Intestinal ischemia (is-KEE-me-uh) describes a variety of conditions that occur when blood flow to your intestines decreases. Ischemia can be due to a fully or partially blocked blood vessel, usually an artery, or low blood pressure leading to an overall reduced blood flow. Intestinal ischemia can affect your small intestine, your large intestine (colon) or both.
The decreased blood flow doesn't provide enough oxygen for the cells in your digestive system. Intestinal ischemia is a serious condition that can cause pain and make it difficult for your intestines to work properly. In severe cases, loss of blood flow to the intestines can damage intestinal tissue and possibly lead to death.
Treatments are available for intestinal ischemia. To improve the chances of recovery, it's crucial to recognize the early symptoms and get medical help right away.
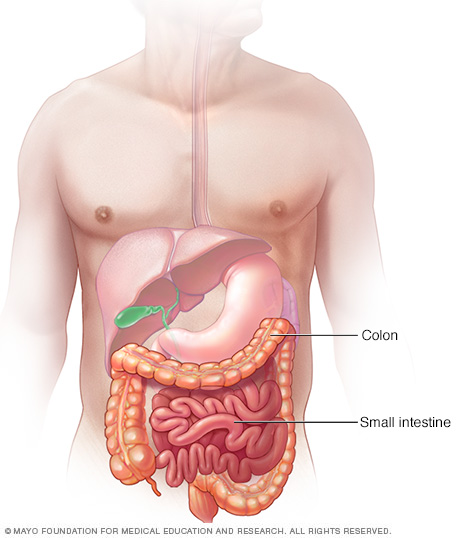
The small intestine and colon are parts of your digestive tract, which processes the foods you eat. The intestines take nutrients from the foods. What isn't absorbed by the intestines continues along the digestive tract and is passed as stool during a bowel movement.
Symptoms
Signs and symptoms of intestinal ischemia can develop suddenly (acute) or gradually (chronic). Signs and symptoms may be different from one person to the next, but there are some generally recognized patterns that suggest intestinal ischemia.
Symptoms of sudden (acute) intestinal ischemia
Signs and symptoms of acute intestinal ischemia typically include:
- Sudden belly (abdominal) pain that may be mild, moderate or severe
- An urgent need to have a bowel movement
- Frequent, forceful bowel movements
- Abdominal tenderness or bloating (distention)
- Blood in your stool
- Nausea and vomiting
- Mental confusion in older adults
Symptoms of gradually developing (chronic) intestinal ischemia
Signs and symptoms of chronic intestinal ischemia can include:
- Abdominal cramps or fullness, usually within 30 minutes after eating, and lasting 1 to 3 hours
- Abdominal pain that gets gradually worse over weeks or months
- Fear of eating because of pain that happens after eating
- Unintended weight loss
- Diarrhea
- Nausea and vomiting
- Bloating
When to see a doctor
Seek immediate medical care if you have sudden, severe abdominal pain. Pain that makes you so uncomfortable that you can't sit still or find a comfortable position is a medical emergency.
If you have other signs or symptoms that worry you, make an appointment with your health care provider.
Causes
Intestinal ischemia occurs when the blood flow through the major blood vessels that supply blood to (arteries) and from (veins) your intestines slows or stops. The condition has many possible causes. These can include:
- Blockage in an artery caused by a blood clot
- Narrowing of an artery due to buildup of fatty deposits, such as cholesterol (atherosclerosis)
- Low blood pressure leading to an overall reduced blood flow
- Blockage in a vein, less commonly
Intestinal ischemia is often divided into categories. Colon ischemia (ischemic colitis) affects the large intestine. Types of ischemia that affect the small intestine include acute mesenteric ischemia, chronic mesenteric ischemia and ischemia due to mesenteric venous thrombosis.
Colon ischemia (ischemic colitis)
This type of intestinal ischemia, which is the most common, occurs when blood flow to part of the colon is slowed or blocked. The cause of reduced blood flow to the colon isn't always clear, but a number of conditions can put you at risk of colon ischemia:
- Dangerously low blood pressure (hypotension) related to dehydration, heart failure, major surgery, trauma or shock
- A blood clot or severe atherosclerosis in an artery supplying the colon
- Twisting of the bowel (volvulus) or trapping of intestinal contents within a hernia
- Excessive bowel enlargement from bowel blockage caused by scar tissue or a tumor
- Other medical disorders that affect your blood, such as inflammation of your blood vessels (vasculitis), lupus or sickle cell anemia
- Medications that narrow (constrict) blood vessels, such as some used to treat heart disease and migraine
- Hormonal medications, such as birth control pills
- Cocaine or methamphetamine use
- Vigorous exercise, such as long-distance running
Acute mesenteric ischemia
Mesenteric ischemia occurs when narrowed or blocked arteries restrict blood flow to your small intestine. Decreased blood flow can permanently damage the small intestine.
Acute mesenteric ischemia is the result of a sudden loss of blood flow to the small intestine. It may be due to:
- A blood clot (embolus) that comes loose from your heart and travels through your bloodstream to block an artery. It usually blocks the superior mesenteric artery, which supplies oxygen-rich blood to your intestines. This is the most common cause of acute mesenteric artery ischemia. This type can be brought on by congestive heart failure, an irregular heartbeat (arrhythmia) or a heart attack.
- A blockage that develops within one of the main intestinal arteries and slows or stops blood flow. This often is a result of atherosclerosis. This type of sudden ischemia tends to occur in people with chronic intestinal ischemia.
- Impaired blood flow resulting from low blood pressure due to shock, heart failure, certain medications or chronic kidney failure. This is more common in people who have other serious illnesses and who have some degree of atherosclerosis. This type of acute mesenteric ischemia is often referred to as nonocclusive ischemia, which means that it's not due to a blockage in the artery.
Chronic mesenteric ischemia
Chronic mesenteric ischemia results from the buildup of fatty deposits on an artery wall (atherosclerosis). The disease process is generally gradual. It's also known as intestinal angina because it results in decreased blood flow to the intestines after eating. You may not require treatment until at least two of the three major arteries supplying your intestines become severely narrowed or completely blocked.
A possibly dangerous complication of chronic mesenteric ischemia is developing a blood clot within a narrowed artery. This can cause blood flow to be suddenly blocked, resulting in acute mesenteric ischemia.
Ischemia due to mesenteric venous thrombosis
This ischemia occurs when blood can't leave your small intestines. A blood clot can develop in a vein draining blood from your intestines. Veins carry blood that has had the oxygen removed back to the heart. When the vein is blocked, blood backs up in the intestines, causing swelling and bleeding. This may result from:
- Acute or chronic irritation and swelling (inflammation) of your pancreas (pancreatitis)
- Infection inside your belly (abdominal infection)
- Cancers of the digestive system
- Bowel diseases, such as ulcerative colitis, Crohn's disease or diverticulitis
- Disorders that make your blood more prone to clotting (hypercoagulation disorders), such as an inherited clotting disorder
- Medications such as estrogen that can increase clotting risk
- Abdominal injuries
Risk factors
Factors that may increase your risk of intestinal ischemia include:
- Buildup of fatty deposits in your arteries (atherosclerosis). If you've had other conditions caused by atherosclerosis you have an increased risk of intestinal ischemia. These conditions include decreased blood flow to your heart (coronary artery disease), legs (peripheral vascular disease) or the arteries supplying your brain (carotid artery disease).
- Age. People older than 50 are more likely to develop intestinal ischemia.
- Smoking. Cigarettes and other forms of smoked tobacco increase your risk of intestinal ischemia.
- Heart and blood vessel problems. Your risk of intestinal ischemia is increased if you have congestive heart failure or an irregular heartbeat such as atrial fibrillation. Blood vessel diseases that result in irritation and inflammation of veins and arteries (vasculitis) may also increase risk.
- Medications. Certain medications may increase your risk of intestinal ischemia. Examples include birth control pills and medications that cause your blood vessels to expand or contract, such as some allergy medications and migraine medications.
- Blood-clotting problems. Diseases and conditions that increase your risk of blood clots may increase your risk of intestinal ischemia. Examples include sickle cell anemia and the Factor V Leiden mutation.
- Other health conditions. For example, having high blood pressure, diabetes or high cholesterol can increase the risk of intestinal ischemia.
- Recreational drug use. Cocaine and methamphetamine use have been linked to intestinal ischemia.
Complications
Complications of intestinal ischemia can include:
- Death of intestinal tissue. If blood flow to your intestine is completely and suddenly blocked, intestinal tissue can die (gangrene).
- A hole through the wall of the intestines (perforation). A perforation can develop, which can cause the contents of the intestine to leak into the abdominal cavity. This may cause a serious infection (peritonitis).
- Scarring or narrowing of your intestine. Sometimes the intestines can recover from ischemia, but as part of the healing process the body forms scar tissue that narrows or blocks the intestines. This occurs most often in the colon. Rarely this happens in the small intestines.
Other health conditions, such as chronic obstructive pulmonary disease (COPD), can worsen the severity of intestinal ischemia. Emphysema, a type of COPD, and other smoking-related lung diseases increase this risk.
In some cases, intestinal ischemia can result in death.
Diagnosis
If after a physical exam your health care provider suspects intestinal ischemia, you may undergo several diagnostic tests. The choice of tests is based on your signs and symptoms and can include:
- Blood tests. Although there are no specific blood tests to indicate intestinal ischemia, certain general blood test results might suggest intestinal ischemia. An example of such a result is an increase in white cell count.
- Imaging tests. Imaging tests may help your health care provider see your internal organs and rule out other causes for your signs and symptoms. Imaging tests may include an X-ray, ultrasound, CT scan or MRI. To look at the blood flow in your veins and arteries you may have an angiogram using a specific type of CT scan or MRI or a catheter-directed angiogram done by an interventional radiologist.
- A scope to see inside your digestive tract. This technique involves inserting a lighted, flexible tube with a camera on its tip into your rectum to view your digestive tract from the inside. This is helpful when ischemia of the large intestine is suspected. When inserted in your rectum, the scope examines the last 2 feet of your colon (sigmoidoscopy) or your entire colon (colonoscopy).
- Dye that tracks blood flow through the arteries. During this test (angiography), a long, thin tube (catheter) is inserted into an artery in your groin or arm. The catheter is then passed to the largest artery in your body (aorta). A dye injected through the catheter flows directly to your intestinal arteries. As the dye moves through your arteries, narrowed areas or a blockage is visible on X-ray images. Angiography also allows the health care provider to treat a blockage in an artery by removing a clot, injecting medication or using special tools to widen an artery.
- Surgery. In some cases, you may need surgery to find and remove damaged tissue. Opening the abdomen allows diagnosis and treatment during one procedure.
Treatment
Treatment of intestinal ischemia involves restoring the blood supply to your digestive tract. Options vary depending on the cause and severity of your condition.
Colon ischemia
If there is evidence of severe colonic ischemia, your health care provider may recommend antibiotics to treat or prevent infections. Treating any underlying medical condition, such as congestive heart failure or an irregular heartbeat, is also important.
You'll likely need to stop medications that constrict your blood vessels, such as migraine drugs, hormone medications and some heart drugs. In most cases, colon ischemia heals on its own.
If your colon has been severely damaged, you may need surgery to remove the dead tissue. In some cases, you may need surgery to bypass a blockage in one of your intestinal arteries. If angiography is done to diagnose the problem, it may be possible to open up a narrowed artery with angioplasty.
Angioplasty involves using a balloon inflated at the end of a catheter to compress the fatty deposits and stretch the artery, making a wider path for the blood to flow. A spring-like metallic tube (stent) also may be placed in your artery to help keep it open. A blood clot may be removed or be treated with medication to dissolve the clot.
Acute mesenteric artery ischemia
Surgery may be necessary to remove a blood clot, to bypass an artery blockage, or to repair or remove a damaged section of intestine. Treatment also may include antibiotics and medications to prevent clots from forming, dissolve clots or dilate blood vessels.
If angiography is done to diagnose the problem, it may be possible to remove a blood clot or to open up a narrowed artery with angioplasty at the same time. A stent also may be placed in your artery to help keep it open.
Chronic mesenteric artery ischemia
Treatment requires restoring blood flow to your intestine. Your surgeon can bypass the blocked arteries or widen narrowed arteries with angioplasty or by placing a stent in the artery.
Ischemia due to mesenteric venous thrombosis
If your intestine shows no signs of damage, you'll likely need to take anticoagulant medication for about 3 to 6 months. Anticoagulants help prevent clots from forming.
You might need a procedure to remove the clot. If parts of your intestine show signs of damage, you might need surgery to remove the damaged section. If tests show you have a blood-clotting disorder, you may need to take anticoagulants for the rest of your life.
Preparing for an appointment
Go the emergency room if you have severe abdominal pain that makes you so uncomfortable that you can't sit still. You may be referred for immediate evaluation to diagnose and treat your condition, possibly with surgery.
If your abdominal pain is moderate and predictable — for example, it always begins soon after eating — call your health care provider for an appointment. When you call to set up an appointment, you may be referred to a specialist, such as a gastroenterologist or vascular surgeon.
Here's some information to help you get ready for your appointment.
What you can do
- Ask about pre-appointment restrictions. When you make your appointment, ask if there's anything you need to do in advance, such as restrict your diet. It's likely your health care provider will ask you not to eat after midnight the night before your appointment.
- Make a list of your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Make a list of other medical conditions, such as a blood clot, or procedures you've had.
- Make a list of all medications, vitamins, herbs and other supplements you take and the dosages. If you take birth control pills, note the drug's name.
- Take a family member or friend along, if you choose. Someone who accompanies you can help you remember what your provider says.
- Make a list of questions to ask your health care provider.
For intestinal ischemia, some questions to ask include:
- What's the most likely cause of my condition?
- Do you think my condition is temporary or will it be long lasting?
- What tests do I need?
- What treatments are available, and what do you recommend?
- If I need surgery, what will my recovery be like? How long will I be in the hospital?
- How will my diet and lifestyle need to change after surgery?
- What follow-up care and treatments will I need?
- Should I see a specialist?
- Is there a generic alternative to the medicine you're prescribing?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don't hesitate to ask other questions that may occur to you during your appointment.
What to expect from your doctor
Your health care provider may ask:
- When did your symptoms begin?
- Have your symptoms stayed the same or gotten worse?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- How soon after eating do your symptoms begin?
- Do you tolerate small meals better than large ones?
- Are liquids easier to tolerate than solids?
- Does anything improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Do you or did you smoke? How much?
- Have you lost weight?
Copyright © 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.