Boxed Warning
For IV use only:
For IV use only - fatal if given by other routes. Death has occurred with intrathecal administration.
Do not interchange:
Vincristine (liposomal) injection has different dosage recommendations than vincristine injection. Verify drug name and dose prior to preparation and administration to avoid overdosage.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension, Intravenous, as sulfate [preservative free]:
Marqibo: 5 mg/31 mL (1 ea)
Pharmacology
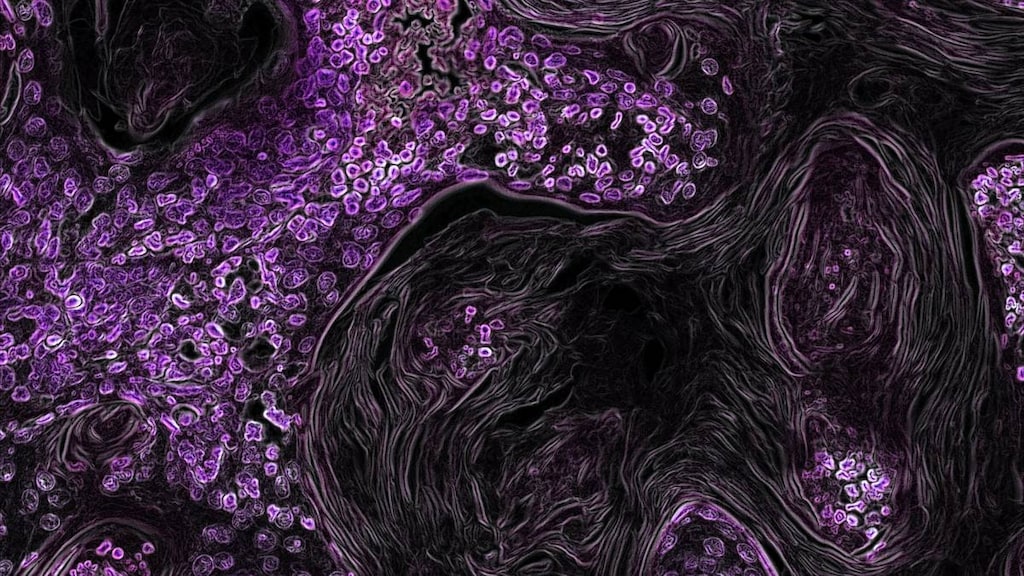
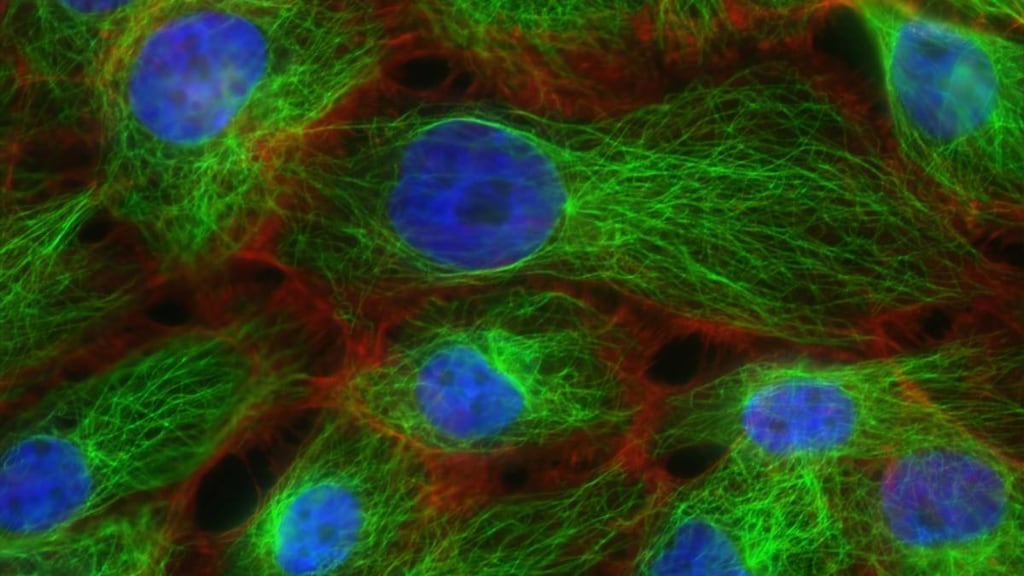
Mechanism of Action
The vincristine liposomal formulation increases the half-life, allowing for enhanced cytotoxic activity in tumor cells. The liposomal formulation of vincristine consists of vincristine encapsulated in sphingosomes, which are composed of sphingomyelin and cholesterol (Bedikian 2006).
Pharmacokinetics/Pharmacodynamics
Distribution
Vdss: 2.7 L (Bedikian 2006)
Metabolism
Primarily hepatic
Excretion
Feces (69%); urine (<8%)
Half-Life Elimination
45 hours (urinary half-life); dependent on rate of vincristine release from sphingosome (Bedikian 2006)
Use: Labeled Indications
Acute lymphoblastic leukemia (relapsed): Treatment of relapsed Philadelphia chromosome-negative (Ph-) acute lymphoblastic leukemia (ALL) in adult patients in second or greater relapse or whose disease has progressed after two or more antileukemic therapies.
Contraindications
Hypersensitivity to vincristine, liposomal vincristine, or any component of the formulation; patients with Charcot-Marie-Tooth syndrome or other demyelinating conditions; administration via the intrathecal route
Dosage and Administration
Dosing: Adult
Note: Vincristine liposomal and conventional vincristine are NOT interchangeable. Dosing differs between formulations; verify intended product and dose prior to preparation and administration. The liposomal vincristine dose is based on actual body surface area (BSA) and was not capped in studies (O'Brien 2009; Rodriguez 2009; Silverman, 2010).
Acute lymphoblastic leukemia (relapsed; Philadelphia chromosome-negative): IV: 2.25 mg/m2 once every 7 days
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Demyelinating conditions (including Charcot-Marie-Tooth syndrome): Use is contraindicated.
Fatigue, severe: Consider dose delay, reduction, or therapy discontinuation.
Hematologic toxicity: Grade 3 or 4 neutropenia, thrombocytopenia, or anemia: Consider dose reduction or modification.
Peripheral neuropathy:
Grade 3 or persistent grade 2 toxicity: Interrupt therapy until recovery to grade 1 or 2, then reduce dose to 2 mg/m2. If grade 3 toxicity persists or if grade 4 toxicity occurs, discontinue liposomal vincristine.
Persistent grade 2 toxicity after first dose reduction to 2 mg/m2: Interrupt therapy for up to 7 days until recovery to grade 1, then reduce dose to 1.825 mg/m2. If neuropathy increases to grade 3 or 4, discontinue liposomal vincristine.
Persistent grade 2 toxicity after second dose reduction to 1.825 mg/m2: Interrupt therapy for up to 7 days until recovery to grade 1, then reduce dose to 1.5 mg/m2. If neuropathy increases to grade 3 or 4, discontinue liposomal vincristine.
Pre-existing neuropathy, severe: Assess treatment benefit versus risk.
Reconstitution
Vincristine liposome preparation requires 60 to 90 minutes of dedicated time utilizing the manufacturer supplied kit. Do not reuse kit components with future doses.
Water bath process:
1). Outside the sterile area, fill a water bath to a depth of at least 8 cm (3.2 inches); water should be heated to and maintained at 63°C to 67°C (145.4°F to 152.6°F) for the entire procedure (use calibrated thermometer to monitor temperature). Maintain water depth of at least 8 cm (3.2 inches) throughout process. Water bath must remain outside the sterile area.
2). In a biological safety cabinet, vent the sodium phosphate vial with a sterile venting needle (with a 0.2 micron filter or other suitable venting device). Venting needle should always be kept above liquid level. Remove 1 mL of sphingomyelin/cholesterol liposome injection and inject into the sodium phosphate vial. Withdraw 5 mL of vincristine sulfate injection and inject into the sodium phosphate vial. Remove the venting needle and gently invert the sodium phosphate vial 5 times to mix (do not shake). Place flotation ring on the sodium phosphate vial.
3). Confirm the water bath is maintained between 63°C to 67°C (145.4°F to 152.6°F). Outside the sterile area, place constituted sodium phosphate vial in the water bath for 10 minutes. Record constitution start and stop time, as well as starting and ending water temperature. After 10 minutes, remove the vial (with tongs), remove flotation ring, then dry the vial, affix vial overlabel, and gently invert 5 times to mix (do not shake).
Block heater process (do NOT use water):
1). Arrange the 3 heater blocks in the block heater; the block holding the constitution vial is centered between the 2 other blank heater blocks (refer to manufacturer labeling for further information). Place a calibrated thermometer in the block opening adjacent to the vial well; thermometer should remain in the block opening through preparation. Turn on block heater and set to 75°C (167°F); verify block temperature (temperature should be 75°C ± 2°C). Equilibrate at this temperature for 15 minutes; maintain block temperature throughout procedure. The flotation ring included in the kit is not required with the block heater process.
2). In a biological safety cabinet, vent the sodium phosphate vial with a sterile venting needle (with a 0.2-micron filter or other suitable venting device). Venting needle should always be kept above liquid level. Remove 1 mL of sphingomyelin/cholesterol liposome injection and inject into the sodium phosphate vial. Withdraw 5 mL of vincristine sulfate injection and inject into the sodium phosphate vial. Remove the venting needle and gently invert the sodium phosphate vial 5 times to mix (do not shake).
3). Confirm the block heater temperature is 73°C to 77°C (163.4°F to 170.6°F). Outside the sterile area, place constituted sodium phosphate vial into the block heater for 18 minutes. Record constitution start and stop time, as well as starting and ending block heater temperature. After 18 minutes, remove the vial (with tongs), affix vial overlabel, and gently invert 5 times to mix (do not shake).
Following water or block heater process: Allow the vial to equilibrate for at least 30 minutes at room temperature (15°C to 30°C [59°F to 86°F]), but for no longer than 12 hours. Once prepared, vincristine sulfate liposome concentration is 5 mg per 31 mL (0.16 mg/mL). Return vial to biologic safety cabinet. Calculate patient's vincristine liposome dose (based on actual BSA); remove corresponding volume from 100 mL NS or D5W infusion bag. Inject vincristine liposome dose into the infusion bag (final volume of 100 mL). Do not use if a precipitate or other foreign matter is present in the vial or infusion bag. The amount contained in each vial may exceed the prescribed dose; use care with dosage and volume calculations. Discard unused portion of the vial. After preparation, keep liposomal vincristine in a location away from the separate storage location recommended for medications intended for CNS administration.
Administration
For IV administration only. Fatal if given by other routes. Liposomal vincristine should NOT be delivered to the patient at the same time as any medications intended for CNS administration.
IV: Infuse over 1 hour. Do not administer IV push or bolus; do not use with in-line filters. Do not administer with other medications. Infusion must be completed within 12 hours of preparation.
Conventional vincristine is a vesicant. Limited information is available regarding liposomal vincristine extravasation, but may cause inflammation if extravasated; avoid extravasation.
Storage
Store intact kit (containing vincristine vial, sphingomyelin/cholesterol liposome vial, and sodium phosphate vial) at 2°C to 8°C (36°F to 46°F); do not freeze. Use appropriate precautions for handling and disposal. Once prepared and diluted in D5W or NS, liposomal vincristine is stable for no more than 12 hours at room temperature. After preparation, keep liposomal vincristine in a location away from the separate storage location recommended for medications intended for CNS administration.
Drug Interactions
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of VinCRIStine (Liposomal). Avoid combination
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lenograstim: Antineoplastic Agents may diminish the therapeutic effect of Lenograstim. Management: Avoid the use of lenograstim 24 hours before until 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Lipegfilgrastim: Antineoplastic Agents may diminish the therapeutic effect of Lipegfilgrastim. Management: Avoid concomitant use of lipegfilgrastim and myelosuppressive cytotoxic chemotherapy. Lipegfilgrastim should be administered at least 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
MitoMYcin (Systemic): Antineoplastic Agents (Vinca Alkaloids) may enhance the adverse/toxic effect of MitoMYcin (Systemic). Specifically, the risk of pulmonary toxicity may be increased. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
NIFEdipine: May increase the serum concentration of VinCRIStine (Liposomal). Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Palifermin: May enhance the adverse/toxic effect of Antineoplastic Agents. Specifically, the duration and severity of oral mucositis may be increased. Management: Do not administer palifermin within 24 hours before, during infusion of, or within 24 hours after administration of myelotoxic chemotherapy. Consider therapy modification
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of VinCRIStine (Liposomal). Avoid combination
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Rifabutin: May decrease the serum concentration of VinCRIStine (Liposomal). Monitor therapy
Rifapentine: May decrease the serum concentration of VinCRIStine (Liposomal). Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
St John's Wort: May decrease the serum concentration of VinCRIStine (Liposomal). Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Teniposide: May enhance the neurotoxic effect of VinCRIStine (Liposomal). Monitor therapy
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Adverse Reactions
>10%:
Central nervous system: Fatigue (41%), peripheral neuropathy (39%; grades 3/4: 17%), insomnia (32%)
Gastrointestinal: Constipation (57%), nausea (52%), diarrhea (37%), decreased appetite (33%)
Hematologic & oncologic: Febrile neutropenia (38%; grades 3/4: 31%), anemia (34%; grades 3/4: 17%), neutropenia (grades 3/4: 18%), thrombocytopenia (grades 3/4: 17%)
Hepatic: Increased serum AST (grades 3/4: 6% to 11%)
Miscellaneous: Fever (43%)
1% to 10%:
Cardiovascular: Hypotension (grades 3/4: 6%), septic shock (grades 3/4: 6%)
Central nervous system: Pain (grades 3/4: 8%), mental status changes (grades 3/4: 4%), myasthenia (grades 3/4: 1%)
Gastrointestinal: Abdominal pain (grades 3/4: 8%), intestinal obstruction (grades 3/4: 6%)
Infection: Staphylococcal bacteremia (grades 3/4: 6%)
Neuromuscular & skeletal: Weakness (grades 3/4: 5%)
Respiratory: Pneumonia (grades 3/4: 8%), respiratory distress (grades 3/4: 6%), respiratory failure (grades 3/4: 5%)
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Grade 3 and greater neutropenia, anemia, and thrombocytopenia were observed in clinical trials. Monitor blood counts closely and adjust dose or withhold therapy if necessary.
- Constipation: Constipation, ileus, bowel obstruction, and colonic pseudo-obstruction have occurred with liposomal vincristine. Patients should be initiated on a prophylactic bowel regimen including a stool softener, dietary fiber, and hydration; laxative treatments may be considered.
- Fatigue: Severe fatigue was noted in clinical trials; treatment delay, dosage adjustment or discontinuation may be necessary.
- Hepatotoxicity: Hepatotoxicity (including fatal cases) and increased AST have been reported. Monitor hepatic function tests; reduce dose or interrupt therapy if necessary. Use caution in patients with hepatic impairment; conventional vincristine undergoes extensive hepatic metabolism. Liposomal vincristine has not been studied in patients with severe hepatic impairment. In a study in a limited number of melanoma patients with moderate (Child-Pugh class B) hepatic impairment secondary to liver metastases, Cmax and AUC were comparable to those in patients with normal hepatic function; patients with hepatic impairment received a liposomal vincristine dose of 1 mg/m2 every 2 weeks versus 2 mg/m2 in subjects with normal hepatic function (Bedikian 2011).
- Neurotoxicity: Neuropathies (sensory and motor) are common and cumulative. Neuropathy symptoms may include paresthesia, hyper-/hypoesthesia, hyporeflexia or areflexia, neuralgia, jaw pain, cranial neuropathy, ileus, arthralgia, myalgia, muscle spasm, and/or weakness. Evaluate neurologic status of patients closely prior to liposomal vincristine administration; neurologic toxicity risk is greater when given to patients with preexisting neuromuscular conditions or when used concomitantly with other neurotoxic agents. Treatment delay, dosage adjustment, and/or discontinuation may be necessary.
- Tumor lysis syndrome: Tumor lysis syndrome may occur as a consequence of therapy; monitor closely for signs and symptoms and manage accordingly.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information. Avoid concomitant therapy with strong CYP3A4 or P-glycoprotein (P-gp) inducers or inhibitors.
Dosage form specific issues:
- Liposomal vs conventional formulation dosing: [US Boxed Warning]: Vincristine liposomal and conventional vincristine are NOT interchangeable. Dosing differs between formulations; verify intended product and dose prior to preparation and administration to avoid overdoses.
Other warnings/precautions:
- Extravasation: Avoid extravasation of liposomal vincristine (conventional vincristine is a vesicant). Only individuals experienced with vesicant administration should administer liposomal vincristine. Check for proper needle placement; if extravasation occurs, discontinue liposomal vincristine infusion immediately and institute appropriate extravasation management procedures.
- For IV use only: [US Boxed Warning]: For IV administration only. Fatal if given by other routes; inadvertent intrathecal administration has resulted in death. Liposomal vincristine should NOT be prepared during the preparation of any medications intended for CNS administration. After preparation, keep liposomal vincristine in a location away from the separate storage location recommended for medications intended for CNS administration. Liposomal vincristine should NOT be delivered to the patient at the same time with any medications intended for CNS administration.
Monitoring Parameters
CBC with differential and platelets; hepatic function; signs/symptoms of peripheral neuropathy or other neurologic toxicities; sodium (in elderly patients; conventional vincristine may cause or exacerbate hyponatremia or syndrome of inappropriate antidiuretic hormone secretion); signs/symptoms of tumor lysis syndrome; symptoms of constipation; monitor infusion site for extravasation
Pregnancy
Pregnancy Considerations
Based on the mechanism of action and data from animal reproduction studies, in utero exposure to vincristine (liposomal) may cause fetal harm.
Females of reproductive potential should avoid becoming pregnant during therapy.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience lack of appetite or trouble sleeping. Have patient report immediately to prescriber signs of infection, signs of bleeding (vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding), signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), signs of tumor lysis syndrome (fast heartbeat or abnormal heartbeat; any passing out; unable to pass urine; muscle weakness or cramps; nausea, vomiting, diarrhea or lack of appetite; or feeling sluggish), burning or numbness feeling, change in reflexes, jaw pain, muscle pain, joint pain, muscle spasm, muscle weakness, severe or persistent nerve problems, severe constipation, severe abdominal pain, bloating, severe nausea, vomiting, severe diarrhea, severe loss of strength and energy, severe dizziness, passing out, or severe injection site pain burning, edema, or irritation (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for healthcare professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience and judgment in diagnosing, treating and advising patients.