Claudication is pain caused by too little blood flow to muscles during exercise. Most often this pain occurs in the legs after walking at a certain pace and for a certain amount of time — depending on the severity of the condition.
The condition is also called intermittent claudication because the pain usually isn't constant. It begins during exercise and ends with rest. As claudication worsens, however, the pain may occur during rest.
Claudication is technically a symptom of disease, most often peripheral artery disease, a narrowing of arteries in the limbs that restricts blood flow.
Treatments focus on lowering the risks of vascular disease, reducing pain, increasing mobility and preventing damage to tissues.
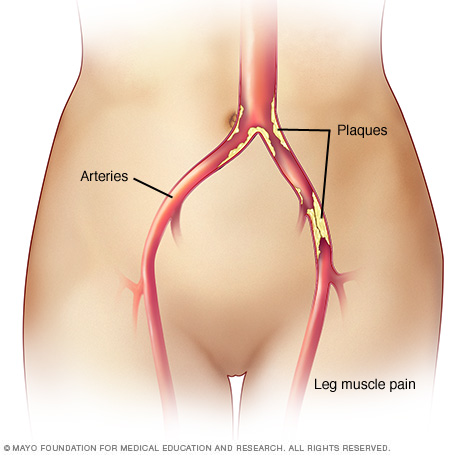
Claudication is pain in the legs or arms that occurs while walking or using the arms. The pain is caused by too little blood flow to the legs or arms. Claudication is usually a symptom of peripheral artery disease, in which the arteries that supply blood to the arms or legs, usually the legs, are narrowed. The narrowing is usually due to a buildup of fatty deposits (plaques) on the artery walls.
Symptoms
Claudication refers to muscle pain due to lack of oxygen that's triggered by activity and relieved by rest. Symptoms include the following:
- Pain, ache, discomfort or fatigue in muscles every time those muscles are used
- Pain in the calves, thighs, buttocks, hips or feet
- Less often, pain in shoulders, biceps and forearms
- Pain that gets better soon after resting
The pain may become more severe over time. You may even start to have pain at rest.
Signs or symptoms of peripheral artery disease, usually in more-advanced stages, include:
- Cool skin
- Severe, constant pain that progresses to numbness
- Skin discoloration
- Wounds that don't heal
When to see a doctor
Talk to your health care provider if you have pain in your legs or arms when you exercise. Claudication can lead to a cycle that results in worsening cardiovascular health. Pain may make exercise intolerable, and a lack of exercise results in poorer health.
Peripheral artery disease is a sign of poor cardiovascular health and an increased risk of heart attack and stroke.
Other conditions involving the blood, nerves and bones can contribute to leg and arm pain during exercise. It's important to have a complete exam and appropriate tests to diagnose potential causes of pain.
Causes
Claudication is most often a symptom of peripheral artery disease. The peripheral arteries are the large vessels that deliver blood to the legs and arms.
Peripheral artery disease is damage to an artery that restricts the flow of blood in an arm or leg (a limb). When you're at rest, the limited blood flow is generally enough. When you're active, however, the muscles aren't getting enough oxygen and nutrients to work well and remain healthy.
Damage to peripheral arteries is usually caused by atherosclerosis. Atherosclerosis is the buildup of fats, cholesterol and other substances in and on the artery walls. This buildup is called plaque. The plaque can cause the arteries to narrow, blocking blood flow. The plaque can also burst, leading to a blood clot.

If there's too much cholesterol in the blood, the cholesterol and other substances may form deposits (plaques) that collect on artery walls. Plaques can cause an artery to become narrowed or blocked. If a plaque ruptures, a blood clot can form. Plaques and blood clots can reduce blood flow through an artery.
Risk factors
Potential risk factors for peripheral artery disease and claudication include:
- A family history of atherosclerosis, peripheral artery disease or claudication
- Age older than 50 years if you also smoke or have diabetes
- Age older than 70 years
- Chronic kidney disease
- Diabetes
- High blood pressure
- High cholesterol
- Obesity (a body mass index, or BMI, over 30)
- Smoking
Complications
Claudication is generally considered a warning of significant atherosclerosis, indicating an increased risk of heart attack or stroke. Other complications of peripheral artery disease due to atherosclerosis include:
- Skin lesions that don't heal
- Death of muscle and skin tissues (gangrene)
- Amputation of a limb
Prevention
The best way to prevent claudication is to maintain a healthy lifestyle and control certain medical conditions. That means:
- Eat a healthy, well-balanced diet
- Exercise regularly
- If you have diabetes, keep your blood sugar in good control
- Maintain a healthy weight
- Manage cholesterol and blood pressure
- Quit smoking if you're a smoker
Diagnosis
Claudication may go undiagnosed because many people consider the pain to be an unwelcome but typical part of aging. Some people simply reduce their activity level to avoid the pain.
A diagnosis of claudication and peripheral artery disease is based on a review of symptoms, a physical exam, evaluation of the skin on the limbs, and tests to check blood flow.
Tests
Some common tests used to diagnose claudication may include:
- Pulse measurement in your palms or feet to assess blood flow to the entire limb
- Ankle-brachial index, a comparison of blood pressure in the ankles with the blood pressure in the arms
- Segmental blood pressure measurement, a series of blood pressure measurements at different areas on the arm or leg to help determine the amount and location of damage to the arteries
- Exercise testing to determine the maximum distance you can walk or the maximum exertion without pain
- Doppler ultrasound to see the flow of blood
- MRI or CT angiography to look for narrowed blood vessels
Treatment
The goals of treating claudication and peripheral artery disease are to reduce pain and manage the risk factors that contribute to heart and blood vessel (cardiovascular) disease.
Exercise is an important part of claudication treatment. Exercise reduces pain, increases exercise duration, improves vascular health in the affected limbs, and contributes to weight management and an overall improvement in quality of life.
Recommended walking programs include:
- Walking until you feel moderate pain or as far as you can
- Resting to relieve pain
- Walking again
- Repeating the walk-rest-walk cycle for 30 to 45 minutes
- Walking three or more days a week
Supervised exercise is recommended for beginning the treatment, but long-term exercise at home is important for ongoing management of claudication.
Medications
Your health care provider may prescribe one or more medications to control pain and manage risk factors for cardiovascular disease. For example, medications may be used to manage the following:
- Pain. The drug cilostazol, which improves blood flow, may reduce pain during exercise and help you to walk further.
- High cholesterol. Statins are a drugs that help lower cholesterol, a key factor in the formation of plaques in arteries. Taking statins may improve walking distance.
- High blood pressure. Several different classes of drugs may be prescribed to lower blood pressure and reduce the risk of heart attack or stroke.
- Other cardiovascular risks. Anti-platelet drugs, which help prevent blood clots, may reduce the risk of heart attack, stroke or clots blocking blood flow to limbs. These drugs include aspirin, clopidogrel (Plavix) and other classes of drugs.
Talk to your doctor about medications or supplements that you shouldn't take with your prescribed treatment.
Surgery or other procedures
When peripheral artery disease is severe and other treatments don't work, surgery may be required. Options include:
- Angioplasty. This procedure improves blood flow by widening a damaged artery. A health care provider guides a narrow tube through blood vessels to deliver an inflatable balloon that expands the artery. Once the artery is widened, the health care provider may place a small metal or plastic mesh tube (stent) in the artery to keep it open.
- Vascular surgery. During this type of surgery, a surgeon takes a healthy blood vessel from another part of the body to replace the vessel that's causing claudication. This allows blood to flow around the blocked or narrowed artery.
Lifestyle and home remedies
A healthy lifestyle can help improve treatment outcomes and lower risks associated with claudication and peripheral artery disease. Recommended lifestyle changes include the following:
- Quit smoking. Smoking greatly increases the risk of complications of peripheral artery disease. Talk to your health care provider if you need help quitting.
- Exercise. Follow the exercise plan recommended by your health care provider. Regular exercise is important for weight management and good heart health.
- Eat a healthy diet. Eat plenty of low-starch vegetables, fruits and whole grains, and modest portions of lean meats, poultry, fish and low-fat dairy.
- Foot care. Talk to your health care provider about proper foot care. Know how to inspect your feet to ensure proper and prompt treatment of injuries. Wear socks and appropriate shoes to support and protect your feet.
Coping and support
Learning all you can about what's causing your claudication may help you better manage the condition.
Some people also find it helpful to talk with other people who are going through similar experiences. In a support group, you may find encouragement, advice, and maybe even an exercise partner or two. Ask your health care provider if there are any support groups in your area.
Preparing for an appointment
You're likely to start by seeing your health care provider. You may be referred to a doctor trained in heart diseases (cardiologist) or a blood vessel (vascular) surgeon.
To make the best of your appointment time, be prepared to answer the following questions:
- When did symptoms begin?
- Do you have pain when you're walking or exercising, when you're at rest, or both?
- On a scale of 1 to 10 (10 being the worst), how would you rate the pain?
- Does anything seem to improve symptoms, such as resting?
- Do you need to sit down to get symptom relief, or does stopping and standing in one place relieve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Is the pain keeping you from regular exercise or normal daily activities?
- Are you having any other symptoms?
- Have you recently started or stopped taking any medications or supplements?
- Do you have a personal history or family history of high blood pressure, high cholesterol, diabetes, heart disease or stroke?
What you can do
Your health care provider may ask about the medications you take, including supplements and drugs bought without a prescription. Before your appointment, write down each drug's name, dosage, reason for taking it and the name of the prescribing provider. Bring the list with you to your appointment.
Other strategies to help you use your appointment time well include the following:
- Bring a family member or friend along to help you remember the information you're given.
- During your appointment, ask your health care provider about anything you don't understand.
- Take notes or ask for a printed document outlining next steps for scheduling tests or additional appointments.
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.