Glioma is a type of tumor that occurs in the brain and spinal cord. Gliomas begin in the gluey supportive cells (glial cells) that surround nerve cells and help them function.
Three types of glial cells can produce tumors. Gliomas are classified according to the type of glial cell involved in the tumor, as well as the tumor's genetic features, which can help predict how the tumor will behave over time and the treatments most likely to work.
Types of glioma include:
- Astrocytomas, including astrocytoma, anaplastic astrocytoma and glioblastoma
- Ependymomas, including anaplastic ependymoma, myxopapillary ependymoma and subependymoma
- Oligodendrogliomas, including oligodendroglioma, anaplastic oligodendroglioma and anaplastic oligoastrocytoma
A glioma can affect your brain function and be life-threatening depending on its location and rate of growth.
Gliomas are one of the most common types of primary brain tumors.
The type of glioma you have helps determine your treatment and your prognosis. In general, glioma treatment options include surgery, radiation therapy, chemotherapy, targeted therapy and experimental clinical trials.

Gliomas begin in the gluey supportive (glial cells) that surround nerve cells in the brain.
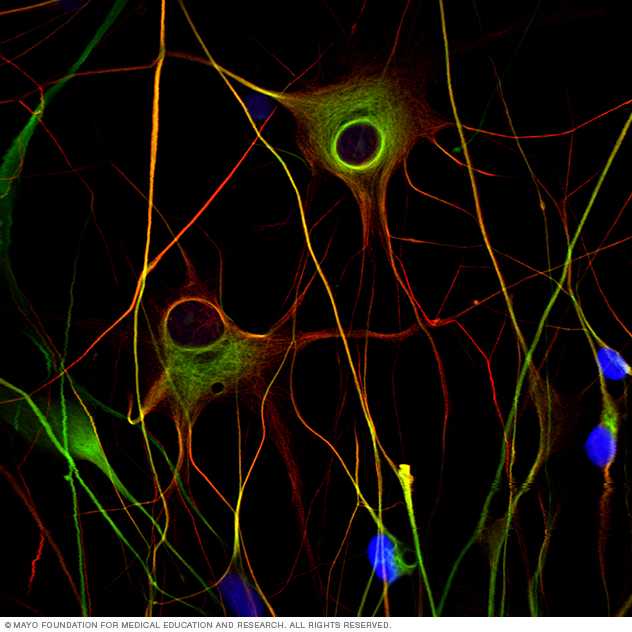
Glioblastoma multiforme (malignant brain tumor) cells. The cells have irregular shapes with fingers that can spread into the brain.
Symptoms
The symptoms of glioma vary by tumor type as well as the tumor's size, location and rate of growth.
Common signs and symptoms of gliomas include:
- Headache
- Nausea or vomiting
- Confusion or a decline in brain function
- Memory loss
- Personality changes or irritability
- Difficulty with balance
- Urinary incontinence
- Vision problems, such as blurred vision, double vision or loss of peripheral vision
- Speech difficulties
- Seizures, especially in someone without a history of seizures
When to see a doctor
Make an appointment with your doctor if you have any signs and symptoms common to glioma.
Causes
Like most primary brain tumors, the exact cause of gliomas is not known. But there are some factors that may increase your risk of a brain tumor.
Risk factors
Like most primary brain tumors, the exact cause of gliomas is not known. But there are some factors that may increase your risk of a brain tumor. Risk factors include:
- Your age. Your risk of a brain tumor increases as you age. Gliomas are most common in adults between ages 45 and 65 years old. However, a brain tumor can occur at any age. Certain types of gliomas, such as ependymomas and pilocytic astrocytomas, are more common in children and young adults.
-
Exposure to radiation. People who have been exposed to a type of radiation called ionizing radiation have an increased risk of brain tumor. Examples of ionizing radiation include radiation therapy used to treat cancer and radiation exposure caused by atomic bombs.
More-common forms of radiation, such as electromagnetic fields from power lines and radiofrequency radiation from microwave ovens have not been shown to increase the risk of glioma.
It isn't clear whether cellphone use increases the risk of brain cancer. Some studies have found a possible association between cellphone use and a type of brain cancer called acoustic neuroma. Many other studies have found no association. Because cellphones are a relatively new factor, more long-term research is needed to understand the potential impact on cancer risk. For the time being, if you're concerned about the possible link between cellphones and cancer, experts recommend limiting your exposure by using a speaker or hands-free device, which keeps the cellphone itself away from your head.
- Family history of glioma. It's rare for glioma to run in families. But having a family history of glioma can double the risk of developing it. Some genes have been weakly associated with glioma, but more study is needed to confirm a link between these genetic variations and brain tumors.
Diagnosis
If your primary care doctor suspects you have a brain tumor, you may be referred to a specialist who is trained in treating brain and nervous system disorders (neurologist). Your doctor may recommend a number of tests and procedures, including:
- A neurological exam. During a neurological exam, your doctor may check your vision, hearing, balance, coordination, strength and reflexes. Problems in one or more of these areas may provide clues about the part of your brain that could be affected by a brain tumor.
-
Imaging tests. Magnetic resonance imaging (MRI) is often used to help diagnose brain tumors. In some cases, a dye (contrast material) may be injected through a vein in your arm during your MRI study to help show differences in brain tissue.
A number of specialized MRI scan components — including functional MRI, perfusion MRI and magnetic resonance spectroscopy — may help your doctor evaluate the tumor and plan treatment.
Other imaging tests may include computerized tomography (CT) scan and positron emission tomography (PET).
- Tests to find cancer in other parts of your body. To rule out other types of brain tumors that may have spread from other parts of the body, your doctor may recommend tests and procedures to determine where the cancer originated. Gliomas originate within the brain and are not the result of cancer that has spread (metastasized) from elsewhere.
-
Collecting and testing a sample of abnormal tissue (biopsy). Depending on the location of the glioma, a biopsy may be performed with a needle before treatment or as part of an operation to remove the brain tumor.
A stereotactic needle biopsy may be done for gliomas in hard-to-reach areas or very sensitive areas within your brain that might be damaged by a more extensive operation. During a stereotactic needle biopsy, your neurosurgeon drills a small hole into your skull. A thin needle is then inserted through the hole. Tissue is removed through the needle, which is frequently guided by CT or MRI scanning.
The biopsy sample is then analyzed under a microscope to determine if it's cancerous or benign.
A biopsy is the only way to definitively diagnose a brain tumor and give a prognosis to guide treatment decisions. Based on this information, a doctor who specializes in diagnosing cancer and other tissue abnormalities (pathologist) can determine the grade or stage of a brain tumor.
The pathologist will also examine the physical appearance and growth rate of your biopsy sample (molecular diagnosis). Your doctor will explain the pathologist's findings to you. This information helps guide decision-making about your treatment plan.

Brain tumor imaging
Treatment
Treatment for glioma depends on the type, size, grade and location of the tumor, as well as your age, overall health and preferences.
In addition to actions to remove the tumor itself, treatment for glioma may also require using drugs to reduce the signs and symptoms of your tumor.
Your doctor may prescribe steroids to reduce swelling and relieve pressure on affected areas of the brain. Anti-epileptic drugs may be used to control seizures.
Surgery
Surgery to remove as much of the tumor as possible is usually the first step in treating most types of gliomas.
In some cases, gliomas are small and easy to separate from surrounding healthy brain tissue, which makes complete surgical removal possible. In other cases, tumors can't be separated from surrounding tissue, or they're located near sensitive areas in your brain and make surgery risky. In these situations your doctor removes as much of the tumor as is safe.
Even removing a portion of the tumor may help reduce your signs and symptoms.
In some cases, neuropathologists may analyze tissue samples removed by a surgeon and report the results while surgery is underway. This information helps the surgeon decide how much tissue to remove.
A variety of surgical technologies and techniques may be used to assist the neurosurgeon in protecting as much healthy brain tissue as possible while removing the tumor, including computer-assisted brain surgery, intraoperative MRI, awake brain surgery and lasers. For example, during awake brain surgery, you may be asked to perform a task with the goal of ensuring the area of the brain controlling that function is not damaged.
Surgery to remove a glioma carries risks, such as infection and bleeding. Other risks may depend on the part of your brain in which your tumor is located. For instance, surgery on a tumor near nerves that connect to your eyes may carry a risk of vision loss.
Radiation therapy
Radiation therapy usually follows surgery in treatment of glioma, especially high-grade gliomas. Radiation uses high-energy beams, such as X-rays or protons, to kill tumor cells. Radiation therapy for glioma comes from a machine outside your body (external beam radiation).
There are several types of external beam radiation currently used and under study for the treatment of glioma. The type of glioma you have, its grade and other prognostic factors are considered in determining the timing and type of radiation therapy you may receive. A doctor who specializes in radiation therapy for cancer (radiation oncologist) will work closely with your other doctors to plan and coordinate the most appropriate radiation treatment for you.
Radiation therapy options include:
- Using computers to pinpoint delivery of radiation treatment to the exact location of the brain tumor. Techniques include intensity-modulated radiation therapy and 3D conformal radiation therapy.
- Using protons — the positive parts of atoms — rather than X-rays as the source of radiation. This technique, called conformal proton beam therapy, delivers radiation only once proton beams reach the tumor, causing less damage than X-rays to surrounding tissue.
- Using multiple beams of radiation to give a highly focused form of radiation treatment. While this technique is called stereotactic radiation therapy (radiosurgery), it doesn't actually involve surgery in the traditional sense. Each beam of radiation isn't particularly powerful, but the point where all the beams meet — at the brain tumor — receives a very large dose of radiation to kill the tumor cells in a very small area.
There are different types of technology used in radiosurgery to deliver radiation to treat brain tumors, such as a Gamma Knife or linear accelerator (LINAC).
Side effects of radiation therapy depend on the type and dose of radiation you receive. Common side effects during or immediately following radiation include fatigue, headaches and scalp irritation.
Chemotherapy
Chemotherapy uses drugs to kill tumor cells. Chemotherapy drugs can be taken in pill form (orally) or injected into a vein (intravenously).
Chemotherapy is usually used in combination with radiation therapy to treat gliomas.
The chemotherapy drug used most often to treat gliomas is temozolomide (Temodar), which is taken as a pill.
Side effects of chemotherapy depend on the type and dose of drugs you receive. Common side effects include nausea and vomiting, headache, hair loss, fever, and weakness. Some side effects may be managed with medication.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
One targeted drug therapy used to treat a type of brain cancer called glioblastoma is bevacizumab (Avastin). This drug, given through a vein (intravenously), stops the formation of new blood vessels, cutting off blood supply to a tumor and killing the tumor cells.
Treatment innovations
Brain cancer research is a very active field of study. Researchers are investigating new ways to deliver drugs to brain tumors, including pumps that release a continuous, slow flow of chemotherapy or targeted drug therapies to a tumor. This type of treatment is called convection-enhanced delivery (CED).
Another type of therapy uses technology called tumor treating fields (Optune) to deliver electric fields to the brain, which can help stop the proliferation of cancer cells. Optune is a wearable, portable device and is used in combination with temozolomide to treat newly diagnosed glioblastoma in adults.
Implanted, biodegradable wafer therapy (Gliadel) relies on an implanted disc to release chemotherapy to tumor tissue that remains after surgery. And in nanoparticle therapy, particles with an unusually high surface area carry chemotherapy across the blood-brain barrier directly to a tumor.
Rehabilitation after treatment
Because brain tumors can develop in parts of the brain that control motor skills, speech, vision and thinking, rehabilitation may be a necessary part of recovery. Your doctor may refer you to services that can help, such as:
- Physical therapy can help you regain lost motor skills or muscle strength
- Occupational therapy, which can help you get back to your normal daily activities, including work, after a brain tumor or other illness
- Speech therapy with specialists in speech difficulties (speech pathologists), which can help if you have difficulty speaking
- Tutoring for school-age children, which can help kids cope with changes in memory and thinking after a brain tumor
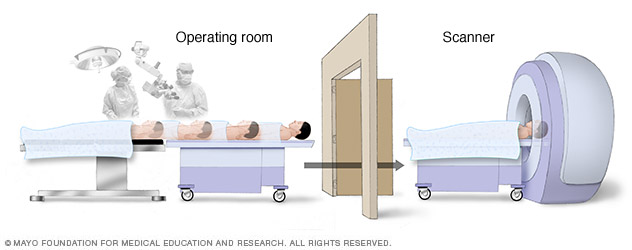
Since the brain can shift during surgery, brain-mapping techniques and intraoperative MRI create accurate pictures of the brain that guide the neurosurgeon in effectively removing only the tumor and avoiding any functional brain tissue, to preserve motor function, language and other important brain functions.
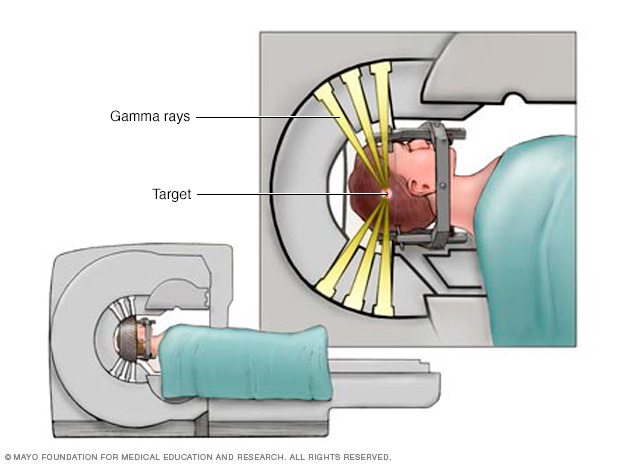
Individual radiation beams are too weak to hurt the brain tissue they travel through on the way to the target. The radiation is most powerful where all the beams intersect.

Physical therapy after glioma treatment can help you regain lost motor skills or muscle strength.

Alternative medicine
Little research has been done on complementary and alternative brain tumor treatments. No alternative treatments have been proved to cure gliomas. However, complementary treatments may help you cope with your brain tumor and its treatment. Talk to your doctor about your options.
Some complementary treatments that may help you cope include:
- Acupuncture
- Hypnosis
- Meditation
- Music therapy
- Relaxation exercises
Coping and support
A diagnosis of a brain tumor can be overwhelming and frightening. It can make you feel like you have little control over your health. But you can take steps to cope with the shock and grief that may come after your diagnosis. Consider trying to:
- Learn enough about gliomas to make decisions about your care. Ask your doctor about your specific type of brain tumor, including your treatment options and, if you like, your prognosis. As you learn more about brain tumors, you may become more confident in making treatment decisions.
- Keep friends and family close. Keeping your close relationships strong will help you deal with your brain tumor. Friends and family can provide the practical support you'll need, such as helping take care of your house if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by cancer.
-
Find someone to talk with. Find a good listener who is willing to listen to you talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your doctor about support groups in your area. Or check your phone book, library or a cancer organization, such as the National Cancer Institute or the American Cancer Society.
Preparing for an appointment
See your doctor if you have any signs or symptoms that worry you. If you're diagnosed with a glioma, you may be referred to specialists, such as:
- Doctors who specialize in brain disorders (neurologists)
- Doctors who treat cancer (oncologists)
- Doctors who use radiation to treat cancer (radiation oncologists)
- Doctors who specialize in nervous system cancers (neuro-oncologists)
- Surgeons who operate on the brain and nervous system (neurosurgeons)
- Rehabilitation specialists
It's a good idea to be well-prepared for your appointment. Here's some information to help you get ready, and what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements that you're taking.
- Consider taking a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor.
Your time with your doctor is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For a brain tumor such as glioma, some basic questions to ask your doctor include:
- What type of brain tumor do I have?
- Where is my brain tumor located?
- How large is my glioma?
- How aggressive is my brain tumor?
- Is my glioma cancerous?
- Will I need additional tests?
- What are my treatment options?
- Can any treatments cure my glioma?
- What are the benefits and risks of each treatment?
- Is there one treatment you feel is best for me?
- Is there a clinical trial available to treat my type of glioma? Is it appropriate for me?
- How will treatment affect my daily activities, like walking, talking and speaking?
- Should I see a specialist? What will that cost, and will my insurance cover it?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
- How often should I see my doctor for checkups?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask other questions that occur to you.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may allow time later to cover other points you want to address. Your doctor may ask:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.