A liver hemangioma (he-man-jee-O-muh) is a noncancerous (benign) mass in the liver made up of a tangle of blood vessels. Also known as hepatic hemangiomas or cavernous hemangiomas, these liver masses are common and are estimated to occur in up to 20% of the population.
Most cases of liver hemangiomas are discovered during an imaging study done for some other condition. People who have a liver hemangioma rarely experience signs and symptoms and typically don't need treatment.
It may be unsettling to know you have a mass in your liver, even if it's a benign mass. However, there's no evidence that an untreated liver hemangioma can lead to liver cancer.
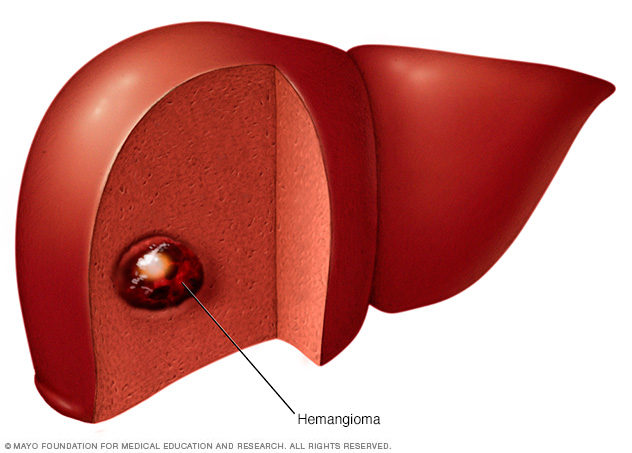
A liver hemangioma is a noncancerous (benign) mass in the liver. A liver hemangioma is made up of a tangle of blood vessels.
Symptoms
In most cases, a liver hemangioma doesn't cause any signs or symptoms.
When a liver hemangioma causes signs and symptoms, they may include:
- Pain in the upper right abdomen
- Feeling full after eating only a small amount of food (early satiety)
- Nausea
- Vomiting
However, these symptoms are nonspecific and in most instances are due to something else even if you have a liver hemangioma, as these tend to be asymptomatic.
When to see a doctor
Make an appointment with your doctor if you experience any persistent signs and symptoms that worry you.

The liver is your largest internal organ. About the size of a football, it's located mainly in the upper right portion of your abdomen — beneath the diaphragm and above your stomach. A small portion extends into the upper left quadrant.
Causes
It's not clear what causes a liver hemangioma to form. Doctors believe liver hemangiomas are present at birth (congenital).
A liver hemangioma usually occurs as a single abnormal collection of blood vessels that is less than about 1.5 inches (about 4 centimeters) wide. Occasionally liver hemangiomas can be larger or occur in multiples. Large hemangiomas can occur in young children, but this is rare.
In most people, a liver hemangioma will never grow and never cause any signs and symptoms. But in a small number of people, a liver hemangioma will grow to cause symptoms and require treatment. It's not clear why this happens.
Risk factors
Factors that can increase the risk that a liver hemangioma will be diagnosed include:
- Your age. A liver hemangioma can be diagnosed at any age, but it's most commonly diagnosed in people ages 30 to 50.
- Your sex. Women are more likely to be diagnosed with a liver hemangioma than are men.
- Pregnancy. Women who have been pregnant are more likely to be diagnosed with a liver hemangioma than women who have never been pregnant. It's believed the hormone estrogen, which rises during pregnancy, may play a role in liver hemangioma growth.
- Hormone replacement therapy. Women who use hormone replacement therapy for menopausal symptoms may be more likely to be diagnosed with a liver hemangioma than women who do not.
Complications
Women who have been diagnosed with liver hemangiomas face a risk of complications if they become pregnant. The female hormone estrogen, which increases during pregnancy, is believed to cause some liver hemangiomas to grow larger.
Very rarely, a growing hemangioma can cause signs and symptoms that may require treatment, including pain in the upper right quadrant of the abdomen, abdominal bloating or nausea. Having a liver hemangioma doesn't mean you can't become pregnant. However, discussing the possible complications with your doctor can help you make a more informed choice.
Medications that affect hormone levels in your body, such as birth control pills, could cause an increase in size and complications if you've been diagnosed with a liver hemangioma. But this is controversial. If you're considering this type of medication, discuss the benefits and risks with your doctor.
Diagnosis
Tests used to diagnose liver hemangiomas include:
- Ultrasound, an imaging method that uses high-frequency sound waves to produce images of the liver
- Computerized tomography (CT) scanning, which combines a series of X-ray images taken from different angles around your body and uses computer processing to create cross-sectional images (slices) of the liver
- Magnetic resonance imaging (MRI), a technique that uses a magnetic field and radio waves to create detailed images of the liver
- Scintigraphy, a type of nuclear imaging that uses a radioactive tracer material to produce images of the liver
Other tests may be used depending on your situation.
Treatment
If your liver hemangioma is small and doesn't cause any signs or symptoms, you won't need treatment. In most cases a liver hemangioma will never grow and will never cause problems. Your doctor may schedule follow-up exams to check your liver hemangioma periodically for growth if the hemangioma is large.
Liver hemangioma treatment depends on the location and size of the hemangioma, whether you have more than one hemangioma, your overall health, and your preferences.
Treatment options may include:
- Surgery to remove the liver hemangioma. If the hemangioma can be easily separated from the liver, your doctor may recommend surgery to remove the mass.
- Surgery to remove part of the liver, including the hemangioma. In some cases, surgeons may need to remove a portion of your liver along with the hemangioma.
- Procedures to stop blood flow to the hemangioma. Without a blood supply, the hemangioma may stop growing or shrink. Two ways to stop the blood flow are tying off the main artery (hepatic artery ligation) or injecting medication into the artery to block it (arterial embolization). Healthy liver tissue is unharmed because it can draw blood from other nearby vessels.
- Liver transplant surgery. In the unlikely event that you have a large hemangioma or multiple hemangiomas that can't be treated by other means, your doctor may recommend surgery to remove your liver and replace it with a liver from a donor.
- Radiation therapy. Radiation therapy uses powerful energy beams, such as X-rays, to damage the cells of the hemangioma. This treatment is rarely used because of the availability of safer and more-effective treatments.
Preparing for an appointment
Most liver hemangiomas are discovered during a test or procedure for something else. If it's thought that you have a liver mass, you may be referred to a doctor who specializes in the digestive system (gastroenterologist) or one who specializes in the liver (hepatologist).
Here's some information to help you get ready for your appointment and to know what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you're experiencing. Most people with liver hemangiomas don't have any signs or symptoms.
- Make a list of all medications, vitamins and supplements you're taking.
- Take a family member or friend along. It can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something you missed or forgot.
- Write down questions to ask your doctor.
For a liver hemangioma, some basic questions to ask your doctor include:
- What is the size of my liver hemangioma?
- Do I have one liver hemangioma or multiple hemangiomas?
- Is my liver hemangioma growing?
- What additional tests do I need?
- Do I need treatment for my liver hemangioma?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
- Should I plan for a follow-up visit?
- Are there medications that may worsen my hemangioma?
- Are my symptoms from the hemangioma?
Don't hesitate to ask any other questions you have.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, including:
- Have you had pain, nausea, loss of appetite or feelings of fullness after eating little?
- Have you been pregnant?
- Have you used hormone replacement therapy?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.