Bacterial vaginosis is a type of vaginal inflammation caused by the overgrowth of bacteria naturally found in the vagina, which upsets the natural balance.
Women in their reproductive years are most likely to get bacterial vaginosis, but it can affect women of any age. The cause isn't completely understood, but certain activities, such as unprotected sex or frequent douching, increase your risk.
Symptoms
Bacterial vaginosis signs and symptoms may include:
- Thin, gray, white or green vaginal discharge
- Foul-smelling "fishy" vaginal odor
- Vaginal itching
- Burning during urination
Many women with bacterial vaginosis have no signs or symptoms.
When to see a doctor
Make an appointment to see your doctor if:
- You have vaginal discharge that's new and associated with an odor or fever. Your doctor can help determine the cause and identify signs and symptoms.
- You've had vaginal infections before, but the color and consistency of your discharge seems different this time.
- You have multiple sex partners or a recent new partner. Sometimes, the signs and symptoms of a sexually transmitted infection are similar to those of bacterial vaginosis.
- You try self-treatment for a yeast infection with an over-the-counter treatment and your symptoms persist.
Causes
Bacterial vaginosis results from overgrowth of one of several bacteria naturally found in your vagina. Usually, "good" bacteria (lactobacilli) outnumber "bad" bacteria (anaerobes). But if there are too many anaerobic bacteria, they upset the natural balance of microorganisms in your vagina and cause bacterial vaginosis.
Risk factors
Risk factors for bacterial vaginosis include:
- Having multiple sex partners or a new sex partner. Doctors don't fully understand the link between sexual activity and bacterial vaginosis, but the condition occurs more often in women who have multiple sex partners or a new sex partner. Bacterial vaginosis also occurs more frequently in women who have sex with women.
- Douching. The practice of rinsing out your vagina with water or a cleansing agent (douching) upsets the natural balance of your vagina. This can lead to an overgrowth of anaerobic bacteria, and cause bacterial vaginosis. Since the vagina is self-cleaning, douching isn't necessary.
- Natural lack of lactobacilli bacteria. If your natural vaginal environment doesn't produce enough of the good lactobacilli bacteria, you're more likely to develop bacterial vaginosis.
Complications
Bacterial vaginosis doesn't generally cause complications. Sometimes, having bacterial vaginosis may lead to:
- Preterm birth. In pregnant women, bacterial vaginosis is linked to premature deliveries and low birth weight babies.
- Sexually transmitted infections. Having bacterial vaginosis makes women more susceptible to sexually transmitted infections, such as HIV, herpes simplex virus, chlamydia or gonorrhea. If you have HIV, bacterial vaginosis increases the odds that you'll pass the virus on to your partner.
- Infection risk after gynecologic surgery. Having bacterial vaginosis may increase the risk of developing a post-surgical infection after procedures such as hysterectomy or dilation and curettage (D&C).
- Pelvic inflammatory disease (PID). Bacterial vaginosis can sometimes cause PID, an infection of the uterus and the fallopian tubes that can increase the risk of infertility.
Prevention
To help prevent bacterial vaginosis:
- Minimize vaginal irritation. Use mild, nondeodorant soaps and unscented tampons or pads.
- Don't douche. Your vagina doesn't require cleansing other than normal bathing. Frequent douching disrupts the vaginal balance and may increase your risk of vaginal infection. Douching won't clear up a vaginal infection.
- Avoid a sexually transmitted infection. Use a male latex condom, limit your number of sex partners or abstain from intercourse to minimize your risk of a sexually transmitted infection.
Diagnosis
To diagnose bacterial vaginosis, your doctor may:
- Ask questions about your medical history. Your doctor may ask about any previous vaginal infections or sexually transmitted infections.
- Perform a pelvic exam. During a pelvic exam, your doctor visually examines your vagina for signs of infection, and inserts two fingers into your vagina while pressing on your abdomen with the other hand to check your pelvic organs for signs that may indicate disease.
- Take a sample of vaginal secretions. This may be done to check for an overgrowth of anaerobic bacteria in your vaginal flora. Your doctor may examine the vaginal secretions under a microscope, looking for "clue cells," vaginal cells covered with bacteria that are a sign of bacterial vaginosis.
- Test your vaginal pH. Your doctor may check the acidity of your vagina by placing a pH test strip in your vagina. A vaginal pH of 4.5 or higher is a sign of bacterial vaginosis.
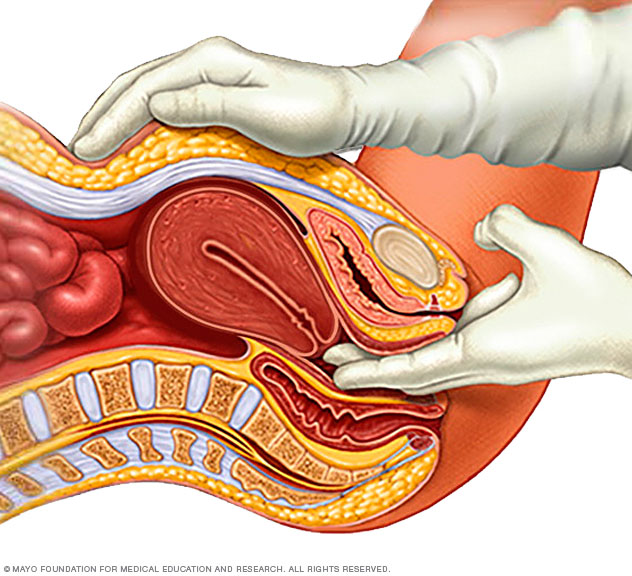
During a pelvic exam, your doctor inserts two gloved fingers inside your vagina. While simultaneously pressing down on your abdomen, he or she can evaluate your uterus, ovaries and other pelvic organs.
Treatment
To treat bacterial vaginosis, your doctor may prescribe one of the following medications:
- Metronidazole (Flagyl, Metrogel-Vaginal, others). This medicine may be taken as a pill by mouth (orally). Metronidazole is also available as a topical gel that you insert into your vagina. To reduce the risk of stomach upset, abdominal pain or nausea while using this medication, avoid alcohol during treatment and for at least one day after completing treatment — check the instructions on the product.
- Clindamycin (Cleocin, Clindesse, others). This medicine is available as a cream that you insert into your vagina. Clindamycin cream may weaken latex condoms during treatment and for at least three days after you stop using the cream.
- Tinidazole (Tindamax). This medication is taken orally. Tinidazole has the same potential for stomach upset and nausea as oral metronidazole does, so avoid alcohol during treatment and for at least three days after completing treatment.
- Secnidazole (Solosec). This is an antibiotic you take orally in one dose. The medication comes as a packet of granules that you sprinkle onto a soft food, such as applesauce, pudding or yogurt. You eat the mixture within 30 minutes, being careful not to crunch or chew the granules.
It's generally not necessary to treat an infected woman's male sexual partner, but bacterial vaginosis can spread between female sexual partners. Female partners should seek testing and may need treatment. It's especially important for pregnant women with symptoms to be treated to help decrease the risk of premature delivery or low birth weight.
Take your medicine or use the cream or gel for as long as your doctor prescribes it — even if your symptoms go away. Stopping treatment early may increase the risk of recurrence.
Recurrence
It's common for bacterial vaginosis to recur within three to 12 months, despite treatment. Researchers are exploring treatments for recurrent bacterial vaginosis. If your symptoms recur soon after treatment, talk with your doctor about treatments. One option may be extended-use metronidazole therapy.
A self-help approach is lactobacillus colonization therapy — which attempts to boost the number of good bacteria in your vagina and re-establish a balanced vaginal environment — possibly accomplished by eating certain types of yogurt or other foods containing lactobacilli. While current research shows there may be some benefit to probiotic therapy, more research is needed on the subject.
Preparing for an appointment
Try to schedule your appointment on a day when you don't have your period. That way, your primary care doctor or gynecologist can observe and evaluate your vaginal discharge without menstrual discharge getting in the way. Avoid using tampons and vaginal deodorant sprays, and don't douche or have sex for 24 hours before your appointment.
What you can do
To make the best use of your time with your doctor and prevent you from forgetting an important question:
- Make a list of any symptoms you're experiencing. Include all of your symptoms, even if you don't think they're related.
- Make a list of any medications, vitamins, herbs or other supplements you take. Include how often you take them and the doses.
- Take a notepad or electronic device with you. Take notes of important information during your visit.
- Prepare a list of questions to ask your doctor. List your most important questions first, in case time runs out.
For bacterial vaginosis, some basic questions to ask your doctor include:
- Can I do anything to prevent bacterial vaginosis?
- What signs and symptoms should I look for?
- Do I need to take medicine?
- Does my partner also need to be tested or treated?
- Are there any special instructions for taking the medicine?
- Are there any over-the-counter products that will treat my condition?
- What can I do if my symptoms return after treatment?
Don't hesitate to ask questions during your appointment if you don't understand something.
Questions your doctor may ask
Be prepared to answer questions your doctor may have, such as:
- What symptoms are you experiencing?
- How long have you had your symptoms?
- Do you notice a strong vaginal odor?
- Have you ever been treated for a vaginal infection?
- Have you tried any over-the-counter products to treat your condition?
- Have you recently taken antibiotics for any reason?
- Are you sexually active?
- Are you pregnant?
- Do you use scented soap or bubble bath?
- Do you douche or use feminine hygiene spray?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.