Male hypogonadism is a condition in which the body doesn't produce enough of the hormone that plays a key role in masculine growth and development during puberty (testosterone) or enough sperm or both.
You can be born with male hypogonadism, or it can develop later in life, often from injury or infection. The effects — and what you can do about them — depend on the cause and at what point in your life male hypogonadism occurs. Some types of male hypogonadism can be treated with testosterone replacement therapy.
Symptoms
Hypogonadism can begin during fetal development, before puberty or during adulthood. Signs and symptoms depend on when the condition develops.
Fetal development
If the body doesn't produce enough testosterone during fetal development, the result may be impaired growth of the external sex organs. Depending on when hypogonadism develops and how much testosterone is present, a child who is genetically male may be born with:
- Female genitals
- Genitals that are neither clearly male nor clearly female (ambiguous genitals)
- Underdeveloped male genitals
Puberty
Male hypogonadism can delay puberty or cause incomplete or lack of normal development. It can hamper:
- Development of muscle mass
- Voice deepening
- Growth of body and facial hair
- Growth of the penis and testicles
And it can cause:
- Excessive growth of the arms and legs in relation to the trunk of the body
- Development of breast tissue (gynecomastia)
Adulthood
In adult males, hypogonadism can alter certain masculine physical characteristics and impair normal reproductive function. Early signs and symptoms might include:
- Decreased sex drive
- Decreased energy
- Depression
Over time, men with hypogonadism can develop:
- Erectile dysfunction
- Infertility
- Decrease in hair growth on the face and body
- Decrease in muscle mass
- Development of breast tissue (gynecomastia)
- Loss of bone mass (osteoporosis)
Severe hypogonadism can also cause mental and emotional changes. As testosterone decreases, some men have symptoms similar to those of menopause in women. These can include:
- Difficulty concentrating
- Hot flashes
When to seek help
See your health care provider if you have symptoms of male hypogonadism. Finding the cause of hypogonadism is an important first step to getting appropriate treatment.
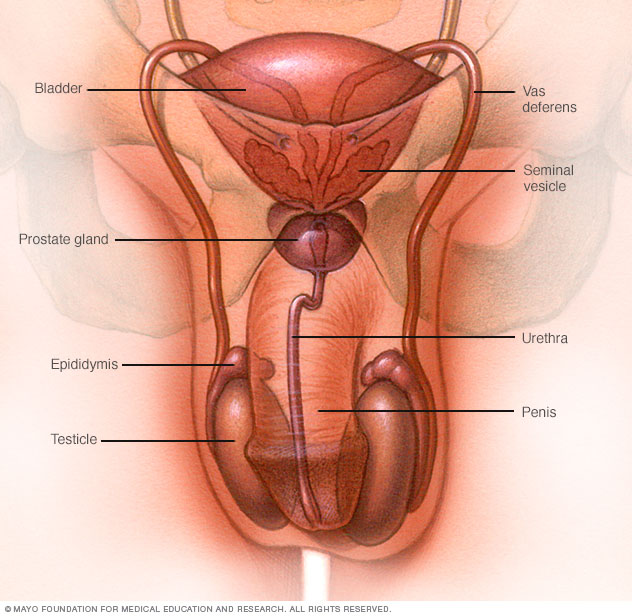
The male reproductive system makes, stores and moves sperm. Testicles produce sperm. Fluid from the seminal vesicles and prostate gland combine with sperm to make semen. The penis ejaculates semen during sexual intercourse.
Causes
Male hypogonadism means the testicles don't produce enough of the male sex hormone testosterone. There are two basic types of hypogonadism:
- Primary. This type of hypogonadism — also known as primary testicular failure — originates from a problem in the testicles.
- Secondary. This type of hypogonadism indicates a problem in the hypothalamus or the pituitary gland — parts of the brain that signal the testicles to produce testosterone. The hypothalamus produces gonadotropin-releasing hormone, which signals the pituitary gland to make follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Luteinizing hormone then signals the testes to produce testosterone.
Either type of hypogonadism can be caused by an inherited (congenital) trait or something that happens later in life (acquired), such as an injury or an infection. At times, primary and secondary hypogonadism occur together.
Primary hypogonadism
Common causes of primary hypogonadism include:
-
Klinefelter syndrome. This condition results from a congenital abnormality of the sex chromosomes, X and Y. A male normally has one X and one Y chromosome. In Klinefelter syndrome, two or more X chromosomes are present in addition to one Y chromosome.
The Y chromosome contains the genetic material that determines the sex of a child and related development. The extra X chromosome that occurs in Klinefelter syndrome causes abnormal development of the testicles, which in turn results in underproduction of testosterone.
-
Undescended testicles. Before birth, the testicles develop inside the abdomen and normally move down into their permanent place in the scrotum. Sometimes one or both of the testicles aren't descended at birth.
This condition often corrects itself within the first few years of life without treatment. If not corrected in early childhood, it can lead to malfunction of the testicles and reduced production of testosterone.
- Mumps orchitis. A mumps infection involving the testicles that occurs during adolescence or adulthood can damage the testicles, affecting the function of the testicles and testosterone production.
- Hemochromatosis. Too much iron in the blood can cause testicular failure or pituitary gland dysfunction, affecting testosterone production.
- Injury to the testicles. Because they're outside the abdomen, the testicles are prone to injury. Damage to both testicles can cause hypogonadism. Damage to one testicle might not impair total testosterone production.
-
Cancer treatment. Chemotherapy or radiation therapy for the treatment of cancer can interfere with testosterone and sperm production. The effects of both treatments often are temporary, but permanent infertility may occur.
Although many men regain their fertility within a few months after treatment, preserving sperm before starting cancer therapy is an option for men.
Secondary hypogonadism
In secondary hypogonadism, the testicles are normal but don't function properly due to a problem with the pituitary or hypothalamus. A number of conditions can cause secondary hypogonadism, including:
- Kallmann's syndrome. This is an abnormal development of the area of the brain that controls the secretion of pituitary hormones (hypothalamus). This abnormality can also affect the ability to smell (anosmia) and cause red-green color blindness.
-
Pituitary disorders. An abnormality in the pituitary gland can impair the release of hormones from the pituitary gland to the testicles, affecting normal testosterone production. A pituitary tumor or other type of brain tumor located near the pituitary gland may cause testosterone or other hormone deficiencies.
Also, treatment for a brain tumor, such as surgery or radiation therapy, can affect the pituitary gland and cause hypogonadism.
- Inflammatory disease. Certain inflammatory diseases, such as sarcoidosis, histiocytosis and tuberculosis, involve the hypothalamus and pituitary gland and can affect testosterone production.
- HIV/AIDS. HIV/AIDS can cause low levels of testosterone by affecting the hypothalamus, the pituitary and the testes.
- Medications. The use of certain drugs, such as opiate pain medications and some hormones, can affect testosterone production.
- Obesity. Being significantly overweight at any age might be linked to hypogonadism.
- Aging. As men age, there's a slow, progressive decrease in testosterone production. The rate varies greatly.

The pituitary gland and the hypothalamus are located within the brain and control hormone production.
Risk factors
Risk factors for hypogonadism include:
- HIV/AIDS
- Previous chemotherapy or radiation therapy
- Aging
- Obesity
- Malnutrition
Hypogonadism can be inherited. If any of these risk factors are in your family health history, tell your doctor.
Complications
The complications of untreated hypogonadism differ depending on when it develops — during fetal development, puberty or adulthood.
Complications might include:
- Abnormal genitalia
- Enlarged male breasts (gynecomastia)
- Infertility
- Erectile dysfunction
- Osteoporosis
- Poor self-image
Diagnosis
Early detection in boys can help prevent problems from delayed puberty. Early diagnosis and treatment in men offer better protection against osteoporosis and other related conditions.
Your health care provider will conduct a physical exam and note whether your sexual development, such as your pubic hair, muscle mass and size of your testes, is consistent with your age.
Your provider will test your blood level of testosterone if you have signs or symptoms of hypogonadism. Because testosterone levels vary and are generally highest in the morning, blood testing is usually done early in the day, before 10 a.m., possibly on more than one day.
If tests confirm that you have low testosterone, further testing can determine if a testicular disorder or a pituitary abnormality is the cause. These studies might include:
- Hormone testing
- Semen analysis
- Pituitary imaging
- Genetic studies
- Testicular biopsy
Treatment
Adult men
Male hypogonadism usually is treated with testosterone replacement to return testosterone levels to normal. Testosterone can help counter the signs and symptoms of male hypogonadism, such as decreased sexual desire, decreased energy, decreased facial and body hair, and loss of muscle mass and bone density.
For older men who have low testosterone and signs and symptoms of hypogonadism due to aging, the benefits of testosterone replacement are less clear.
While you're taking testosterone, the Endocrine Society recommends that your health care provider monitor you for treatment effectiveness and side effects several times during your first year of treatment and yearly after that.
Types of testosterone replacement therapy
Oral testosterone preparations have not been used for treatment of hypogonadism because they can cause serious liver problems. Also, they don't keep testosterone levels steady.
One Food and Drug Administration-approved oral testosterone replacement preparation, testosterone undecanoate (Jatenzo), is absorbed by the lymph system. It might avoid the liver problems seen with other oral forms of testosterone.
Other preparations you might choose, depending on convenience, cost and your insurance coverage, include:
-
Gel. There are several gels and solutions available, with different ways of applying them. Depending on the brand, you rub the testosterone into your skin on your upper arm or shoulder (AndroGel, Testim, Vogelxo) or apply it to the front and inner thigh (Fortesta).
Your body absorbs testosterone through your skin. Don't shower or bathe for several hours after a gel application, to be sure it gets absorbed.
Side effects include skin irritation and the possibility of transferring the medication to another person. Avoid skin-to-skin contact until the gel is completely dry, or cover the area after an application.
-
Injection. Testosterone cypionate (Depo-Testosterone) and testosterone enanthate are given in a muscle or under the skin. Your symptoms might waver between doses depending on the frequency of injections.
You or a family member can learn to give testosterone injections at home. If you're uncomfortable giving yourself injections, member of your care team can give the injections.
Testosterone undecanoate (Aveed) is given by deep intramuscular injection, typically every 10 weeks. It must be given at your provider's office and can have serious side effects.
- Patch. A patch containing testosterone (Androderm) is applied each night to your thighs or torso. A possible side effect is severe skin reaction.
-
Gum and cheek (buccal cavity). A small putty-like substance, gum-and-cheek testosterone replacement delivers testosterone through the natural depression above your top teeth where your gum meets your upper lip (buccal cavity).
This product, taken three times a day, sticks to your gumline and allows testosterone to be absorbed into your bloodstream. It can cause gum irritation.
- Nasal. This testosterone gel (Natesto) can be pumped into the nostrils. This option reduces the risk that medication will be transferred to another person through skin contact. Nasal-delivered testosterone must be applied twice in each nostril, three times daily, which might be more inconvenient than other delivery methods.
- Implantable pellets. Testosterone-containing pellets (Testopel) are surgically implanted under the skin every three to six months. This requires an incision.
Testosterone therapy carries various risks, including:
- Increased production of red blood cells
- Acne
- Enlarged breasts
- Sleep disturbances
- Prostate enlargement
- Limited sperm production
Treatment of infertility due to hypogonadism
If a pituitary problem is the cause, pituitary hormones can be given to stimulate sperm production and restore fertility. A pituitary tumor may require surgical removal, medication, radiation or the replacement of other hormones.
There's often no effective treatment to restore fertility in men with primary hypogonadism, but assisted reproductive technology may be helpful. This technology covers a variety of techniques designed to help couples who have been unable to conceive.
Treatment for boys
Treatment of delayed puberty in boys depends on the underlying cause. Three to six months of testosterone supplementation given as an injection can stimulate puberty and the development of secondary sex characteristics, such as increased muscle mass, beard and pubic hair growth, and growth of the penis.
Coping and support
Having male hypogonadism can affect your self-image and, possibly, your relationships. Talk with your health care provider about how you can reduce the anxiety and stress that often accompany these conditions. Many men benefit from psychological or family counseling.
Find out if there are support groups in your area or online. Support groups put you in touch with other people with similar challenges.
Preparing for an appointment
Although you're likely to start by seeing your family doctor or other care provider, you might be referred to someone who specializes in the hormone-producing glands (endocrinologist).
Here's some information to help you get ready for your appointment.
What you can do
Make a list of:
- Your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment, and when they began
- Key personal information, including any major stresses, recent life changes, and history of childhood illnesses or surgeries
- All medications, vitamins or other supplements you take, including doses
- Questions to ask your provider
For male hypogonadism, some questions to ask your provider include:
- What's the most likely cause of my symptoms?
- Are there other possible causes for my symptoms?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What treatments are available?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your provider
Be prepared to answer questions about your condition, such as:
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- When did you begin puberty? Did it seem to be earlier or later than your peers?
- Did you have any growth problems as a child or adolescent?
- Have you injured your testicles?
- Did you have the mumps as a child or teen? Do you recall if you felt pain in your testicles while you had the mumps?
- Did you have undescended testicles as a baby?
- Did you have surgery for a groin hernia or genital surgery as a child?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.