Creutzfeldt-Jakob (KROITS-felt YAH-kobe) disease (CJD) is a degenerative brain disorder that leads to dementia and, ultimately, death. Creutzfeldt-Jakob disease symptoms can be similar to those of other dementia-like brain disorders, such as Alzheimer's disease. But Creutzfeldt-Jakob disease usually progresses much more rapidly.
CJD captured public attention in the 1990s when some people in the United Kingdom developed a form of the disease — variant CJD (vCJD) — after eating meat from diseased cattle. However, "classic" Creutzfeldt-Jakob disease hasn't been linked to contaminated beef. All types of CJD are serious, but very rare. Worldwide, about one to two cases of CJD are diagnosed per million people each year, most often in older adults.
Symptoms
Creutzfeldt-Jakob disease is marked by rapid mental deterioration, usually within a few months. Early signs and symptoms typically include:
- Personality changes
- Memory loss
- Impaired thinking
- Blurred vision or blindness
- Insomnia
- Incoordination
- Difficulty speaking
- Difficulty swallowing
- Sudden, jerky movements
As the disease progresses, mental symptoms worsen. Most people eventually fall into a coma. Heart failure, lung (respiratory) failure, pneumonia or other infections are generally the cause of death, which usually occurs within a year.
In people with the rarer vCJD, psychiatric symptoms may be more apparent in the beginning. In many cases, dementia — the loss of the ability to think, reason and remember — develops later in the illness. vCJD also affects people at a younger age and appears to last 12 to 14 months.
Causes
Creutzfeldt-Jakob disease and its variants belong to a broad group of human and animal diseases known as transmissible spongiform encephalopathies (TSEs). The name derives from the spongy holes, visible under a microscope, that develop in affected brain tissue.
The cause of Creutzfeldt-Jakob disease and other TSEs appears to be abnormal versions of a kind of protein called a prion. Normally these proteins are produced in our bodies and are harmless. But when they're misshapen, they become infectious and can harm normal biological processes.
How CJD is transmitted
The risk of CJD is low. The disease can't be spread through coughing or sneezing, touching, or sexual contact. CJD can develop in three ways:
- Sporadically. Most people with classic CJD develop the disease for no apparent reason. This type, called spontaneous CJD or sporadic CJD, accounts for most cases.
- By inheritance. Fewer than 15% of people with CJD have a family history of the disease or test positive for a genetic mutation associated with CJD. This type is referred to as familial CJD.
-
By contamination. A small number of people have developed CJD after being exposed to infected human tissue during a medical procedure, such as a cornea or skin transplant. Also, because standard cleaning methods don't destroy abnormal prions, a few people have developed CJD after undergoing brain surgery with contaminated instruments. A small number of people have also developed the disease from eating contaminated beef.
Cases of CJD related to medical procedures are referred to as iatrogenic CJD. Variant CJD is linked primarily to eating beef infected with mad cow disease (bovine spongiform encephalopathy, or BSE).
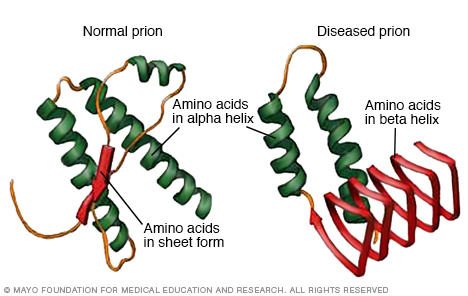
Prions are proteins that occur naturally in the brains of animals and people. Normally, the proteins are harmless, but when they're misshapen, they can cause devastating illnesses such as BSE disease in cattle and Creutzfeldt-Jakob disease in humans.
Risk factors
Most cases of Creutzfeldt-Jakob disease occur for unknown reasons, and no risk factors can be identified. However, a few factors seem to be associated with different kinds of CJD:
- Age. Sporadic CJD tends to develop later in life, usually around age 60. Onset of familial CJD occurs slightly earlier, and vCJD has affected people at a much younger age, usually in their late 20s.
- Genetics. People with familial CJD have a genetic mutation that causes the disease. To develop familial CJD, a child must have one copy of the mutated gene, which is inherited from either parent. If you have the mutation, the chance of passing it on to your children is 50%.
-
Exposure to contaminated tissue. People who've received infected manufactured human growth hormone, or who've had transplants of the infected tissues that cover the brain (dura mater), may be at risk of iatrogenic CJD.
The risk of getting vCJD from eating contaminated beef is very low. In general, if countries are effectively implementing public health measures, the risk is virtually nonexistent. Chronic wasting disease (CWD) is a prion disease that affects deer, elk, reindeer and moose. It has been found in some areas of North America. To date, no documented cases of CWD have caused disease in humans.

In an autosomal dominant disorder, the altered gene is a dominant gene located on one of the nonsex chromosomes (autosomes). You need only one altered gene to be affected by this type of disorder. A person with an autosomal dominant disorder — in this case, the father — has a 50% chance of having an affected child with one altered gene (dominant gene) and a 50% chance of having an unaffected child with two typical genes (recessive genes).
Complications
Creutzfeldt-Jakob disease greatly affects the brain and body. CJD usually progresses quickly. Over time, people with CJD withdraw from friends and family and eventually lose the ability to recognize or relate to them. They also lose the ability to care for themselves and many eventually slip into a coma. The disease is always fatal.
Prevention
There's no known way to prevent sporadic Creutzfeldt-Jakob disease (CJD). If you have a family history of neurological disease, you may benefit from talking with a genetics counselor. He or she can help you sort through the risks associated with your situation.
Preventing iatrogenic CJD
Hospitals and other medical institutions follow clear policies to prevent iatrogenic CJD. These measures have included:
- Exclusive use of man-made human growth hormone, rather than the kind derived from human pituitary glands
- Destruction of surgical instruments used on the brain or nervous tissue of someone with known or suspected CJD
- Single-use kits for spinal taps (lumbar punctures)
To help ensure the safety of the blood supply, people with a risk of exposure to CJD or vCJD aren't eligible to donate blood in the United States. This includes people who:
- Have a biological relative who has been diagnosed with familial CJD
- Have received a dura mater brain graft
- Have received cadaveric human growth hormone
- Spent at least three months in the United Kingdom from 1980 to 1996
- Spent five years or more in France or Ireland between1980 and 2001
- Received a blood transfusion in the U.K., France or Ireland since 1980
The U.K., as well as some other countries, also has certain restrictions regarding blood donations from people with a risk of exposure to CJD or vCJD.
Preventing vCJD
The risk of getting vCJD in the United States remains very low. Only four cases have been reported in the U.S. According to the U.S. Centers for Disease Control and Prevention (CDC), strong evidence suggests that these cases were acquired in other countries outside of the U.S.
In the United Kingdom, where the majority of vCJD cases have occurred, fewer than 200 cases have been reported. CJD incidence peaked in the U.K. between 1999 and 2000 and has been declining since. A very small number of other vCJD cases also have been reported in other countries worldwide.
To date, there is no evidence that people can develop vCJD from consuming meat of animals infected with CWD prions. Nonetheless, the CDC recommends that hunters strongly consider having deer and elk tested before eating the meat in areas where CWD is known to be present. In addition, hunters should avoid shooting or handling meat from deer or elk that appear sick or are found dead.
Regulating potential sources of vCJD
Most countries have taken steps to prevent BSE-infected tissue from entering the food supply, including:
- Tight restrictions on importation of cattle from countries where BSE is common
- Restrictions on animal feed
- Strict procedures for dealing with sick animals
- Surveillance and testing methods for tracking cattle health
- Restrictions on which parts of cattle can be processed for food
Diagnosis
Only a brain biopsy or an exam of brain tissue after death (autopsy) can confirm the presence of Creutzfeldt-Jakob disease (CJD). But doctors often can make an accurate diagnosis based on your medical and personal history, a neurological exam, and certain diagnostic tests.
The exam is likely to reveal characteristic symptoms such as muscle twitching and spasms, abnormal reflexes, and coordination problems. People with may also have areas of blindness and changes in visual-spatial perception.
In addition, doctors commonly use these tests to help detect CJD:
- Electroencephalogram (EEG). This test measures the brain's electrical activity using electrodes placed on the scalp. People with and vCJD show a characteristically abnormal pattern.
- MRI. This imaging technique uses radio waves and a magnetic field to create cross-sectional images of the head and body. It's especially useful in diagnosing brain disorders because of its high-resolution images of the brain's white and gray matter.
-
Spinal fluid tests. Cerebral spinal fluid surrounds and cushions the brain and spinal cord. In a test called a lumbar puncture — commonly known as a spinal tap — doctors use a needle to withdraw a small amount of this fluid for testing. This test is often used to rule out other neurological diseases, but elevation of certain proteins that usually occurs in the brain may indicate CJD or vCJD.
Real-time quaking-induced conversion (RT-QuIC), is a newer test that can detect the presence of the prion proteins that cause in spinal fluid and help establish the diagnosis.
Treatment
No effective treatment exists for Creutzfeldt-Jakob disease or any of its variants. Many drugs have been tested and haven't shown benefits. For that reason, doctors focus on relieving pain and other symptoms and on making people with these diseases as comfortable as possible.
Preparing for an appointment
You're likely to start by seeing your family doctor or a general doctor. In some cases when you call for an appointment, you may be referred immediately to a brain specialist (neurologist).
Here's some information to help you prepare for your appointment.
What you can do
- List your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including recent life changes.
- List medications, vitamins and supplements you take.
- Bring a family member or friend along, if possible. Someone who accompanies you might help you remember something you missed or forgot.
- Write down questions to ask your doctor.
For Creutzfeldt-Jakob disease, some basic questions to ask your doctor include:
- What is likely causing my symptoms?
- Other than the most likely cause, what are other possible causes for my symptoms?
- What tests do I need?
- What is the best course of action?
- Are there restrictions I need to follow?
- Should I see a specialist?
- I have other medical conditions. How do I manage them together?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, including:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Has anyone in your family had Creutzfeldt-Jakob disease?
- Have you lived or traveled extensively outside the United States?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.