Multiple Sclerosis Relapse: 7 Triggers to Avoid

Multiple sclerosis (MS) is a lifelong disease of the central nervous system, which includes your brain and spinal cord. Most people with MS (85 percent) have relapsing-remitting MS, a type in which symptoms come and go. When symptoms return, it's called a relapse. An MS relapse can also be called a flare, an attack or an exacerbation.
What is a relapse?
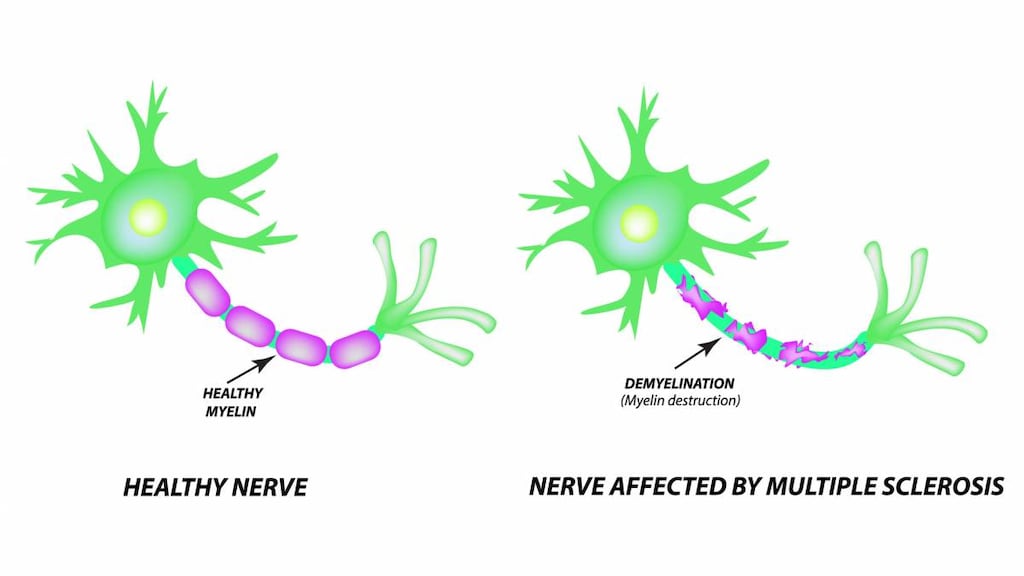
A relapse happens when your immune system attacks the protective insulation around the nerves of your brain or spinal cord (myelin). This causes inflammation that stops or interferes with nerve signals, leading to symptoms of a relapse.
To be considered a true relapse, you must have new MS symptoms or old symptoms that get worse and last for at least 24 hours. There also needs to be at least 30 days between symptoms for relapses to be considered separate attacks, and there can't be another possible cause of the symptoms such as infection or overheating. Common MS symptoms (like fatigue, confusion, tingling, or numbness) that get worse generally are not considered a relapse.
A relapse usually starts over hours or days and can last for weeks or months. Mild relapses may not need to be treated. If you have a relapse that interferes with your ability to do your usual daily activities, your doctor may recommend a short course of steroids in addition to your other MS medications.
Relapses can happen without warning, but they're often triggered by something. Relapse triggers may be different for each person. You may even have different triggers with each relapse. Along with taking disease-modifying medications for MS, avoiding triggers is the best way to prevent an MS relapse.
7 relapse triggers to avoid
The most common triggers of MS relapses are:
- Infection. Infections trigger a third of all relapses. Urinary tract infections as well as cold or flu viruses are common causes. To prevent a urinary tract infection, drink plenty of fluid. Also, get an annual flu shot and avoid sick people and crowds during cold and flu season. Wash your hands often.
- Increased body temperature. This could be from a fever. It could also be from hot weather or soaking in a sauna or hot tub. Some people with MS benefit from wearing a water-cooled vest during hot weather.
- Smoking. Evidence continues to mount that smoking is a major MS trigger. If you have trouble quitting, ask your doctor for help.
- Stress. Minor stress is unavoidable, but severe, chronic stress can be a trigger for many people with MS. Try ways to manage stress, such as yoga or meditation. For severe stress, consider seeing a mental health counselor.
- Fatigue. MS fatigue is one of the most common symptoms, and getting overtired is a very common trigger. Make sure you get enough sleep. Exercising regularly is a good way to manage stress and help you sleep better at night. Know your limits and avoid overdoing activities.
- Medications. Some specific medications used to treat Crohn’s disease and rheumatoid arthritis have been linked to MS relapses. It's also possible that medication interactions can cause a relapse. Ask your doctor to review your medication list to avoid this trigger.
- Stopping your disease-modifying medications. Some people with MS make the mistake of stopping their disease-modifying medication on their own because they feel fine or don’t think it's helping. Research shows that taking these medications may prevent MS damage, both when you feel fine and when you don’t. Never make any medication decisions without talking to your MS doctor.
- Hormonal changes. Sometimes the hormonal changes related to pregnancy can trigger a relapse. Pregnancy actually seems to stop disease activity for a while, but the stress of delivery or the hormonal changes after having a baby may increase the risk for a relapse for six months after giving birth.
The bottom line
You may not be able to prevent an MS relapse, but you can reduce your risk by working with your doctor to find the best MS treatment for you and avoiding triggers as much as possible.
To that end:
- Take precautions to avoid common triggers, like catching infections or getting too hot.
- Make sure you get enough rest and find some ways to reduce stress.
- Don’t even think about smoking.
Also, be sure to let your doctor know if you have new MS symptoms or if your existing symptoms get worse for longer than 24 hours.
Article references
- MS Society, Relapsing remitting MS https://www.mssociety.org.uk/about-ms/types-of-ms/relapsing-remitting-ms
- National Multiple Sclerosis Society, Managing Relapses https://www.nationalmssociety.org/Treating-MS/Managing-Relapses
- Cleveland Clinic, Avoid 8 Common Triggers to Make Your Life With MS Easier https://health.clevelandclinic.org/avoid-8-common-triggers-to-make-your-life-with-ms-easier/