Boxed Warning
Bleeding risk:
Do not use vorapaxar in patients with a history of stroke, transient ischemic attack, or intracranial hemorrhage; or active pathological bleeding. Antiplatelet agents, including vorapaxar, increase the risk of bleeding, including intracranial hemorrhage and fatal bleeding.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Zontivity: 2.08 mg
Pharmacology
Mechanism of Action
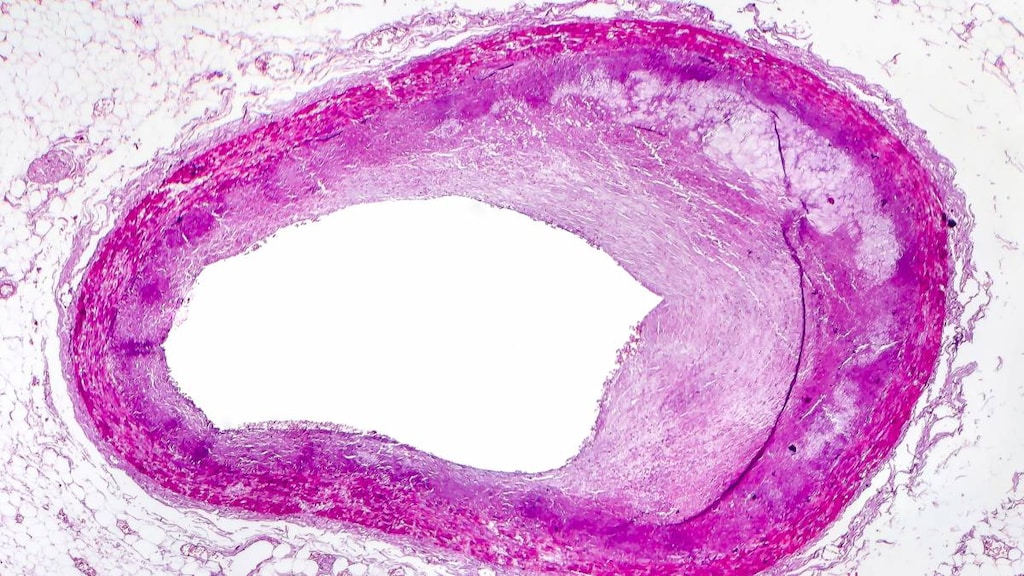
Vorapaxar, an antagonist of the protease-activated receptor-1 (PAR-1) expressed on platelets, inhibits thrombin-induced and thrombin receptor agonist peptide (TRAP)-induced platelet aggregation. Due to the very long half-life, vorapaxar is effectively irreversible. Vorapaxar reversibly binds to the PAR-1 receptor with a long receptor dissociation half-life of approximately 20 hours; additionally, vorapaxar displays significant inhibition of platelet aggregation that remains for up to 4 weeks after discontinuation due to the very long elimination half-life (Ueno 2010).
Pharmacokinetics/Pharmacodynamics
Absorption
Rapidly absorbed (Kosoglou 2012)
Distribution
~424 L
Metabolism
Hepatic via CYP3A4 and CYP2J2. Major active metabolite: M20 (accounts for ~20% of exposure to vorapaxar)
Excretion
Primarily in the form of metabolites through feces (58%); urine (25%)
Onset of Action
≥80% inhibition of TRAP-induced platelet aggregation within one week
Time to Peak
1 to 2 hours
Duration of Action
Dose and concentration dependent; with the recommended dosing, inhibition of TRAP-induced platelet aggregation at a level of 50% can be expected 4 weeks after discontinuation
Half-Life Elimination
Effective half-life: 3 to 4 days; Terminal elimination half-life (vorapaxar and active metabolite): ~8 days (range: 5 to 13 days)
Protein Binding
≥99% to albumin
Use: Labeled Indications
History of MI or established peripheral arterial disease: To reduce thrombotic cardiovascular events (cardiovascular death, MI, stroke, urgent coronary revascularization) in patients with a history of MI or with peripheral arterial disease (PAD)
Contraindications
History of stroke, transient ischemic attack (TIA), or intracranial hemorrhage (ICH); active pathological bleeding (eg, ICH, peptic ulcer bleeding)
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to vorapaxar or any ingredient in the formulation; severe hepatic impairment
Dosage and Administration
Dosing: Adult
Note: Vorapaxar 2.08 mg is equivalent to vorapaxar sulfate 2.5 mg.
History of MI or established peripheral arterial disease (PAD): Note: Role in therapy not well established. The overall clinical benefit of adding vorapaxar to other antiplatelet therapy is uncertain; must consider the risk-benefit of bleeding versus reduction in cardiovascular events (ACC/AHA [Gerhard-Herman 2017]; Morrow 2012).
Oral: 2.08 mg once daily in combination with aspirin and/or clopidogrel; there is no experience with use of vorapaxar as monotherapy or with antiplatelet agents other than aspirin and/or clopidogrel.
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer with or without food.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Store in the original package; protect from moisture. Keep the desiccant in the bottle.
Drug Interactions
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Anticoagulants: Vorapaxar may enhance the adverse/toxic effect of Anticoagulants. More specifically, this combination is expected to increase the risk of bleeding. Avoid combination
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Vorapaxar. Avoid combination
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Vorapaxar. Avoid combination
Dasatinib: May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
St John's Wort: May decrease the serum concentration of Vorapaxar. Avoid combination
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Adverse Reactions
>10%:
Hematologic and oncologic: Hemorrhage (any GUSTO [Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Arteries] bleeding [severe, moderate, mild]): 25%), major hemorrhage, life-threatening (13%; clinically significant bleeding, including any bleeding requiring medical attention such as intracranial hemorrhage, or clinically significant overt signs of hemorrhage associated with a drop in hemoglobin of ≥3 g/dL [or when hemoglobin is unavailable, an absolute drop in hematocrit of ≥15% or a fall in hematocrit of 9% to <15%])
1% to 10%:
Central nervous system: Depression (2%)
Dermatologic: Skin rash (2%, includes cutaneous eruptions and exanthemas)
Endocrine & metabolic: Iron deficiency (<2%)
Gastrointestinal: Gastrointestinal hemorrhage (4%)
Hematologic and oncologic: Anemia (5%), major hemorrhage (GUSTO bleeding category “moderate or severe”: 3%; GUSTO bleeding category “severe”: 1%)
Ophthalmic: Retinopathy (<2%)
<1%, postmarketing, and/or case reports: Diplopia (or oculomotor disturbance), hemorrhagic death, intracranial hemorrhage
Warnings/Precautions
Concerns related to adverse effects:
- Bleeding: [US Boxed Warning]: Use is contraindicated in patients with history of stroke, TIA, or ICH; or active pathological bleeding. Discontinue use in patients who experience a stroke, TIA, or ICH during therapy. Vorapaxar increases the risk of bleeding, including ICH and fatal bleeding. The risk of bleeding is proportional to the patient's underlying bleeding risk. General risk factors for bleeding include older age, low body weight, reduced renal or hepatic function, history of bleeding disorders, and concomitant use of medications known to increase the risk of bleeding (eg, anticoagulants, NSAIDS, SSRIs, SNRI); avoid use with anticoagulants. Note: No specific antidote exists for vorapaxar reversal. Significant inhibition of platelet aggregation remains 4 weeks after discontinuation.
Disease-related concerns:
- Hepatic impairment: Due to increased risk of bleeding, use is not recommended in patients with severe hepatic impairment; use with caution in patients with mild or moderate hepatic impairment.
- Renal impairment: Due to increased risk of bleeding, use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
Signs of bleeding; hemoglobin and hematocrit periodically
Pregnancy
Pregnancy Considerations
Due to the potential for serious adverse events (eg, maternal bleeding, hemorrhage) and the long half-life of vorapaxar, alternate agents may be preferred in pregnant women. Discontinue use if pregnancy is detected.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Have patient report immediately to prescriber signs of bleeding (vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding), signs of severe cerebrovascular disease (change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes), severe headache, severe dizziness, passing out, loss of strength and energy, or depression (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for healthcare professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience and judgment in diagnosing, treating and advising patients.