An incompetent cervix, also called a cervical insufficiency, occurs when weak cervical tissue causes or contributes to premature birth or the loss of an otherwise healthy pregnancy.
Before pregnancy, your cervix — the lower part of the uterus that opens to the vagina — is normally closed and firm. As pregnancy progresses and you prepare to give birth, the cervix gradually softens, decreases in length (effaces) and opens (dilates). If you have an incompetent cervix, your cervix might begin to open too soon — causing you to give birth too early.
An incompetent cervix can be difficult to diagnose and treat. If your cervix begins to open early, or you have a history of cervical insufficiency, your doctor might recommend preventive medication during pregnancy, frequent ultrasounds or a procedure that closes the cervix with strong sutures (cervical cerclage).
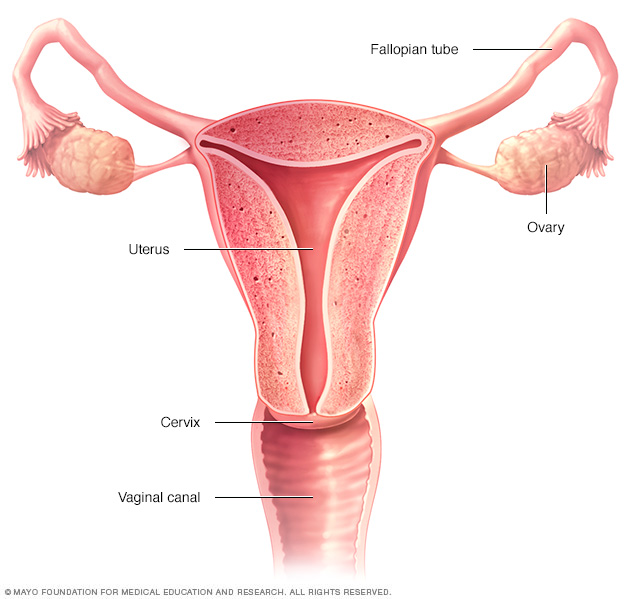
The ovaries, fallopian tubes, uterus, cervix and vagina (vaginal canal) make up the female reproductive system.
Symptoms
If you have an incompetent cervix, you may not have any signs or symptoms during early pregnancy. Some women have mild discomfort or spotting over the course of several days or weeks starting between 14 and 20 weeks of pregnancy.
Be on the lookout for:
- A sensation of pelvic pressure
- A new backache
- Mild abdominal cramps
- A change in vaginal discharge
- Light vaginal bleeding
Risk factors
Many women don't have a known risk factor. Risk factors for cervical insufficiency include:
- Cervical trauma. Some surgical procedures used to treat cervical abnormalities associated with an abnormal Pap smear can result in cervical insufficiency. Other surgical procedures such as a D&C could also be associated with cervical insufficiency. Rarely, a cervical tear during a previous labor and delivery could be associated with an incompetent cervix.
- Race. Black women seem to have a higher risk of developing cervical insufficiency. It isn't clear why.
- Congenital conditions. Uterine abnormalities and genetic disorders affecting a fibrous type of protein that makes up your body's connective tissues (collagen) might cause an incompetent cervix. Exposure to diethylstilbestrol (DES), a synthetic form of the hormone estrogen, before birth also has been linked to cervical insufficiency.
Complications
An incompetent cervix poses risks for your pregnancy — particularly during the second trimester — including:
- Premature birth
- Pregnancy loss
Prevention
You can't prevent an incompetent cervix — but there's much you can do to promote a healthy, full-term pregnancy. For example:
- Seek regular prenatal care. Prenatal visits can help your doctor monitor your health and your baby's health. Mention any signs or symptoms that concern you, even if they seem silly or unimportant.
- Eat a healthy diet. During pregnancy, you'll need more folic acid, calcium, iron and other essential nutrients. A daily prenatal vitamin — ideally starting a few months before conception — can help fill any dietary gaps.
- Gain weight wisely. Gaining the right amount of weight can support your baby's health. A weight gain of 25 to 35 pounds (about 11 to 16 kilograms) is often recommended for women who have a healthy weight before pregnancy.
- Avoid risky substances. If you smoke, quit. Alcohol and illegal drugs are off-limits, too. In addition, get your doctor's OK before taking any medications or supplements — even those available over-the-counter.
If you've had an incompetent cervix during one pregnacy, you're at risk of premature birth or pregnancy loss in later pregnancies. If you're considering getting pregnant again, talk with your doctor to understand the risks and what you can do to promote a healthy pregnancy.
Diagnosis
An incompetent cervix can only be detected during pregnancy. Even then diagnosis can be difficult — particularly during a first pregnancy.
Your doctor will ask about any symptoms you're having and your medical history. Be sure to let your doctor know if you've had a pregnancy loss during the second trimester or if you had a procedure on your cervix.
Your doctor might diagnose an incompetent cervix if you have:
- A history of painless cervical dilation and second trimester deliveries
- Advanced cervical dilation and effacement before week 24 of pregnancy without painful contractions, vaginal bleeding, water breaking (ruptured membranes) or infection
Tests and procedures to help diagnose an incompetent cervix during the second trimester include:
- Transvaginal ultrasound. Your doctor may use transvaginal ultrasound to evaluate the length of your cervix and to check if membranes are protruding through the cervix. During this type of ultrasound, a slender transducer is placed in your vagina to send out sound waves that generate images on a monitor.
- Pelvic exam. Your doctor will examine your cervix to see if the amniotic sac has begun to protrude through the opening (prolapsed fetal membranes). If the fetal membranes are in your cervical canal or vagina, this indicates cervical insufficiency. Your doctor will also check for contractions and, if necessary, monitor them.
- Lab tests. If fetal membranes are visible and an ultrasound shows signs of inflammation but you don't have symptoms of an infection, your doctor might test a sample of amniotic fluid (amniocentesis) to diagnose or rule out an infection of the amniotic sac and fluid (chorioamnionitis).
There aren't any tests that can be done before pregnancy to reliably predict an incompetent cervix. However, certain tests done before pregnancy, such as an MRI or an ultrasound, can help detect uterine abnormalities that might cause an incompetent cervix.
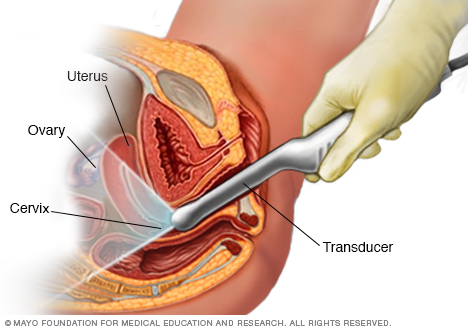
During a transvaginal ultrasound, your care provider or a medical technician inserts a wandlike device (transducer) into your vagina while you lie on your back on an exam table. The transducer emits sound waves that generate images of your pelvic organs.
Treatment
Treatments for or approaches to managing an incompetent cervix might include:
- Progesterone supplementation. If you have a history of premature birth, your doctor might suggest weekly shots of a form of the hormone progesterone called hydroxyprogesterone caproate (Makena) during your second and third trimester. However, further research is needed to determine the best use of progesterone in cervical insufficiency.
- Repeated ultrasounds. If you have a history of early premature birth, or you have a history that may increase your risk of cervical insufficiency, your doctor might begin carefully monitoring the length of your cervix by giving you ultrasounds every two weeks from week 16 through week 24 of pregnancy. If your cervix begins to open or becomes shorter than a certain length, your doctor might recommend cervical cerclage.
-
Cervical cerclage. If you are less than 24 weeks pregnant or have a history of early premature birth and an ultrasound shows that your cervix is opening, a surgical procedure known as cervical cerclage might help prevent premature birth. During this procedure, the cervix is stitched closed with strong sutures. The sutures will be removed during the last month of pregnancy or during labor.
If you have a history of premature births that are likely due to cervical insufficiency, your doctor might also recommend cervical cerclage before your cervix begins to open (prophylactic cerclage). This procedure is typically done before week 14 of pregnancy.
Cervical cerclage isn't appropriate for everyone at risk of premature birth. The procedure isn't recommended for women carrying twins or more. Be sure to talk to your doctor about the risks and benefits of cervical cerclage.
Your doctor might also recommend the use of a device that fits inside the vagina and is designed to hold the uterus in place (pessary). A pessary can be used to help lessen pressure on the cervix. However, further research is needed to determine if a pessary is an effective treatment for cervical insufficiency.

In a cervical cerclage, strong stiches (sutures) are used to close the cervix during pregnancy to help prevent premature birth. Typically, the stitches are removed during the last month of pregnancy.
Lifestyle and home remedies
If you have an incompetent cervix, your doctor might recommend restricting sexual activity or limiting certain physical activities.
Coping and support
It can be difficult to learn that you have an incompetent cervix. It may make you feel anxious about your pregnancy and afraid to think about the future. Ask your doctor for suggestions on safe ways to relax.
If you give birth prematurely, you might also feel that you did something to cause the premature birth or that you could have done more to prevent it. If you're experiencing feelings of guilt, talk to your partner and loved ones, as well as your doctor. Try to focus your energy on caring for and getting to know your child.
Preparing for an appointment
If you're pregnant and have any risk factors for an incompetent cervix or you experience any symptoms during your second trimester that indicate you might have an incompetent cervix, consult your doctor right away. Depending on the circumstances, you might need immediate medical care.
Here's some information to help you get ready for your appointment, as well as what to expect from your doctor.
What you can do
Before your appointment, you might want to:
- Ask about pre-appointment restrictions. In most cases you'll be seen immediately. If that's not the case, ask whether you should restrict your activities while you wait for your appointment.
- Find a loved one or friend who can join you for your appointment. Fear and anxiety might make it difficult to focus on what your doctor says. Take someone along who can help remember all the information.
- Write down questions to ask your doctor. That way, you won't forget anything important that you want to ask, and you can make the most of your time with your doctor.
Below are some basic questions to ask your doctor about an incompetent cervix. If any additional questions occur to you during your visit, don't hesitate to ask.
- Has my cervix begun to open? If so, how much?
- Is there anything I can do to help prolong my pregnancy?
- Are there any treatments that can prolong my pregnancy or help the baby?
- Do I need to be on bed rest? If so, for how long? What kinds of activities will I be able to do? Will I need to be in the hospital?
- What signs or symptoms should prompt me to call you?
- What signs or symptoms should prompt me to go to the hospital?
- What will happen to my baby if he or she is born now? What can I expect?
What to expect from your doctor
Your doctor is likely to ask you a number of questions, including:
- When did you first notice your signs or symptoms?
- Have you had any contractions or changes in vaginal discharge?
- Have you had any previous pregnancies, miscarriages or cervical surgeries that I'm not aware of?
- How long would it take you to get to the hospital in an emergency, including time to arrange any necessary child care, transportation and so on?
- Do you have friends or loved ones nearby who could care for you if you need bed rest?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.