Endometriosis Surgery: What to Expect

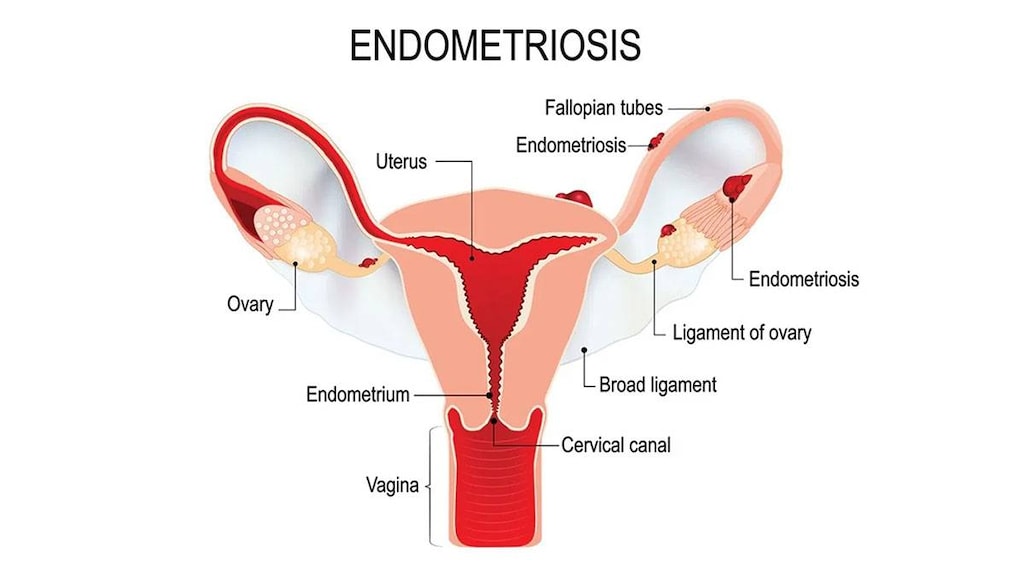
Pelvic pain and cramping, especially around the time of your menstrual cycle, are hallmarks of endometriosis, a condition that occurs when tissue similar to the lining of the uterus (the endometrium) grows outside of your uterus.
When this happens, the tissue from your endometrium may be found in your ovaries, the fallopian tubes that transport an egg from your ovary to your uterus, the tissues holding your uterus in place or on the outer surface of your uterus. Other areas where endometrial implants may be found include your vulva, vagina, cervix, rectum, bladder or bowel.
The affected tissue can swell and bleed, just as the lining inside your uterus does every month when you get your period. With endometriosis, however, this blood has nowhere to go, resulting in inflammation, irritation and scarring. This scar tissue can make it harder for you to get pregnant.
Exactly what causes endometriosis isn’t fully understood, but several theories exist, including a problem with your immune system or endometrial implants attaching to scars from previous surgeries in the affected area, such as from a cesarean delivery.
Endometriosis affects roughly one in 10 women of reproductive age and is most commonly found when women are in their 30s and 40s, according to the American College of Obstetricians and Gynecologists. There is no cure for endometriosis, but for some women, surgery may be a worthwhile option to control the pain and other symptoms.
Endometriosis symptoms
Pelvic pain, especially around the time of menstruation, is the most common symptom of endometriosis. It affects about 75 percent of women who have this condition, according to the U.S National Library of Medicine.
Other symptoms of endometriosis can include:
- Painful menstrual cramps
- Pain during or after sex
- Abdominal pain
- Pain with bowel movements (usually around your period)
- Heavy menstrual flow
- Bleeding between periods
- Pain during urination if endometriosis affects your bladder
- Constipation
- Diarrhea
- Exhaustion
- Lack of energy
- Infertility
Is it endometriosis?
There are many causes of pelvic pain. Endometriosis is just one of them. Your first step toward relief is to get an accurate diagnosis from your doctor.
If you are experiencing pelvic pain, cramps, pain during sex and other symptoms that raise suspicion of endometriosis, your doctor will do a thorough physical and pelvic exam and ask questions about your medical history. You probably also will have imaging tests of your pelvic region.
However, the only way to know with 100 percent accuracy that endometriosis is the source of your symptoms is to undergo a procedure known as a laparoscopy. During this surgical procedure, your doctor inserts a thin tube with a camera and light into a tiny incision to get a better view of the tissue in question and your pelvic organs. This is sometimes followed with a biopsy of the tissue. The results can tell you and your doctor with certainty if you have endometriosis, the U.S. Library of Medicine explains.
Treating endometriosis
The choice of treatment for endometriosis is based on several factors, including how old you are, the severity of your symptoms and your disease, as well as whether you are planning to have children.
The first line of treatment for endometriosis is usually aimed at relieving pain with over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs). Another option, hormonal birth control methods, makes sense only if you are not trying to become pregnant. Extended or continuous cycle contraceptives can reduce or eliminate your monthly periods, relieving bleeding and pain associated with endometriosis. Birth control pills typically contain the hormones estrogen and progestin. Another form of birth control, an implantable, progestin-only IUD, can also relieve pain and reduce bleeding, according to the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
In addition, altered versions of a naturally occurring hormone, known as gonadotropin-releasing hormone, may be prescribed to help control your menstrual flow, which can slow the growth of the endometrial tissue.
Surgery for endometriosis: are you a candidate?
If medications are not effective, surgery can be done to remove endometriosis implants, relieve pain and improve your chances of getting and staying pregnant. That said, your pain may return. As many as 80 percent of women will have pain again within two years of endometriosis surgery, according to the American College of Obstetricians and Gynecologists. The more severe the endometriosis, the more likely it will return. Taking birth control pills or other medications after surgery may help keep pain and symptoms at bay for longer periods of time.
There are several surgical options:
-
Laparoscopy
Conservative endometrial surgery does not remove your uterus or ovaries. Your surgeon will craft a small incision near your navel and insert instruments to remove endometrial tissue via another incision. This is known as the laparoscopic method. The endometrial adhesions can be removed surgically or destroyed using laser energy. Your surgeon may also remove scar tissue during this procedure.
This surgery is usually done on an outpatient basis, but an overnight stay is a possibility, depending on the extent of your disease and the procedure. You will likely be asked to do a bowel prep the night before to clean out your colon, especially if your doctor thinks you have endometriosis on your bowels. The bowel prep regimen varies, but usually includes a liquid diet and medications. Follow your doctor’s specific bowel prep instructions.
You may feel tired in the first few days after surgery. Expect some pain and follow your doctor’s instructions on what you can and can’t do as you recover. Don’t panic if your first period after laparoscopy is more painful, longer or heavier than usual. That is normal.
-
Laparotomy
There are times when endometrial surgery will involve a more extensive traditional abdominal surgery, called a laparotomy. During this procedure, your surgeon will make a much larger incision in your abdomen than with laparoscopy. As such, there is more down time and a longer recovery after this type of endometriosis surgery. Your surgeon may also remove your uterus (hysterectomy) or ovaries (oophorectomy) as part of this procedure, along with as much of the endometriosis that is found outside the uterus. A hysterectomy and oophorectomy for endometriosis is considered a last resort.
This surgery is not without its share of risks and downsides. Having your ovaries removed results in menopause and all of its related symptoms, such as hot flashes, night sweats and thinning, dry skin. Early menopause also increases risk for heart disease, stroke and the brittle bone disease osteoporosis.
What to discuss with your surgeon before your procedure
Regardless of the type of surgery for endometriosis, there are risks to consider, namely infection, bleeding and bruising. These are common and usually not serious. More serious complications may include damage to an organ, severe bleeding or a blood clot in the leg or lungs from not moving around.
Before having any type of surgery, talk to your surgeon about the benefits and possible risks involved.
If you have endometriosis and you are considering surgery, make sure to also ask your doctor the following questions:
- Will the surgery reduce my pain and other endometriosis symptoms?
- What are my options if the symptoms return?
- Will I need to take medication before and after the surgery?
- Will the procedure affect my fertility?
- What will recovery look like?
- Will the surgery be performed through an open incision or via laparoscopy?
- When and under what circumstances would you consider performing a hysterectomy?
Article references
- Office on Women's Health, Endometriosis - https://www.womenshealth.gov/a-z-topics/endometriosis
- Mayo Clinic, Endometriosis Diagnosis and Treatment - https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
- American College of Obstetricians and Gynecologists, Endometriosis - https://www.acog.org/Patients/FAQs/Endometriosis
- U.S. National Library of Medicine, Endometriosis - https://medlineplus.gov/endometriosis.html
- Eunice Kennedy Shriver National Institute of Child Health and Human Development, Treatments for Pain from Endometriosis - https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/treatment#hormone
- Endometriosis Foundation of America, Endometriosis Treatment Support - https://www.endofound.org/endometriosis-treatment-support
- North American Menopause Society, Menopause 101 - https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal
- National Health Service, endometriosis complications - https://www.nhs.uk/conditions/endometriosis/complications/
- Endometriosis UK, Laparoscopic surgery for endometriosis - http://endometriosis-uk.org/sites/default/files/files/Information/laparoscopic_surgery.pdf
- Endometriosis UK, What is a laparoscopy? - https://www.endometriosis-uk.org/your-laparoscopy