Seeing blood in your urine can be alarming. While in many instances the cause is harmless, blood in urine (hematuria) can indicate a serious disorder.
Blood that you can see is called gross hematuria. Urinary blood that's visible only under a microscope (microscopic hematuria) is found when your doctor tests your urine. Either way, it's important to determine the reason for the bleeding.
Treatment depends on the cause.
Symptoms
Gross hematuria produces pink, red or cola-colored urine due to the presence of red blood cells. It takes little blood to produce red urine, and the bleeding usually isn't painful. Passing blood clots in your urine, however, can be painful.
Bloody urine often occurs without other signs or symptoms.
When to see a doctor
Make an appointment to see your doctor anytime you notice blood in your urine.
Some medications, such as the laxative Ex-lax, and certain foods, including beets, rhubarb and berries, can cause your urine to turn red. A change in urine color caused by drugs, food or exercise might go away within a few days.
Bloody urine looks different, but you might not be able to tell the difference. It's best to see your doctor anytime you see red-colored urine.
Causes
In hematuria, your kidneys — or other parts of your urinary tract — allow blood cells to leak into urine. Various problems can cause this leakage, including:
-
Urinary tract infections. These occur when bacteria enter your body through the urethra and multiply in your bladder. Symptoms can include a persistent urge to urinate, pain and burning with urination, and extremely strong-smelling urine.
For some people, especially older adults, the only sign of illness might be microscopic blood in the urine.
- Kidney infections (pyelonephritis). These can occur when bacteria enter your kidneys from your bloodstream or move from your ureters to your kidney(s). Signs and symptoms are often similar to bladder infections, though kidney infections are more likely to cause a fever and flank pain.
-
A bladder or kidney stone. The minerals in concentrated urine sometimes form crystals on the walls of your kidneys or bladder. Over time, the crystals can become small, hard stones.
The stones are generally painless, so you probably won't know you have them unless they cause a blockage or are being passed. Then there's usually no mistaking the symptoms — kidney stones, especially, can cause excruciating pain. Bladder or kidney stones can also cause both gross and microscopic bleeding.
- Enlarged prostate. The prostate gland — which is just below the bladder and surrounding the top part of the urethra — often enlarges as men approach middle age. It then compresses the urethra, partially blocking urine flow. Signs and symptoms of an enlarged prostate (benign prostatic hyperplasia, or BPH) include difficulty urinating, an urgent or persistent need to urinate, and either visible or microscopic blood in the urine. Infection of the prostate (prostatitis) can cause the same signs and symptoms.
- Kidney disease. Microscopic urinary bleeding is a common symptom of glomerulonephritis, an inflammation of the kidneys' filtering system. Glomerulonephritis may be part of a systemic disease, such as diabetes, or it can occur on its own. Viral or strep infections, blood vessel diseases (vasculitis), and immune problems such as IgA nephropathy, which affects the small capillaries that filter blood in the kidneys (glomeruli), can trigger glomerulonephritis.
- Cancer. Visible urinary bleeding may be a sign of advanced kidney, bladder or prostate cancer. Unfortunately, you might not have signs or symptoms in the early stages, when these cancers are more treatable.
- Inherited disorders. Sickle cell anemia — a hereditary defect of hemoglobin in red blood cells — causes blood in urine, both visible and microscopic hematuria. So can Alport syndrome, which affects the filtering membranes in the glomeruli of the kidneys.
- Kidney injury. A blow or other injury to your kidneys from an accident or contact sports can cause visible blood in your urine.
- Medications. The anti-cancer drug cyclophosphamide and penicillin can cause urinary bleeding. Visible urinary blood sometimes occurs if you take an anticoagulant, such as aspirin and the blood thinner heparin, and you also have a condition that causes your bladder to bleed.
-
Strenuous exercise. It's rare for strenuous exercise to lead to gross hematuria, and the cause is unknown. It may be linked to trauma to the bladder, dehydration or the breakdown of red blood cells that occurs with sustained aerobic exercise.
Runners are most often affected, although anyone can develop visible urinary bleeding after an intense workout. If you see blood in your urine after exercise, don't assume it's from exercising. See your doctor.
Often the cause of hematuria can't be identified.

Your urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys are located toward the back of the upper abdomen. They filter waste and fluid from the blood and produce urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through another small tube called the urethra.

Your urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys are located toward the back of the upper abdomen. They filter waste and fluid from the blood and produce urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through another small tube called the urethra.
Risk factors
Almost anyone — including children and teens — can have red blood cells in the urine. Factors that make this more likely include:
- Age. Many men older than 50 have occasional hematuria due to an enlarged prostate gland.
- A recent infection. Kidney inflammation after a viral or bacterial infection (post-infectious glomerulonephritis) is one of the leading causes of visible urinary blood in children.
- Family history. You might be more prone to urinary bleeding if you have a family history of kidney disease or kidney stones.
- Certain medications. Aspirin, nonsteroidal anti-inflammatory pain relievers and antibiotics such as penicillin are known to increase the risk of urinary bleeding.
- Strenuous exercise. Long-distance runners are especially prone to exercise-induced urinary bleeding. In fact, the condition is sometimes called jogger's hematuria. But anyone who works out strenuously can develop symptoms.
Diagnosis
The following tests and exams play a key role in finding a cause for blood in your urine:
- Physical exam, which includes a discussion of your medical history.
- Urine tests. Even if your bleeding was discovered through urine testing (urinalysis), you're likely to have another test to see if your urine still contains red blood cells. A urinalysis can also check for a urinary tract infection or the presence of minerals that cause kidney stones.
- Imaging tests. Often, an imaging test is required to find the cause of hematuria. Your doctor might recommend a CT or MRI scan or an ultrasound exam.
- Cystoscopy. Your doctor threads a narrow tube fitted with a tiny camera into your bladder to examine the bladder and urethra for signs of disease.
Sometimes, the cause of urinary bleeding can't be found. In that case, your doctor might recommend regular follow-up tests, especially if you have risk factors for bladder cancer, such as smoking, exposure to environmental toxins or a history of radiation therapy.
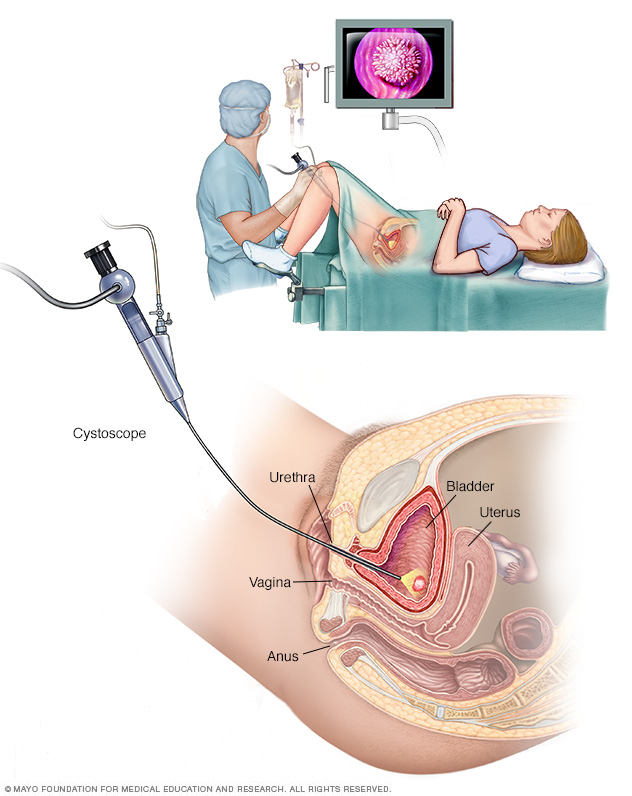
Cystoscopy allows your doctor to view your lower urinary tract to look for abnormalities, such as a bladder stone. Surgical tools can be passed through the cystoscope to treat certain urinary tract conditions.
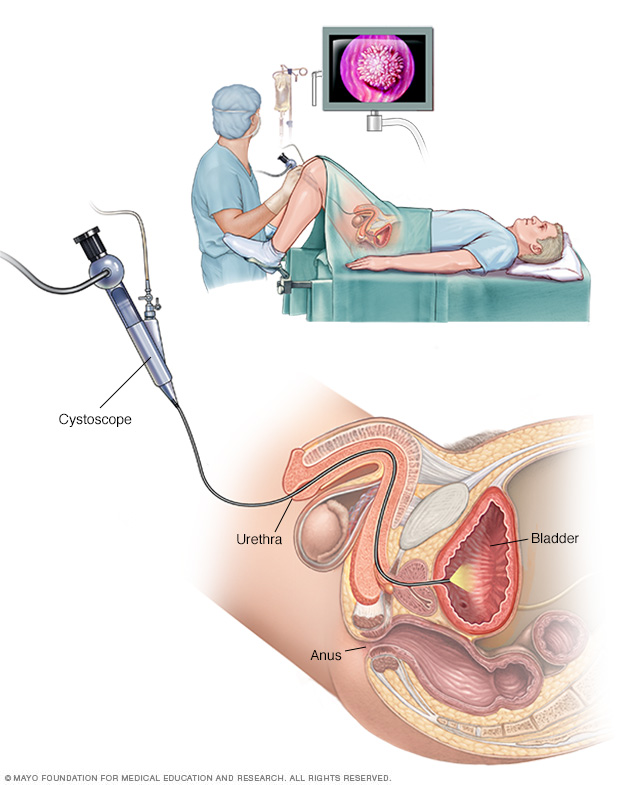
Cystoscopy allows your doctor to view your lower urinary tract to look for abnormalities in your urethra and bladder. Surgical tools can be passed through the cystoscope to treat certain urinary tract conditions.
Treatment
Depending on the condition causing your hematuria, treatment might involve taking antibiotics to clear a urinary tract infection, trying a prescription medication to shrink an enlarged prostate or having shock wave therapy to break up bladder or kidney stones. In some cases, no treatment is necessary.
Be sure to follow up with your doctor after treatment to ensure there's no more blood in your urine.
Preparing for an appointment
You're likely to start by seeing your family doctor or primary care provider. Or you might be referred to a doctor who specializes in urinary tract disorders (urologist).
Here's some information to help you prepare for your appointment.
What you can do
Make a list of:
- Your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment, and when they began
- Key medical information, including other conditions for which you're being treated, and whether bladder or kidney diseases run in your family
- All medications, vitamins or other supplements you take, including doses
- Questions to ask your doctor
For hematuria, some questions to ask include:
- What are the possible causes of my symptoms?
- What tests do I need?
- Is my condition likely temporary?
- What treatments are available?
- I have other health issues. How can I best manage them together?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you questions, such as:
- Do you have pain when you urinate?
- Do you see blood in your urine only sometimes or all the time?
- When do you see blood in your urine — when you start urinating, toward the end of your urine stream or the entire time you're urinating?
- Are you also passing blood clots during urination? What size and shape are they?
- Do you smoke?
- Are you exposed to chemicals on the job? What kinds?
- Have you had radiation therapy?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.