A guide to female reproductive hormones

Hormones drive the female reproductive system. They are chemical messengers that regulate puberty, menstruation, fertility, pregnancy, menopause, sex drive and sexuality.
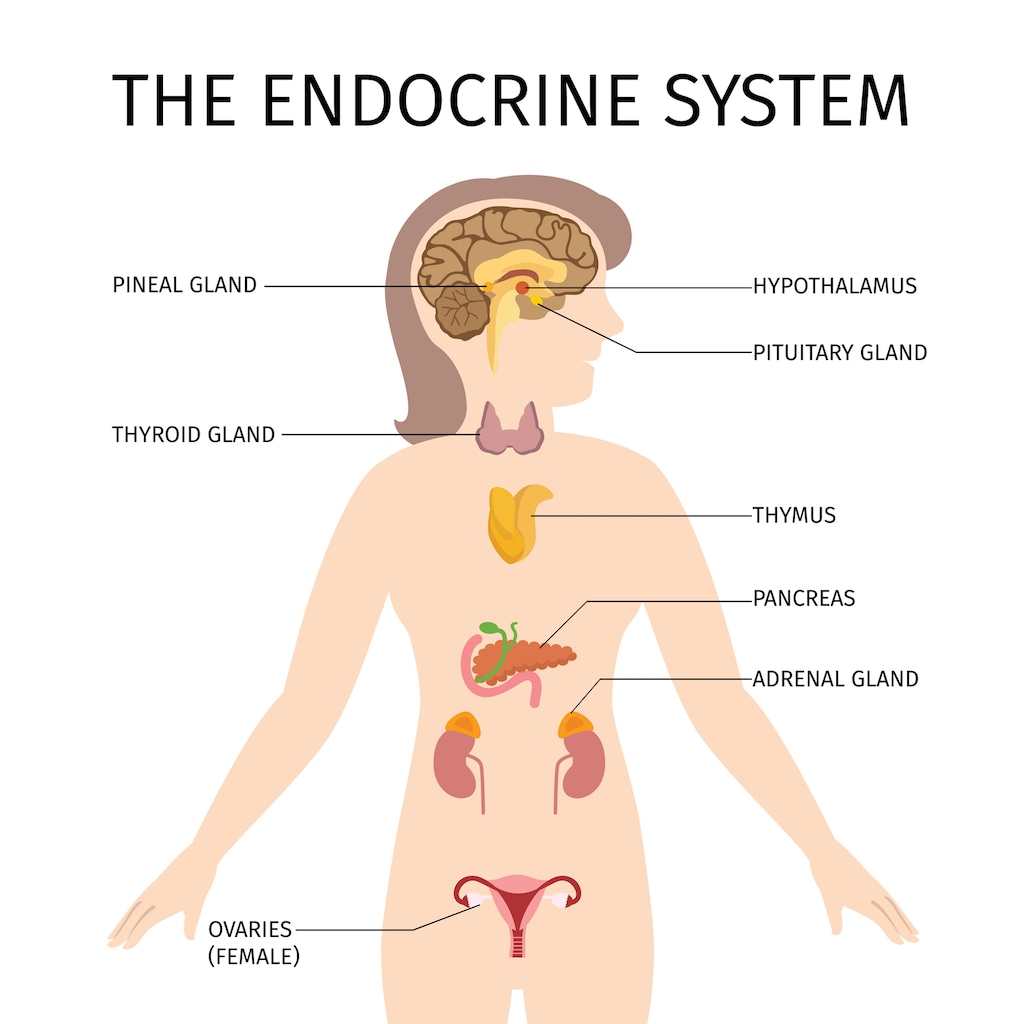
Hormones are a part of your endocrine system, which is sometimes called your ‘hormone system’. Your endocrine system is a network of glands and organs that produce the many hormones your body needs to function.
Here we list the names of key hormones involved in the female reproductive system, describe what they do and where in the body they are made.
Hormones of the female reproductive system
Key hormones of the female reproductive system include:
- Estrogen
- Gonadotropin releasing hormone (GnRH)
- Follicle stimulating hormone (FSH)
- Luteinizing hormone (LH)
- Progesterone
- Testosterone and other androgens
- Prolactin
- Human chorionic gonadotropin (hCG)
Other hormones include:
- Anti Müllerian Hormone (AMH)
- Relaxin
- Oxytocin
What do female reproductive hormones do?
Estrogen
Estrogen is a sex steroid hormone and the main female reproductive hormone. Estrogen comes in three major forms including:
- Estrone (E1) - main form made after menopause
- Estradiol (E2) - main form made during the reproductive years
- Estriol (E3) - main form made during pregnancy
Estrogen is necessary for bringing about the physical changes that occur during puberty. Rising estrogen levels during puberty drive the growth of breasts, pubic and underarm hair, and the start of menstrual cycles.
Through much of your adult life, estrogen also helps to maintain the thickness, elasticity and lubrication of your vaginal walls, which makes sexual intercourse more comfortable.
Estrogen is often described as a pregnancy hormone. In the days leading up to ovulation, estrogen causes your cervical mucus to thin, which makes it easier for sperm to reach an egg and fertilize it. Estrogen also thickens your endometrium - the lining of your uterus - in preparation for pregnancy.
During pregnancy, estrogen promotes the growth of new blood vessels, which helps to nourish the fetus. It’s also involved in the development of milk ducts in the breasts.
In the years leading up to your menstrual cycle stopping - a time known as perimenopause - your estrogen levels start to drop. A year after your last menstrual cycle, which is when menopause officially begins, your main or primary source of estrogen becomes estrone, which is less potent than the estradiol made during your reproductive years.
In addition to its roles in the female reproductive system, estrogen also affects cholesterol levels, bones, muscles, blood sugar levels, blood flow, skin and brain function.
Gonadotropin releasing hormone
During adolescence, rising levels of GnRH trigger the start of puberty or sexual maturation. GnRH also plays a very important role during your reproductive years, regulating the release of the gonadotropic hormones FSH and LH. These hormones promote ovulation and stimulate secretion of the sex hormones estrogen and progesterone from the ovaries.
Follicle stimulating hormone
FSH is a gonadotropic hormone which is essential for driving the changes that occur at puberty and controlling the function of ovaries.
FSH stimulates small fluid-filled sacs in the ovaries called follicles to grow each cycle. As the follicles grow they secrete estrogen. One of the follicles will mature each cycle and eventually burst open releasing an egg (oocyte) at ovulation.
Luteinizing hormone
LH is a gonadotropic hormone that also regulates the function of the ovaries. In the first half of the menstrual cycle it stimulates ovarian follicles to produce estrogen. A surge of LH in the middle of your cycle then causes ovulation, the process where a follicle tears open releasing a mature egg from the ovary. In the second half of the menstrual cycle, LH stimulates the remains of the torn follicle - the corpus luteum - to produce the hormone progesterone.
Progesterone
Progesterone is a sex steroid hormone that performs a number of roles. It is initially produced by the remains of the torn follicle from which the egg erupted at ovulation, which is called the corpus luteum. And its first task is to prepare your body for pregnancy.
If the egg is fertilized, progesterone stimulates the growth of blood vessels in the endometrium and glands to secrete nutrients to sustain an embryo. It prepares the lining of the uterus for implantation of the embryo and helps establish the placenta. The placenta supplies the growing baby with oxygen and nutrients, and it also takes over the role of supplying progesterone, which helps maintain the endometrium for the duration of the pregnancy.
If an egg is not fertilized after ovulation, the corpus luteum will stop producing progesterone and levels of the hormone will fall.
Progesterone also stimulates the growth of breast tissue in pregnant people, prevents lactation during pregnancy and helps to strengthen the muscles of the pelvic wall in the lead up to labor. Progesterone levels rise during pregnancy until the baby is born.
Testosterone and other androgens
Testosterone is one of several androgens or male sex steroid hormones, which is also found in females, albeit in much smaller amounts than in males. Other androgens include androstenedione, dihydrotestosterone (DHT), dehydroepiandrosterone (DHEA) and dehydroepiandrosterone-sulfate (DHEA-S).
While testosterone and other androgens perform various roles in females, they are mostly converted by the enzyme aromatase into estrogen.
In addition to providing a source of estrogen, androgens play a role in determining when puberty begins and also stimulate the growth of pubic and body hair. They are also thought to help regulate the function of the kidneys and liver.
In both males and females, testosterone strengthens muscles and bones during and after puberty, increases sex drive and tells the body when to produce new blood cells. It also regulates the secretion of LH and FSH and is important for ovarian function. It may also play a role in brain function, affecting mood and cognitive function.
Prolactin
Prolactin (lactotropin) is a hormone that stimulates the development of mammary glands within breast tissue in pregnant people.
Prolactin also stimulates milk production, including the production of lactose, casein and lipids which make up breastmilk.
Levels of this hormone are usually high in those who are pregnant or breastfeeding. About one to two weeks after stopping breastfeeding, prolactin levels will have returned to levels seen in non-pregnant people.
Human chorionic gonadotropin
hCG is a hormone produced by the placenta. It stops your menstrual cycle and thickens the lining of your uterus to support the growing embryo. It stimulates the body to produce more estrogen and progesterone.
hCG is the hormone that pregnancy tests measure to help confirm a pregnancy. It can be detected in blood and urine about 10 to 11 days after conception occurs, which is when an egg is fertilized by a sperm. Levels of the hormone continue to rise, doubling about every 3 days, until about week 10 of pregnancy. After this levels of hCG start to decline.
Anti-Müllerian hormone
AMH is a protein hormone produced by ovarian follicles. Measuring the amount of AMH in your bloodstream can be useful to help assess your ovarian reserves, or how many follicles you have left, if you’re concerned about your reproductive age. AMH may also play a role in regulating the production of steroid sex hormones in the ovaries.
The embryonic testes of a male fetus also produce AMH, which causes Müllerian ducts earmarked to develop into a female reproductive tract to disappear. The male fetus is then left with only Wollfian ducts, which develop into a male reproductive tract in the presence of testosterone.
In the female fetus the Wollifian ducts disappear because of a lack of testosterone and the Müllerian ducts develop into the fallopian tubes, uterus, cervix and upper area of the vagina in the absence of AMH.
Relaxin
Relaxin is a protein hormone that is known for relaxing ligaments in the pelvis and softening and widening the cervix in preparation for childbirth. It also promotes the rupture of the membranes surrounding the baby.
Circulating levels of the hormone rise after ovulation, relaxing the walls of the uterus and preparing the lining of the uterus for pregnancy. Levels drop again if pregnancy does not occur.
Levels of relaxin are at their highest during the first trimester of pregnancy. It’s thought that during this time, relaxin encourages the implantation of the embryo in the uterus and growth of the placenta. It also helps to stop the uterus from contracting in early pregnancy.
Relaxin also helps to relax blood vessels, which increases the flow of blood to the placenta and kidneys, helping to meet the extra demands put on the body by the growing fetus. Its ability to relax blood vessels can also cause changes in blood pressure.
It is thought that the release of relaxin may be stimulated by LH from the pituitary gland during the menstrual cycle and by hCG from the placenta during pregnancy.
Relaxin also reduces the formation of hard tissue known as fibrosis in the kidneys, heart and liver that can occur in response to inflammation. It’s also thought to aid wound healing and have anti-inflammatory properties.
Oxytocin
Oxytocin is a peptide hormone that signals the muscles of the uterus to contract during childbirth and lactation. It also increases the production of prostaglandins, which aids contractions.
Oxytocin also encourages milk flow through the ducts in the breasts during breastfeeding. In addition to this, it works in the brain, playing a role in behavior.
Where are female reproductive hormones made?
- Estrogen. Estrogen is mainly made by the ovaries during your reproductive years. Some estrogen is also made by your adrenal glands, body fat, and by your placenta during pregnancy.
- Gonadotropin releasing hormone (GnRH). GnRH is produced and secreted by the hypothalamus. It then travels to the pituitary gland below where it stimulates the production of FSH and LH.
- Follicle stimulating hormone (FSH). FSH is made in the anterior pituitary gland.
- Luteinizing hormone (LH). LH is made in the anterior pituitary gland.
- Progesterone. Progesterone is mainly made in the ovaries by the corpus luteum, until the placenta takes over its production during pregnancy. The ovaries and adrenal glands also produce small amounts of progesterone.
- Testosterone. Testosterone is produced by the ovaries and also the adrenal glands, fat cells and skin.
- Prolactin. Prolactin is mainly made and released by your pituitary gland. Nipple stimulation, exercise and stress can also cause your central nervous system, immune system, uterus and mammary glands to produce prolactin.
- Human chorionic gonadotropin (hCG). hCG is produced by the placenta.
- Anti Müllerian Hormone (AMH). AMH is produced in the ovaries by ovarian follicles. It’s also produced by the embryonic testes in a growing male fetus.
- Relaxin. Relaxin is primarily produced by the corpus luteum. It’s also produced by the placenta and uterus.
- Oxytocin. Oxytocin is made by the hypothalamus and secreted by the posterior pituitary gland.
Location of the glands and organs that produce the hormones listed above
| Gland or organ | Location |
| Adrenal glands | One on top of each kidney |
| Body fat (adipose tissue) | Found under the skin, around organs, muscles, in bone marrow and breast tissue. |
| Central nervous system | Brain and spinal cord |
| Corpus luteum | Inside the ovaries |
| Hypothalamus | Base of your brain near where your optic nerves meet |
| Immune system | Made up of organs, cells and chemicals throughout the body |
| Mammary glands | In the breasts |
| Ovaries | Either side of the uterus, near the fallopian tubes |
| Pituitary gland | Below the brain |
| Placenta | In the uterus during pregnancy |
| Uterus (womb) | In the pelvis, below the ovaries and between the bladder and the rectum |
What regulates the female reproductive system?
The female reproductive system is regulated by the interaction of hormones with the hypothalamus, pituitary gland and ovaries, which form the hypothalamic-pituitary-gonadal axis.
The hypothalamus releases GnRH in pulses, which stimulates the production and release of FSH and LH from the anterior pituitary. These hormones promote ovulation. They also stimulate the ovaries to secrete estrogen and progesterone,
Rising and falling levels of estrogen, progesterone and inhibin, which is also produced by the ovaries, lead to changes in the amount of GnRH, FSH and LH produced.
For example, if an egg is not fertilized, levels of estrogen and progesterone fall signaling the hypothalamus to secrete more GnRH and start the next menstrual cycle. However, if pregnancy does occur, higher levels of progesterone inhibit FSH and LH, preventing the development of new follicles and eggs and another pregnancy.
Article references
- Endocrine Society. Reproductive Hormones. January 23, 2022. Available at: https://www.endocrine.org/patient-engagement/endocrine-library/hormones-and-endocrine-function/reproductive-hormones. [Accessed July 18, 2022].
- You and your Hormones, an Education Resource from the Society for Endocrinology. Hormones. Available at: https://www.yourhormones.info/hormones. [Accessed July 18, 2022].
- Cleveland Clinic. Estrogen. February 8, 2022. Available at: https://my.clevelandclinic.org/health/body/22353-estrogen. [Accessed July 18, 2022].
- Cleveland Clinic. Prolactin. February 15, 2022. Available at: https://my.clevelandclinic.org/health/articles/22429-prolactin. [Accessed July 18, 2022].
- Harvard Health. Testosterone - What It Does And Doesn’t Do. August 29, 2019. Available at: https://www.health.harvard.edu/medications/testosterone--what-it-does-and-doesnt-do. [Accessed July 18, 2022].
- Cleveland Clinic. Human Chorionic Gonadotropin. March 11, 2022. Available at: https://my.clevelandclinic.org/health/articles/22489-human-chorionic-gonadotropin. [Accessed July 18, 2022].
- Klein CE. The Hypothalamic-Pituitary-Gonadal Axis. In: Kufe DW, Pollock RE, Weichselbaum RR, et al., editors. Holland-Frei Cancer Medicine. 6th edition. Hamilton (ON): BC Decker; 2003. Available from: https://www.ncbi.nlm.nih.gov/books/NBK13386/.
- MSD Manual Professional Version. Female Reproductive Endocrinology. April 2022. Available at: https://www.msdmanuals.com/en-nz/professional/gynecology-and-obstetrics/female-reproductive-endocrinology/female-reproductive-endocrinology. [Accessed July 18, 2022].



