Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Suspension Reconstituted, Intramuscular:
Trelstar: 3.75 mg (1 ea [DSC]); 11.25 mg (1 ea [DSC]) [contains polysorbate 80]
Trelstar Mixject: 3.75 mg (1 ea [DSC]); 11.25 mg (1 ea [DSC]); 22.5 mg (1 ea [DSC]) [contains polysorbate 80]
Suspension Reconstituted, Intramuscular [preservative free]:
Trelstar Mixject: 3.75 mg (1 ea); 11.25 mg (1 ea); 22.5 mg (1 ea) [contains polysorbate 80]
Suspension Reconstituted ER, Intramuscular:
Triptodur: 22.5 mg (1 ea) [contains polysorbate 80]
Pharmacology
Mechanism of Action
Triptorelin is an agonist analog of gonadotropin releasing hormone (GnRH) and causes suppression of ovarian and testicular steroidogenesis due to decreased levels of LH and FSH with subsequent decrease in testosterone (male) and estrogen (female) levels. After chronic and continuous administration, usually 2 to 4 weeks after initiation, a sustained decrease in LH and FSH secretion occurs. When used for assisted reproductive technologies (ART), prevents premature LH surge in women undergoing controlled ovarian hyperstimulation.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: 30 to 33 L
Metabolism
Unknown; unlikely to involve CYP; no known metabolites
Excretion
Urine (42% as intact peptide); hepatic
Time to Peak
Trelstar: 1 to 3 hours; Triptodur: 4 hours
Half-Life Elimination
2.8 ± 1.2 hours
Moderate-to-severe renal impairment: 6.6 to 7.7 hours
Hepatic impairment: 7.6 hours
Protein Binding
None
Use in Specific Populations
Special Populations: Renal Function Impairment
There is a decrease in total Cl proportional to decrease in CrCl and increased Vd and half-life. Patients with renal impairment had 2- to 4-fold higher exposure (AUC) values than younger healthy men.
Special Populations: Hepatic Function Impairment
The decrease in triptorelin Cl is more pronounced. Triptorelin half-life increase is similar to renal impairment. Patients with hepatic impairment had 2- to 4-fold higher exposure (AUC) values than younger healthy men.
Special Populations: Elderly
Triptorelin clearance is partly correlated to total CrCl, which is well known to decrease with age.
Use: Labeled Indications
Central precocious puberty: Triptodur: Treatment of central precocious puberty in patients 2 years and older
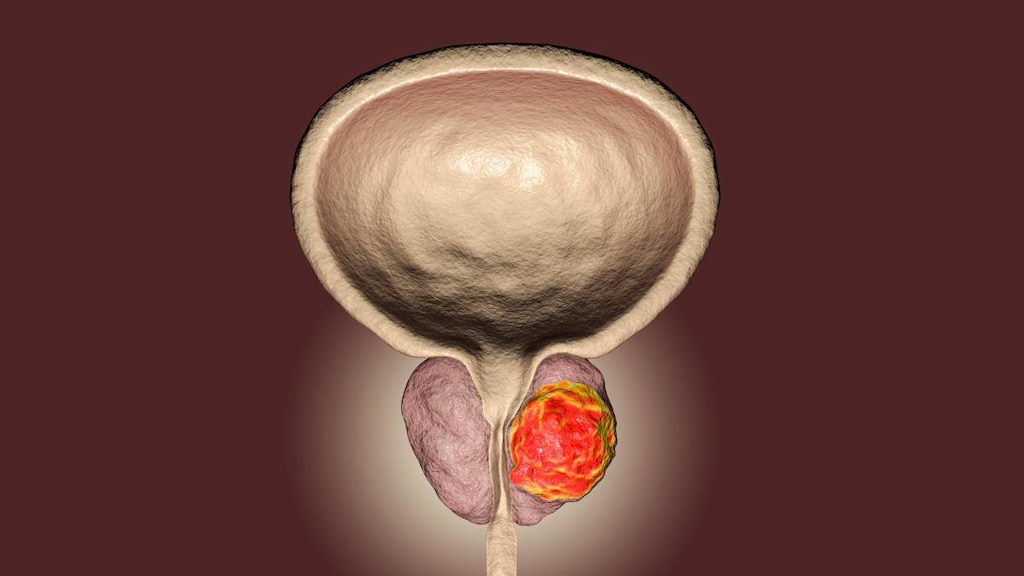
Prostate cancer (advanced): Trelstar: Palliative treatment of advanced prostate cancer
Assisted reproductive technologies: Decapeptyl [Canadian product]: Adjunctive therapy in women undergoing controlled ovarian hyperstimulation for assisted reproductive technologies (ART)
Use: Off Label
Endometrial stromal sarcomacyes
Data from a limited number of case reports and clinical experience suggest triptorelin may be beneficial in the treatment of endometrial stromal sarcoma Burke 2004, Jin 2015. Clinical experience also suggests the utility of gonadotropin-releasing hormone receptor analogs, including triptorelin may be of benefit in the treatment of endometrial stromal sarcoma Amant 2009, ESMO 2012. Additional studies are necessary to further define the role of triptorelin in the management of this condition.
Endometriosiscyes
Data from a small multicenter clinical trial and from a small randomized, double blind, placebo control study suggest that triptorelin may be beneficial in the treatment of endometriosis Bergqvist 1998, Choktanasiri 1996.
Based on the American College of Obstetricians and Gynecologists (ACOG) Management of Endometriosis Guidelines and the Society of Obstetricians and Gynaecologists of Canada (SOGC) Endometriosis Diagnosis and Management Guidelines, empiric therapy with a GnRH agonist is effective (as second-line therapy) in the management of pain associated with endometriosis once other causes have been excluded and treatment with preferred initial therapies have failed ACOG 114 2010, SOGC [Leyland 2010].
Paraphilia/hypersexualityyes
Based on The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Paraphilias, triptorelin given for paraphilia/hypersexuality is an effective and recommended treatment option in the management of this condition.
Contraindications
Known hypersensitivity to triptorelin or any component of the formulation, other GnRH agonists or GnRH; pregnancy
Canadian labeling: Additional contraindications (not in the US labeling): Breastfeeding women
Dosage and Administration
Dosing: Adult
Prostate cancer (advanced): Trelstar: IM:
3.75 mg once every 4 weeks or
11.25 mg once every 12 weeks or
22.5 mg once every 24 weeks
Controlled ovarian hyperstimulation for assisted reproductive technologies (ART) (adjunctive therapy): Decapeptyl (Canadian product): Females: SubQ: Usual dose: 0.1 mg once daily initiated on day 2 or 3 or days 21 to 23 of menstrual cycle (or 5 to 7 days prior to expected onset of menses). Dose may be adjusted according to ovarian response as measured by ovarian ultrasound with or without serum estradiol levels. Treatment is continued until follicles achieve suitable size (typically 4 to 7 weeks).
Endometrial stromal sarcoma (off-label use): IM: 3.75 mg once every 28 days for ~3 to 5 months (Jin 2015). Additional studies are necessary to further define the role of triptorelin in the management of this condition.
Endometriosis (off-label use): IM: 3.75 mg once every 4 weeks for a total of 6 doses (Bergqvist 1998; Choktanasiri 1996) or 3.75 mg once every 6 weeks for a total of 4 doses (Tse 2000) or 11.25 mg once every 3 months (Donnez 2004). Hormonal add-back therapy (such as estrogens or progestins) is recommended at the start of treatment to reduce bone mineral loss (Dunselman 2014; SOGC [Leyland 2010]). Duration of therapy is not well established (Dunselman 2014) but should be evaluated after 3 months (SOGC [Leyland 2010]); in general, use of GnRH agonists is limited to less than 6 or 12 months due to adverse events (Leone Roberti Maggiore 2014).
Treatment of paraphilia/hypersexuality (off-label use) (Guay 2009; Thibaut 1993): Males:
Note: May cause an initial increase in androgen concentrations, which may be treated with an antiandrogen (eg, flutamide, cyproterone) for 1 to 2 months (Guay 2009). Avoid use in patients with osteoporosis or active pituitary pathology.
SubQ: Test dose: 1 mg (observe for hypersensitivity); if tolerated, follow with monthly IM injections
IM: 3.75 mg monthly
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Central precocious puberty: Children ≥2 years: Triptodur: IM: 22.5 mg once every 24 weeks; discontinue therapy at appropriate age of onset of puberty.
Reconstitution
MixJect System: Follow manufacturer's instructions for mixing prior to use.
Trelstar: Reconstitute with 2 mL sterile water for injection. Shake well to obtain a uniform suspension. Solution will appear milky. Administer immediately after reconstitution.
Triptodur: Reconstitute with 2 mL sterile water for injection. Agitate the vial for 30 to 60 seconds to obtain a milky and homogenous suspension. Administer immediately after reconstitution to avoid separation of the suspension. Refer to manufacturer’s labeling for detailed preparation instructions.
Administration
IM: Administer by IM injection into the buttock (Trelstar) or into the buttock or thigh (Triptodur); alternate injection sites. Administer immediately after reconstitution. Must administer under the supervision of a health care provider.
Decapeptyl [Canadian product] is administered by subcutaneous injection into the lower abdomen; alternate injection sites. If a dose is missed, it can be administered on the same day; however, do not double doses. Must administer under the supervision of a health care provider.
Storage
Trelstar: Store at 20°C to 25°C (68°F to 77°F). Do not freeze MIXJECT system. Administer immediately after reconstitution.
Triptodur: Store at 20°C to 25°C (68°F to 77°F). Do not freeze.
Decapeptyl [Canadian product]: Store at 2°C to 8°C (36°F to 46°F); do not freeze. Protect from light.
Drug Interactions
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Choline C 11: Luteinizing Hormone-Releasing Hormone Analogs may diminish the therapeutic effect of Choline C 11. Monitor therapy
Corifollitropin Alfa: Luteinizing Hormone-Releasing Hormone Analogs may enhance the therapeutic effect of Corifollitropin Alfa. Avoid combination
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Indium 111 Capromab Pendetide: Luteinizing Hormone-Releasing Hormone Analogs may diminish the diagnostic effect of Indium 111 Capromab Pendetide. Avoid combination
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Test Interactions
Pituitary-gonadal function may be suppressed with chronic administration and for up to 8 weeks after triptorelin therapy has been discontinued.
Adverse Reactions
>10%:
Endocrine & metabolic: Hot flash (prostate cancer: 59% to 73%; central precocious puberty: 2% to 5%), increased serum glucose (prostate cancer)
Hematologic & oncologic: Decreased hemoglobin (prostate cancer), decreased red blood cells (prostate cancer)
Hepatic: Increased serum alanine aminotransferase (prostate cancer), increased serum aspartate aminotransferase (prostate cancer), increased serum transaminases (prostate cancer)
Local: Pain at injection site (central precocious puberty: 45%; prostate cancer: 4%), erythema at injection site (central precocious puberty: 14%)
Nervous system: Headache (2% to 14%)
Neuromuscular & skeletal: Skeletal pain (prostate cancer: 12% to 13%)
Renal: Increased blood urea nitrogen (prostate cancer)
Respiratory: Nasopharyngitis (central precocious puberty: 14%)
1% to 10%:
Cardiovascular: Lower extremity edema (prostate cancer: 6%), hypertension (prostate cancer: ≤4%; central precocious puberty), chest pain (prostate cancer: 2%), peripheral edema (prostate cancer: 1%)
Dermatologic: Injection site pruritus (central precocious puberty: 2%), skin rash (prostate cancer: 2%), pruritus (prostate cancer: 1%)
Endocrine & metabolic: Decreased libido (prostate cancer: 2%), dependent edema (prostate cancer: 2%), gynecomastia (prostate cancer: 2%)
Gastrointestinal: Gastroenteritis (central precocious puberty: 7%), nausea (prostate cancer: 3%), anorexia (prostate cancer: 2%), constipation (prostate cancer: 2%), dyspepsia (prostate cancer: 2%), vomiting (prostate cancer: 2%), abdominal pain (prostate cancer: 1%), diarrhea (prostate cancer: 1%)
Genitourinary: Erectile dysfunction (prostate cancer: 10%), menstruation (central precocious puberty: 8%), testicular atrophy (prostate cancer: 8%), impotence (prostate cancer: 2% to 7%), dysuria (prostate cancer: 5%), mastalgia (prostate cancer: 2%), urinary retention (prostate cancer: 1%), urinary tract infection (prostate cancer: 1%)
Hematologic & oncologic: Anemia (prostate cancer: 1%)
Hepatic: Increased serum alkaline phosphatase (≥2%), hepatic insufficiency (prostate cancer: 1%)
Infection: Influenza (central precocious puberty: 5%)
Local: Swelling at injection site (central precocious puberty: 2%)
Nervous system: Pain (prostate cancer: 2% to 3%), dizziness (prostate cancer: 1% to 3%), anxiety (central precocious puberty: 2%), fatigue (prostate cancer: 2%), mood changes (central precocious puberty: 2%), insomnia (prostate cancer: ≤2%), emotional lability (≤1%)
Neuromuscular & skeletal: Lower extremity pain (prostate cancer: 2% to 5%), back pain (prostate cancer: ≤3%), lower limb cramps (prostate cancer: 2%), arthralgia (prostate cancer: ≤2%), asthenia (prostate cancer: 1%), myalgia (prostate cancer: 1%)
Ophthalmic: Conjunctivitis (prostate cancer: 1%), eye pain (prostate cancer: 1%)
Otic: Otitis externa (central precocious puberty: 5%)
Respiratory: Upper respiratory tract infection (central precocious puberty: 9%), cough (central precocious puberty: 7%; prostate cancer: 2%), bronchitis (central precocious puberty: 5%), pharyngitis (central precocious puberty: 5%; prostate cancer: 1%), sinusitis (central precocious puberty: 5%), dyspnea (prostate cancer: 1%)
Miscellaneous: Postoperative pain (reproductive studies: 3% to 4%), missed abortion (reproductive studies: 2%)
Frequency not defined: Endocrine & metabolic: Increased testosterone level
<1%, postmarketing, and/or case reports: Altered gonadal hormone levels (pituitary-gonadal axis suppression), anaphylactic shock, anaphylactoid shock, angioedema, cerebrovascular accident, deep vein thrombosis, hypersensitivity reaction, interstitial pulmonary disease, intracranial hypertension (Tan 2019), limb pain, myocardial infarction, pituitary apoplexy, pulmonary embolism, seizure, thrombophlebitis, transient ischemic attacks, urticaria, visual disturbance, visual impairment
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular effects: Androgen-deprivation therapy (ADT) may increase the risk for cardiovascular disease (Levine 2010). Myocardial infarction, sudden cardiac death and stroke have been reported in men receiving GnRH agonists. ADT may prolong the QT/QTc interval; consider the benefits of ADT versus the risk for QT prolongation in patients with a history of QTc prolongation, congenital long QT syndrome, heart failure, frequent electrolyte abnormalities, and in patients with medications known to prolong the QT interval. Consider periodic monitoring of electrocardiograms and electrolytes in at-risk patients.
- Decreased bone density: Use with caution in patients with risk factors for decreased bone mineral density; GnRH agonist therapy may increase risk for osteoporosis and bone fractures particularly with prolonged use.
- Hyperglycemia: Hyperglycemia and an increased risk of developing diabetes has been reported with therapy and may manifest as diabetes or worsening of glycemic control in patients with diabetes. Monitor blood glucose and/or glycosylated hemoglobin (HbA1c) as clinically necessary.
- Hypersensitivity reactions: Angioedema and anaphylactic shock have occurred; discontinue use if severe reaction occurs.
- Ovarian hyperstimulation syndrome: Decapeptyl [Canadian product]: Ovarian hyperstimulation syndrome (OHSS) is a rare exaggerated response to ovulation induction therapy (Corbett 2014; Fiedler 2012). This syndrome may begin within 24 hours of treatment but may become most severe 7 to 10 days after therapy (Corbett 2014). Symptoms of mild/moderate OHSS may include abdominal distention/discomfort, diarrhea, nausea, and/or vomiting. Severe OHSS symptoms may include severe abdominal pain, anuria/oliguria, ascites, severe dyspnea, hypotension, or nausea/vomiting (intractable). Decreased creatinine clearance, hemoconcentration, hypoproteinemia, elevated liver enzymes, elevated WBC, and electrolyte imbalances may also be present (ASRM 2016; Corbett 2014; Fiedler 2012). Treatment is primarily symptomatic and includes fluid and electrolyte management, analgesics, and prevention of thromboembolic complications (ASRM 2016; SOGC-CFAS 2011). Therapy with gonadotropins should be stopped.
- Pituitary apoplexy: Rare cases of pituitary apoplexy (frequently secondary to pituitary adenoma) have been observed with GnRH agonist administration (onset from 1 hour to usually <2 weeks); may present as sudden headache, vomiting, visual or mental status changes, and infrequently cardiovascular collapse; immediate medical attention required.
- Psychiatric effects: Symptoms of emotional lability (eg, crying, irritability, anger, aggression, impatience) have been reported with GnRH agonists, including triptorelin; monitor for the development or worsening of psychiatric symptoms.
- Seizures: Seizures have been reported with GnRH agonists, including triptorelin in patients with or without a history of seizures or other conditions or concurrent medications associated with seizures.
- Spinal cord compression: Cases of spinal cord compression, which may contribute to weakness or paralysis (possible fatal complications), have been reported; observe patients with metastatic vertebral lesions closely during the first few weeks of treatment.
- Symptom flare: Transient initial increases in gonadotropins and sex steroids leading to a worsening of symptoms may be observed during the first few weeks of therapy or after subsequent doses. Patients with prostate cancer may experience new or increased bone pain, neuropathy, hematuria, or urethral or bladder outlet obstruction. Female patients with central precocious puberty may experience transient vaginal bleeding.
Disease-related concerns:
- Urinary tract obstruction: Observe patients with urinary tract obstruction closely during the first few weeks of treatment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Monitoring Parameters
Glucose and HbA1c (periodically), signs and symptoms of emerging cardiovascular disease; consider periodic monitoring of electrocardiograms and electrolytes in at-risk patients; development/worsening of psychiatric symptoms.
Additional monitoring (per indication):
Treatment of precocious puberty: Monitor response to therapy with LH levels after a GnRH or GnRH agonist stimulation test, basal LH, or serum sex steroid levels beginning 1 to 2 months after initiation of therapy, during therapy, and with each subsequent dose; height every 3 to 6 months; bone age (periodically)
Prostate cancer: Serum testosterone levels, prostate-specific antigen; bone density.
Assisted reproductive technologies: Decapeptyl [Canadian product]: Negative pregnancy test prior to initiation of therapy; signs/symptoms of allergic reaction for 30 minutes after administration; ultrasound and/or estradiol levels to assess follicle development; ultrasound to assess number and size of follicles
OHSS: Monitoring of hospitalized patients should include abdominal circumference, albumin, cardiorespiratory status, electrolytes, fluid balance, hematocrit, hemoglobin, serum creatinine, urine output, urine specific gravity, vital signs, weight (daily or as necessary) and liver enzymes (weekly) (SOGC-CFAS 2011).
Treatment of paraphilia/hypersexuality (off-label use): The following monitoring has been recommended for other GnRH agonists: CBC (baseline, monthly for 4 months then every 6 months); serum testosterone (baseline, monthly for 4 months then every 6 months); serum LH (baseline and every 6 months), FSH (baseline), serum BUN and creatinine (baseline and every 6 months); bone density (baseline and yearly); ECG (baseline) (Reilly 2000)
Pregnancy
Pregnancy Considerations
Based on the mechanism of action and data from animal reproduction studies, in utero exposure to triptorelin may cause fetal harm.
Hormonal changes that occur with therapy may increase the risk of pregnancy loss. Therefore, use is contraindicated in females who are pregnant. Information following inadvertent exposure in early pregnancy is limited (Elefant 1995).
When used for assisted reproductive technologies (ART; not an approved use in the US), pregnancy must be ruled out prior to therapy and nonhormonal contraception should be used until menses occurs. Due to the short half-life of triptorelin (formulations used for ART), it is not expected to be present in the maternal serum at the time of embryo transfer.
Based on the mechanism of action, may impair fertility in males of reproductive potential.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience sexual dysfunction, hot flashes, nausea, injection site irritation, or trouble sleeping. Have patient report immediately to prescriber signs of pituitary apoplexy (sudden headache, vomiting, passing out, mood changes, eye weakness, unable to move eyes, or vision changes), signs of high blood sugar (confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit), signs of a urinary tract infection (blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain), signs of severe cerebrovascular disease (change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes), chest pain, shortness of breath, excessive weight gain, swelling of arms or legs, difficult urination, severe headache, severe dizziness, passing out, vision changes, back pain, blood in the urine, burning or numbness feeling, fast heartbeat, abnormal heartbeat, chills, sore throat, behavioral changes, mood changes, severe muscle pain, severe joint pain, severe loss of strength and energy, difficulty moving, muscle weakness, or bone pain (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.