverse/toxic effect of Trimethoprim. Monitor therapy
Repaglinide: CYP2C8 Inhibitors (Weak) may increase the serum concentration of Repaglinide. Monitor therapy
RifAMPin: May decrease the serum concentration of Trimethoprim. Monitor therapy
Rifapentine: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Sapropterin: Trimethoprim may decrease the serum concentration of Sapropterin. Specifically, trimethoprim may decrease tissue concentrations of tetrahydrobiopterin. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Spironolactone: Trimethoprim may enhance the hyperkalemic effect of Spironolactone. Monitor therapy
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Varenicline: Trimethoprim may increase the serum concentration of Varenicline. Management: Monitor for increased varenicline adverse effects with concomitant use of trimethoprim, particularly in patients with severe renal impairment. International product labeling recommendations vary. Consult appropriate labeling. Monitor therapy
Test Interactions
May falsely increase (~10%) creatinine determination measured by the Jaffé alkaline picrate assay; may interfere with determination of serum methotrexate when measured by methods that use a bacterial dihydrofolate reductase as the binding protein (eg, the competitive binding protein technique); does not interfere with RIA for methotrexate
Adverse Reactions
Frequency not always defined.
Dermatologic: Maculopapular rash (200 mg/day: 3% to 7%; incidence higher with larger daily doses), phototoxicity, pruritus (common)
Endocrine & metabolic: Hyperkalemia, hyponatremia
Gastrointestinal: Epigastric distress, glossitis, nausea, vomiting
Hematologic & oncologic: Leukopenia, megaloblastic anemia, methemoglobinemia, neutropenia, thrombocytopenia
Hepatic: Increased liver enzymes
Hypersensitivity: Anaphylaxis, hypersensitivity reaction
Renal: Increased blood urea nitrogen, increased serum creatinine
Miscellaneous: Fever
1%, postmarketing, and/or case reports: Aseptic meningitis, cholestatic jaundice, erythema multiforme, exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- Hematologic effects: May rarely interfere with hematopoiesis, especially with large doses or long term therapy; monitor patients on long term therapy for signs/symptoms of hematologic disorders.
- Hyperkalemia: May cause hyperkalemia; potential risk factors include high dosage (20 mg/kg/day), renal impairment, older age, hypoaldosteronism, and concomitant use of medications causing or exacerbating hyperkalemia (Perazella 2000).
- Hypersensitivity: Serious hypersensitivity reactions have been reported (rarely).
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Renal impairment: Use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Elderly patients may be at risk for hyperkalemia with trimethoprim use and are at an increased risk for severe and potentially life-threatening hyperkalemia when trimethoprim is used concomitantly with medications known to cause or exacerbate hyperkalemia, such as spironolactone, ACE inhibitors, or ARBs (Antoniou 2010; Antoniou 2011; Antoniou 2015).
- Patients with potential for folate deficiency: Use with caution in patients with potential folate deficiency (malnourished, chronic anticonvulsant therapy, or elderly).
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP ["Inactive" 1997]; Zar 2007).
Other warnings/precautions:
- Appropriate use: Otitis media: Not indicated for prophylactic or prolonged administration in otitis media at any age.
Monitoring Parameters
CBC with differential, platelet count, liver enzyme tests, bilirubin, serum potassium, serum creatinine, and BUN periodically during long-term therapy
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Trimethoprim crosses the placenta.
Trimethoprim may affect folic acid metabolism; adverse fetal events may be associated with maternal trimethoprim use immediately prior to or during pregnancy (Andersen 2013a; Andersen 2013b; Mølgaard-Nielsen 2012; Sun 2014).
Studies evaluating the effects of trimethoprim administration in pregnancy have also been conducted with Sulfamethoxazole and Trimethoprim (see sulfamethoxazole/trimethoprim monograph for details).
Patient Education
What is this drug used for?
- It is used to treat bacterial infections.
Frequently reported side effects of this drug
- Diarrhea
- Nausea
- Vomiting
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Methemoglobinemia like blue or gray color of the lips, nails, or skin; abnormal heartbeat; seizures; severe dizziness or passing out; severe headache; fatigue; loss of strength and energy; or shortness of breath.
- Electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting.
- Chills
- Sore throat
- Pale skin
- Bruising
- Bleeding
- Purple patches on skin or mouth
- Clostridium difficile (C. diff)-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.