Guillain-Barre (gee-YAH-buh-RAY) syndrome is a rare disorder in which your body's immune system attacks your nerves. Weakness and tingling in your hands and feet are usually the first symptoms.
These sensations can quickly spread, eventually paralyzing your whole body. In its most severe form Guillain-Barre syndrome is a medical emergency. Most people with the condition must be hospitalized to receive treatment.
The exact cause of Guillain-Barre syndrome is unknown. But two-thirds of patients report symptoms of an infection in the six weeks preceding. These include a COVID-19, respiratory or a gastrointestinal infection or Zika virus.
There's no known cure for Guillain-Barre syndrome, but several treatments can ease symptoms and reduce the duration of the illness. Although most people recover completely from Guillain-Barre syndrome, some severe cases can be fatal. While recovery may take up to several years, most people are able to walk again six months after symptoms first started. Some people may have lasting effects from it, such as weakness, numbness or fatigue.
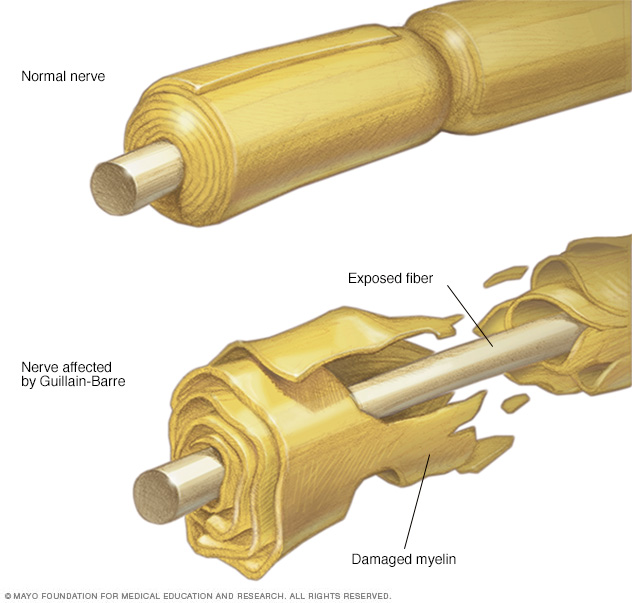
The demyelinating form of Guillain-Barre syndrome destroys the protective covering of the peripheral nerves (myelin sheath), preventing the nerves from transmitting signals to the brain.
Symptoms
Guillain-Barre syndrome often begins with tingling and weakness starting in your feet and legs and spreading to your upper body and arms. Some people notice the first symptoms in the arms or face. As Guillain-Barre syndrome progresses, muscle weakness can turn into paralysis.
Signs and symptoms of Guillain-Barre syndrome may include:
- A pins and needles sensation in your fingers, toes, ankles or wrists
- Weakness in your legs that spreads to your upper body
- Unsteady walking or inability to walk or climb stairs
- Difficulty with facial movements, including speaking, chewing or swallowing
- Double vision or inability to move the eyes
- Severe pain that may feel achy, shooting or cramplike and may be worse at night
- Difficulty with bladder control or bowel function
- Rapid heart rate
- Low or high blood pressure
- Difficulty breathing
People with Guillain-Barre syndrome usually experience their most significant weakness within two weeks after symptoms begin.
Types
Guillain-Barre syndrome has several forms. The main types are:
- Acute inflammatory demyelinating polyradiculoneuropathy (AIDP), the most common form in North America and Europe. The most common sign of AIDP is muscle weakness that starts in the lower part of your body and spreads upward.
- Miller Fisher syndrome (MFS), in which paralysis starts in the eyes. MFS is also associated with unsteady gait. MFS is less common in the U.S. but more common in Asia.
- Acute motor axonal neuropathy (AMAN) and acute motor-sensory axonal neuropathy (AMSAN) are less common in the U.S. But AMAN and AMSAN are more frequent in China, Japan and Mexico.
When to see a doctor
Call your doctor or health care provider if you have mild tingling in your toes or fingers that doesn't seem to be spreading or getting worse. Seek emergency medical help if you have any of these severe signs or symptoms:
- Tingling that started in your feet or toes and is now moving up your body
- Tingling or weakness that's spreading rapidly
- Difficulty catching your breath or shortness of breath when lying flat
- Choking on saliva
Guillain-Barre syndrome is a serious condition that requires immediate hospitalization because it can worsen rapidly. The sooner appropriate treatment is started, the better the chance of a good outcome.
Causes
The exact cause of Guillain-Barre syndrome isn't known. The disorder usually appears days or weeks after a respiratory or digestive tract infection. Rarely, recent surgery or vaccination can trigger Guillain-Barre syndrome. There have been cases reported following infection with the Zika virus. Guillain-Barre syndrome may occur after infection with the COVID-19 virus. It's also a rare reaction in those who receive the Johnson & Johnson or AstraZeneca COVID-19 vaccine.
In Guillain-Barre syndrome, your immune system — which usually attacks only invading organisms — begins attacking the nerves. In AIDP, the nerves' protective covering (myelin sheath) is damaged. The damage prevents nerves from transmitting signals to your brain, causing weakness, numbness or paralysis.
Risk factors
Guillain-Barre syndrome can affect all age groups, but your risk increases as you age. It's also slightly more common in males than females.
Guillain-Barre syndrome may be triggered by:
- Most commonly, infection with campylobacter, a type of bacteria often found in undercooked poultry
- Influenza virus
- Cytomegalovirus
- Epstein-Barr virus
- Zika virus
- Hepatitis A, B, C and E
- HIV, the virus that causes AIDS
- Mycoplasma pneumonia
- Surgery
- Trauma
- Hodgkin's lymphoma
- Rarely, influenza vaccinations or childhood vaccinations
- COVID-19 virus
- COVID-19 Johnson & Johnson and AstraZeneca vaccine
Complications
Guillain-Barre syndrome affects your nerves. Because nerves control your movements and body functions, people with Guillain-Barre may experience:
- Breathing difficulties. The weakness or paralysis can spread to the muscles that control your breathing, a potentially fatal complication. Up to 22% of people with Guillain-Barre syndrome need temporary help from a machine to breathe within the first week when they're hospitalized for treatment.
- Residual numbness or other sensations. Most people with Guillain-Barre syndrome recover completely or have only minor, residual weakness, numbness or tingling.
- Heart and blood pressure problems. Blood pressure fluctuations and irregular heart rhythms (cardiac arrhythmias) are common side effects of Guillain-Barre syndrome.
- Pain. One-third of people with Guillain-Barre syndrome experience severe nerve pain, which may be eased with medication.
- Bowel and bladder function problems. Sluggish bowel function and urine retention may result from Guillain-Barre syndrome.
- Blood clots. People who are immobile due to Guillain-Barre syndrome are at risk of developing blood clots. Until you're able to walk independently, taking blood thinners and wearing support stockings may be recommended.
- Pressure sores. Being immobile also puts you at risk of developing bedsores (pressure sores). Frequent repositioning may help avoid this problem.
- Relapse. A small percentage of people with Guillain-Barre syndrome have a relapse, experiencing muscle weakness even years after the symptoms ended.
Severe, early symptoms of Guillain-Barre syndrome significantly increase the risk of serious long-term complications. Rarely, death may occur from complications such as respiratory distress syndrome and heart attacks.
Diagnosis
Guillain-Barre syndrome can be difficult to diagnose in its earliest stages. Its signs and symptoms are similar to those of other neurological disorders and may vary from person to person.
Your doctor is likely to start with a medical history and thorough physical examination.
Your doctor may then recommend:
- Spinal tap (lumbar puncture). A small amount of fluid is withdrawn from the spinal canal in your lower back. The fluid is tested for a type of change that commonly occurs in people who have Guillain-Barre syndrome.
- Electromyography. Thin-needle electrodes are inserted into the muscles your doctor wants to study. The electrodes measure nerve activity in the muscles.
- Nerve conduction studies. Electrodes are taped to the skin above your nerves. A small shock is passed through the nerve to measure the speed of nerve signals.
Treatment
There's no cure for Guillain-Barre syndrome. But two types of treatments can speed recovery and reduce the severity of the illness:
- Plasma exchange (plasmapheresis). The liquid portion of part of your blood (plasma) is removed and separated from your blood cells. The blood cells are then put back into your body, which manufactures more plasma to make up for what was removed. Plasmapheresis may work by ridding plasma of certain antibodies that contribute to the immune system's attack on the peripheral nerves.
- Immunoglobulin therapy. Immunoglobulin containing healthy antibodies from blood donors is given through a vein (intravenously). High doses of immunoglobulin can block the damaging antibodies that may contribute to Guillain-Barre syndrome.
These treatments are equally effective. Mixing them or administering one after the other is no more effective than using either method alone.
You are also likely to be given medication to:
- Relieve pain, which can be severe
- Prevent blood clots, which can develop while you're immobile
People with Guillain-Barre syndrome need physical help and therapy before and during recovery. Your care may include:
- Movement of your arms and legs by caregivers before recovery, to help keep your muscles flexible and strong
- Physical therapy during recovery to help you cope with fatigue and regain strength and proper movement
- Training with adaptive devices, such as a wheelchair or braces, to give you mobility and self-care skills
Recovery
Although some people can take months and even years to recover, most people with Guillain-Barre syndrome experience this general timeline:
- After the first signs and symptoms, the condition tends to progressively worsen for about two weeks
- Symptoms reach a plateau within four weeks
- Recovery begins, usually lasting 6 to 12 months, though for some people it could take as long as three years
Among adults recovering from Guillain-Barre syndrome:
- About 80% can walk independently six months after diagnosis
- About 60% fully recover motor strength one year after diagnosis
- About 5% to 10% have very delayed and incomplete recovery
Children, who rarely develop Guillain-Barre syndrome, generally recover more completely than adults.
Coping and support
A diagnosis of Guillain-Barre syndrome can be emotionally difficult. Although most people eventually recover fully, the condition is generally painful and requires hospitalization and months of rehabilitation. You must adjust to limited mobility and fatigue.
To manage the stress of recovery from Guillain-Barre syndrome, consider these suggestions:
- Maintain a strong support system of friends and family
- Contact a support group, for yourself or for family members
- Discuss your feelings and concerns with a counselor
Preparing for an appointment
You may be referred to a doctor who specializes in disorders of the brain and nervous system (neurologist).
What you can do
- Write down your symptoms, including any that may seem unrelated to the reason why you scheduled the appointment.
- Make a list of all your medications, vitamins and supplements.
- Write down your key medical information, including other conditions.
- Write down key personal information, including any recent changes or stressors in your life.
- Write down questions to ask your doctor.
- Ask a relative or friend to accompany you, to help you remember what the doctor says.
Questions to ask your doctor
- What's the most likely cause of my symptoms?
- What kinds of tests do I need?
- What kind of treatments do I need?
- How soon do you expect my symptoms to improve with treatment?
- How fully do you expect I'll recover?
- How long will recovery take?
- Am I at risk of long-term complications?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may leave time to go over points you want to spend more time on. You may be asked:
- What are your symptoms, and what parts of your body are affected?
- When did you first begin experiencing symptoms? Did they start suddenly or gradually?
- Do your symptoms seem to be spreading or getting worse?
- If you are experiencing weakness, does it affect one or both sides of your body?
- Have you had problems with bladder or bowel control?
- Have you had any problems with vision, breathing, chewing or swallowing?
- Have you recently had an infectious illness?
- Have you recently spent time in a forested area or traveled abroad?
- Have you recently had any medical procedures, including vaccinations?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.