Chronic exertional compartment syndrome is an exercise-induced muscle and nerve condition that causes pain, swelling and sometimes disability in the affected muscles of the legs or arms. Anyone can develop the condition, but it's more common in young adult runners and athletes who participate in activities that involve repetitive impact.
Chronic exertional compartment syndrome may respond to nonsurgical treatment and activity modification. If nonsurgical treatment doesn't help, your doctor might recommend surgery. Surgery is successful for many people and might allow you to return to your sport.
Symptoms
Your limbs have specific areas of muscle (compartments). Your lower leg, for example, has four compartments. Chronic exertional compartment syndrome often occurs in the same compartment of an affected limb on both sides of the body, usually the lower leg.
Signs and symptoms can include:
- Aching, burning or cramping pain in a compartment of the affected limb
- Tightness in the affected limb
- Numbness or tingling in the affected limb
- Weakness of the affected limb
- Foot drop, in severe cases, if legs are affected
- Occasionally, swelling or bulging as a result of a muscle hernia
Pain caused by chronic exertional compartment syndrome typically follows this pattern:
- Begins consistently after a certain time, distance or intensity of exertion after you start exercising the affected limb
- Progressively worsens as you exercise
- Becomes less intense or stops completely within 15 minutes of stopping the activity
- Over time, recovery time after exercise may increase
Taking a complete break from exercise or performing only low-impact activity might relieve your symptoms, but relief is usually only temporary. Once you take up running again, for instance, those familiar symptoms usually come back.
When to see a doctor
If you have recurring unusual pain, swelling, weakness, loss of sensation or soreness while exercising or participating in sports activities, talk to your doctor.
Sometimes chronic exertional compartment syndrome is mistaken for shin splints, a more common cause of leg pain in young people who do a lot of vigorous weight-bearing activity, such as running. If you think you have shin splints and the pain doesn't get better with self-care, talk to your doctor.
Causes
The cause of chronic exertional compartment syndrome isn't completely understood. When you exercise, your muscles expand in volume. If you have chronic exertional compartment syndrome, the tissue that encases the affected muscle (fascia) doesn't expand with the muscle, causing pressure and pain in a compartment of the affected limb.
Some experts suggest that how you move while exercising might have a role in causing chronic exertional compartment syndrome. Other causes might include having muscles that enlarge excessively during exercise, having an especially inflexible fascia surrounding the affected muscle compartment or having high pressure within your veins.
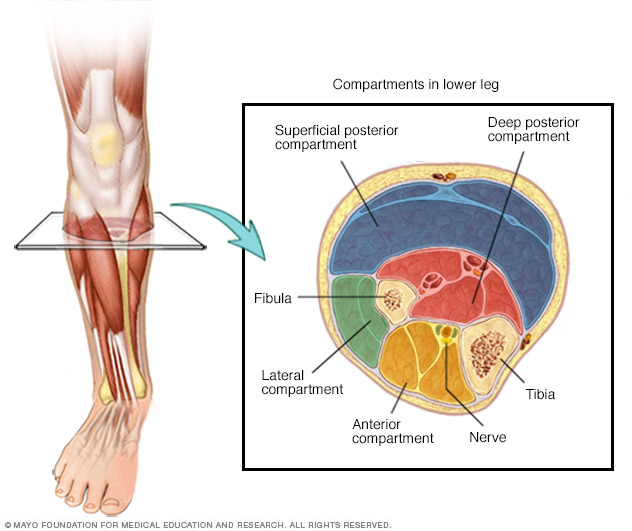
Chronic exertional compartment syndrome is a musculoskeletal condition brought on by exercise. It can affect muscle compartments in any of your limbs but occurs most commonly in the lower legs. The lower leg has four compartments, and any one or all of them can be affected.
Risk factors
Certain factors increase your risk of developing chronic exertional compartment syndrome, including:
- Age. Although people of any age can develop chronic exertional compartment syndrome, the condition is most common in male and female athletes under age 30.
- Type of exercise. Repetitive impact activity — such as running — increases your risk of developing the condition.
- Overtraining. Working out too intensely or too frequently also can raise your risk of chronic exertional compartment syndrome.
Complications
Chronic exertional compartment syndrome isn't a life-threatening condition and usually doesn't cause lasting damage if you get appropriate treatment. However, pain, weakness or numbness associated with chronic exertional compartment syndrome may prevent you from continuing to exercise or practice your sport at the same level of intensity.
Diagnosis
Other exercise-related problems are more common than chronic exertional compartment syndrome, so your doctor may first try to rule out other causes — such as shin splints or stress fractures — before moving on to more specialized testing.
Results of physical exams for chronic exertional compartment syndrome are often normal. Your doctor might prefer to examine you after you've exercised to the point of bringing on symptoms. Your doctor may notice a muscle bulge, tenderness or tension in the affected area.
Imaging studies
Imaging studies may include:
-
MRI. A typical MRI scan of your legs can be used to evaluate the structure of the muscles in the compartments and rule out other possible causes of your symptoms.
An advanced MRI scan can help assess the fluid volumes of the compartments. Images are taken at rest, while moving your foot until you feel symptoms, and after the exercise. This type of MRI scan has been found to be accurate in detecting chronic exertional compartment syndrome, and may reduce the need for the invasive compartment pressure testing.
- Near infrared spectroscopy (NIRS). NIRS is a newer technique that measures the amount of oxygen in your blood in the affected tissue. The test is done at rest and after physical activity. This helps determine if your muscle compartment has decreased blood flow.
Compartment pressure testing
If results from imaging studies do not show a stress fracture or similar cause of pain, your doctor might suggest measuring the pressure within your muscle compartments.
This test, often called compartment pressure measurement, is the gold standard for diagnosing chronic exertional compartment syndrome. The test involves the insertion of a needle or catheter into your muscle before and after exercise to make the measurements.
Because it's invasive and mildly painful, compartment pressure measurement usually isn't performed unless your medical history and other tests strongly suggest you have this condition.
Treatment
Options to treat chronic exertional compartment syndrome include both nonsurgical and surgical methods. However, nonsurgical measures are typically successful only if you stop or greatly reduce the activity that caused the condition.
Nonsurgical options
Your doctor may initially recommend pain medications, physical therapy, athletic shoe inserts (orthotics), massage or a break from exercise. Changing how you land on your feet when you jog or run also might be helpful. However, nonsurgical options typically don't provide lasting benefit for true chronic exertional compartment syndrome.
Injections of botulinum toxin A (Botox) into the muscles of the leg may also help treat chronic exertional compartment syndrome, but more research needs to be done on this treatment option. Your doctor may use numbing injections beforehand to help map the affected area and determine what Botox dose is needed.
Surgical options
A surgical procedure called fasciotomy is the most effective treatment of chronic exertional compartment syndrome. It involves cutting open the inflexible tissue encasing each of the affected muscle compartments. This relieves the pressure.
Sometimes, a fasciotomy can be performed through small incisions, which may reduce recovery time and allow you to return to your regular sport or activity sooner.
Although surgery is effective for most people, it's not without risk and, in some cases, it may not completely alleviate symptoms associated with chronic exertional compartment syndrome. Complications of the surgery can include infection, permanent nerve damage, numbness, weakness, bruising and scarring.
Lifestyle and home remedies
To help relieve the pain of chronic exertional compartment syndrome, try the following:
- Use orthotics or wear better athletic shoes.
- Limit your physical activities to those that don't cause pain, especially focusing on low-impact activities such as cycling or an elliptical trainer. For example, if running bothers your legs, try swimming. Or try running on softer surfaces.
- Stretch the painful limb after exercise.
Preparing for an appointment
You're likely to start by seeing your family doctor. He or she may refer you to a doctor who specializes in sports medicine or orthopedic surgery.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment
- Key personal information, including what sports you participate in, the type of exercise you do, and how much and how often you exercise
- All medications, vitamins or other supplements you take, including the doses
- Questions to ask your doctor
Get copies of recent imaging tests you've had, if possible. Ask your doctor's staff how you can get these forwarded to your doctor before the appointment.
Take a family member or friend along, if possible, to help you remember the information you're given.
For chronic exertional compartment syndrome, questions to ask your doctor include:
- What's the most likely cause of my symptoms?
- Are there other possible causes?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What treatments are available, and which do you recommend?
- I have other health conditions. How can I best manage these conditions together?
- Are there restrictions I need to follow, such as avoiding certain activities?
- Should I see a specialist? If so, whom do you recommend?
- Are there brochures or other printed materials I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you several questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- How soon do your symptoms start after you begin your activity?
- How quickly do your symptoms resolve after you stop your activity?
- Do you notice weakness in your legs or feet?
- Do you have numbness or tingling?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.